PICU
Elizabeth C. Parsons
Peter P. Moschovis
Elliot Melendez
General ICU Care Prophylaxis in Critical Illness
Ventilator-Associated PNA
(Am J Infect Control 2006;34:84) See section on VAP
Prevention strategies: Hand washing, HOB >30°, oral chlorhexidine bid (↓ risk in surgical pts), minimize narcotics, avoid unnecessary stress ulcer ppx (does not seem to ↑VAP risk in PICU pts). Neuromusc blockers impair gastric emptying.
Stress Ulcer
(AACN Adv Crit Care 2007;18:158)
Pathophysiology: Stress → splanchnic hypoperfusion → gastric mucosal breakdown and impaired gastric motility, leading to prolonged gastric acid exposure
pH has significant, nonlinear correlation w/ stress ulcer occurrence and bleeding.
pH 7.0 protective, below w/ increased risk.
After bleed, 50% ↓ in clot stability when pH dec from 7.4 to 6.5. (Crit Care Med 2002;30:S351)
Generally during 3rd–7th ICU d; can cause signif bleed (up to 4× inc mortality)
Prophylaxis indicated for high risk: Sepsis, shock, operative procedure ≥3 hr, trauma/closed-head injury, status epilepticus, acute renal or hepatic failure, anticoagulation or coagulopathy, burns >35% BSA, concurrent steroids, enteral feeds (Crit Care Med 1992;20:1519)
Regimens:
Proton pump inhibitors: Preferred
Most potent (dose-depend, 99% achieve pH = 7), max effect not until 48 hr
Risks: CYP450 metabolism, poss assoc w/ C. diff infxn, acute interstitial nephritis
Histamine2-receptor antagonists
Quicker onset of action but less effective. Maximum achievable gastric pH 4.0–5.0. After 24–48 hr, pH stabilizes at 3.0–4.0.
Risk of thrombocytopenia: Use PPI if Plt <50,000; cimetidine inh cytochrome P450
DVT Prophylaxis
(Thrombosis Research 2006;118:3)
See Pulmonary Embolism in Pulmonary section for details on treatment.
Incidence of DVT same as for adults (likely a result of more frequent ppx in adults)
Major ICU risk factor is CVL placement (18%–26% assoc w/ VTE in ICU). Others include prolonged immobility/paralysis (spinal cord injury), malignancy, sepsis, surgery/trauma, long-term TPN (up to 66%).
Dx: US most often used, but has low sensitivity (30%–80%).
In ICU, a neg US does not rule out DVT. If high suspicion, treat until able to confirm w/ contrast CT or venogram (gold standard)
Hypercoag workup recommended for all patients (same incidence as in adults)
Prophy: No consensus due to lack of pediatric studies; extrapolation from adults difficult 2/2 dif in developmental hemostasis (varying levels/response of clotting cascade proteins) & pharmacokinetic/dynamic properties of anticoag agents in children
Methods: TEDs or pneumoboots, rarely LMWH
Pediatric evidence: No benefit of prophy in trauma pts <13 yo (J Trauma 2005;59:1345) or w/ warfarin in pedi-onc pts w/ CVL (Acta Paediatr 2006;95:1053)
Bottom Line: Consider prophylaxis for adult-sized patients w/ significant risk factors (long-term immobilization, CVL, malignancy)
Pain Control and Sedation
Pain and sedation scores should be followed for all pts receiving sedatives or analgesics
Commonly Used Analgesics and Sedatives
| Drug | Onset/peak (IV) | Duration (IV) | Relative Potency (IV) | Starting Dose (IV) |
|---|---|---|---|---|
| Morphine | 20 min | 3–5 hr | 1 | Infant/Child: 0.05 mg/kg/dose. usual 0.1–0.2 mg/kg/dose q2–4h prn (max 15 mg/dose) |
| Dilaudid | 15 min | 5 hr | 7 | Child: 0.015 mg/kg/dose q3–6h prn |
| Fentanyl | Immediate | 30–60 min | 100 | Infants: Intermittent: 3 mcg/kg/dose q2–4h prn. Continuous: 1–2 mcg/kg load → 0.5–1 mcg/kg/hr; titrate upward Children: Intermittent: 1–2 mcg/kg/dose; may repeat at 30–60-min intervals. Continuous: 1–2 mcg/kg load → 1 mcg/kg/hr; titrate upward (usual: 1–3 mcg/kg/hr) |
| Versed | 1–5 min | 2–6 hr | N/A | 0.05 mg/kg IV ×1, repeat q2–3 min (max 0.4–0.6 mg/kg IBW); if vented cont at 0.5–1 mcg/kg/min titrate to effect |
| Ativan | 15–30 min | 8–12 hr | N/A | 0.05 mg/kg IV (also IM) q4–8h, max 2 mg/dose |
| These are suggested doses & do not replace clinical judgment. Follow institutional guidelines where available. | ||||
| Equianalgesic Dosing | ||
|---|---|---|
| Oral (mg) | IV (mg) | |
| Morphine | 30 | 10 |
| Fentanyl | N/A | 0.1 |
| Dilaudid | 7.5 | 1.5 |
| Codeine | 200 | N/A |
| Hydrocodone | 20 | N/A |
Respiratory Failure
Definition: Failure of oxygenation, ventilation, gas exchange or airway protection
Diagnostic eval: ABG (VBG can be used to r/o hypercapnia), CXR (r/o PNA, edema).
Consider CBC (anemia), CT (if suspect PE), ECHO, BNP (if suspect shunt or CHF)
Treatment: Treat underlying cause, NPO (to prevent aspiration)
Hypoxemia: Supplemental O2, consider CPAP or intubation
Hypercapnia: Consider BiPAP or intubation
Hypoxemia (↓ Pao2)
| Cause | A-a gradient | SvO2 | Distinguishing Features | Clinical Scenario |
|---|---|---|---|---|
| Hypoventilation | Normal | Drug o/d (benzo’s) | ||
| O2 delivery/consumption imbalance | High | Low | ↑ demand (stress, infection) ↓ supply (hypoxia, ↓ CO, anemia) | |
| High | High | ↓ demand (poor utilization – late shock)↑ supply (high Fio2) | ||
| True shunt | High | Low/normal | Does not correct w/O2 | R->L intracardiac shunt, AVM, alveolar collapse or filling |
| VQ mismatch | High | Low/normal | Corrects w/O2 | Airway (asthma), alveolar (PNA, CHF), vascular (PE) |
A-a gradient: Alveolar-capillary gas exchange
PAO2 – PaO2 = (FiO2 × 713) – (PaCO2/0.8))
normal value on RA ∼ 2.5 + (0.21 × age (yrs))
normal value on RA ∼ 2.5 + (0.21 × age (yrs))
PAO2 = partial pressure of O2 in alveolus
PaO2 = oxygenation in artery
Most useful in assessing progression of lung disease Pao2/Fio2 ratio (oxygenation index): Measure of severity
Normal >300; ALI: Pao2/Fio2 201–300; ARDS: Pao2/Fio2 ≤200
Hypercapnea (↑Pco2)
| Cause | Pathophysiology | Clinical Scenario |
|---|---|---|
| Central | ↓ resp drive | Metabolic alkalosis, CNS event/infection, sedation (med or toxin related) |
| Pulmonary | Lung/Airway Musculoskeletal * Note: ↑WOB may not be apparent; blood gas helpful. | PNA, asthma, BPD, CF Obesity, kyphosis/scoliosis, pleural effusion. Neuropathy, botulism, myopathy (muscular dystropy, hypophosphatemia) |
| Increased production | Increased CO2 production from inc metabolic rate | Fever, sepsis, excess carb load |
Mechanical Ventilation
Basic Definitions: see Pulmonary Formulae (Appendix)
Noninvasive Methods
CPAP: Continuous PEEP. Useful for hypoxemia (atelectasis, edema, OSA, HMD)
BiPAP: Pt-triggered PIP + CPAP. Useful for hypoventilation (CF, NM disease)
Invasive Methods
Support (PS/VS): Spont breaths assisted to reach goal pressure (P) or volume (V)
No set rate, pt must initiate breaths. Pt determines I time. Less efficient if ETT leak.
Assist/Control (AC): Vent delivers minumum # supported breaths (synch to pt effort) with add’l pt-initiated breaths getting full assist to reach goal P or V w/controlled l time.
Downside: Uncomfortable, dyssynchrony and auto-PEEP (breath stacking)
SIMV: Vent delivers minimum # supported breaths (sync to pt effort) but add’I pt-initiated breaths get no assist. May add PS to assist spont breaths (SIMV + PS)
Downside: Inc resp effort (pt must overcome circuit resistance during spont breaths)
HFOV: Rapid oscillatory breaths given at set frequency (Hz); manipulate MAP and ΔP
Downside: Can easily hypervent. Vent Δ may take longer to equilibrate on blood gas.
Used when conventional ventilation fails.
Initial trials supporting HFOV over conventional vent strategies were done before ARDSNet low TV protocols, which appear to have same mortality. They are likely equal, but HFOV may be easier way to obtain same result. (Crit Care 2005;9:177)
Troubleshooting
Acute desaturation: Think DOPE
Dislodgement (ETT); Obstruction (mucus plug); Pneumothorax; Equipment failure
Oxygenation depends on Mean Airway Pressure (MAP)
Ventilation depends on minute ventilation and dead space
| Vent Type | Parameter to Change | Increase O2 | Decrease CO2 |
|---|---|---|---|
| Conventional | RR | No effect | ↑ |
| Fio2 | ↑ | No effect | |
| PEEP | ↑ | ↓ | |
| PIP | ↑ | ↑ | |
| I-time (should not be 1st line) | ↑ | ↓ | |
| HFOV | MAP | ↑ | |
| DeltaP | ↑ |
Pediatric ECMO/ECLS
Definition
Extracorporeal life support for lung &/or cardiac fxn (see NICU section for details)
| Circuit | Indication | To ↑ O2 | To ↓ CO2 | Considerations | |
|---|---|---|---|---|---|
| V-V | Blood returns to RA/central vein | Resp failure | Inc Fio2 HCT >35; inc flow; inc CO | Inc sweep | Less efficient oxygenation (SaO2 80%–95%), watch for recirculation |
| V-A | Blood returns to aortic arch | Combined cardioresp failure | Carotid/IJ ligation, direct arterial emboli, renal nonpulsatile flow, inaccurate CVP, lower coronary artery O2 supply, high LV afterload, cardiac stun |
Pediatric Indications
Death “imminent” with other treatment and
Reversible lung disease (commonly PNA, burns/inhalation, acute chest, ARDS PPHN)
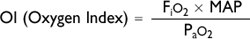
High ventilator support >7 d: PIP >35, PEEP >10, MAP >18, OI >40, Pao2/Fio2>150
No other significant organ dysfunction or
Bridge for cardiac support (CHD postop, myocarditis, arrhythmias, bridge to transplant—must be at a transplant center, postresuscitation care for rapid cooling)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


