CHAPTER 20 scar from previous corpus luteum. a fluid structure formed from the graafian follicle after ovulation; produces progesterone. protrusion within the graafian follicle containing the oocyte. hormone secreted by the follicle, promoting growth of the endometrium. functional or physiological ovulatory cyst consisting of an ovum surrounded by a layer of cells. hormone that stimulates growth and maturation of the graafian follicle(s). mature follicle containing a cumulus mass with a single oocyte. hormone that stimulates ovulation. abnormally heavy or long menses. monthly cyclic changes in the female reproductive system typically 28 days in length. term used to describe pelvic pain preceding ovulation. time between monthly menstrual cycles that exceeds 35 days. explosive release of an ovum from a ruptured graafian follicle. transition period occurring several years before menopause. time between monthly menstrual cycles that is fewer than 21 days. an unusually early onset of puberty. • The onset of menstruation generally occurs between 11 and 13 years of age. • Cessation of menstruation usually occurs around 50 years of age. • The length of a menstrual cycle ranges between 21 and 35 days (average 28 days). • Rupture of a graafian follicle should occur each cycle. • Menstruation depends on the functional integrity of the hypothalamus, pituitary gland, and ovarian axis. • Primarily reflects the activity of the ovaries. • During pregnancy, estradiol levels will steadily rise. • Small amounts are present in the adrenal cortex and arterial walls. • Normal levels 5 to 100 μg/24 h (urine). • Naturally occurring estrogens include estradiol, estriol, and estrone. • Primarily produced by developing follicles and the placenta. • Follicle-stimulating hormone (FSH) and luteinizing hormone (LH) stimulate the production of estrogen in the ovaries. • The breasts, liver, and adrenal glands produce a small amount of estrogen. • Functions include: It promotes formation of female secondary sex characteristics, accelerates growth in height and metabolism, reduces muscle mass, stimulates endometrial growth and proliferation, and increases uterine growth. • Initiates follicular growth and stimulates the maturation of the graafian follicle(s). • Secreted by the anterior pituitary gland. • Levels are normally low in childhood and slightly higher after menopause. • Levels decline in the late follicular phase and demonstrate a slight increase at the end of the luteal phase. • Essential in both males and females for reproduction. • Secreted by the anterior pituitary gland. • Increasing estrogen levels stimulate LH production. • A surge in LH levels triggers ovulation and initiates the conversion of the residual follicle into a corpus luteum. The corpus luteum produces progesterone to prepare the endometrium for possible implantation. • Levels are low in childhood and postmenopause. • Produced in the adrenal glands, corpus luteum, brain, and placenta. • Increasing amounts of progesterone are produced during pregnancy. • Levels are low during the preovulatory phase, increase after ovulation, and remain elevated during the luteal phase. • Functions include: preparing the endometrium for possible implantation or starting the next menstrual cycle. • Endometrial thickness should not exceed 14 mm. • Thickness of the postmenopausal endometrium without hormone replacement therapy should not exceed 8 mm, and it is consistently benign when measuring 5 mm or less. • Fluid within the endometrial cavity is not included in the measurement of the endometrial thickness. • Early pubic hair, breast, or genital development may result from natural early maturation or from several other conditions. • Pubic hair or genital enlargement in boys before 9 years. • Breast development in boys before appearance of pubic hair and testicular enlargement. • Pubic hair before 8 years or breast development in girls before 7 years. • Menstruation in girls before 10 years. • Elevated hormone levels indicate the possible presence of a hypothalamus, gonad, or adrenal gland neoplasm. • Induces early bone maturation and reduces eventual adult height. • Adult shaped uterus; ovarian volume greater than 1 cm3. Menstrual Phase of the Endometrium Proliferation Phase of the Endometrium Secretory Phase of the Endometrium • At birth, each ovary contains approximately 200,000 primary follicles. • Secretion of FSH stimulates follicular development. • Follicles will fill with fluid and secrete increasing amounts of estrogen. • Typically, 5 to 11 follicles will begin to develop, with one reaching maturity each cycle. • 80% of patients will demonstrate a nondominant follicle. • Visualization of a cumulus oophorus indicates follicular maturity, with ovulation typically occurring within 36 hours. • Ovulation is regulated by the hypothalamus within the brain. • LH usually reaches its peak 10 to 12 hours before ovulation. • A surge in LH accompanied by a smaller FSH surge triggers ovulation.
Physiology of the female pelvis
Normal physiology
Laboratory values
Estradiol
Estrogen
Follicle-stimulating hormone (FSH)
Luteinizing hormone (LH)
Progesterone
Endometrium
Premenarche
Precocious puberty
Menarche
DESCRIPTION
SONOGRAPHIC APPEARANCE
Menstruation occurs from days 1- 5
Functional layer undergoes necrosis from a decrease in estrogen and progesterone levels.
Early Phase
Hypoechoic central line during menstruation measuring 4-8 mm
Late Phase
Thin, discrete, hyperechoic line postmenstruation measuring 2-3 mm
DESCRIPTION
SONOGRAPHIC APPEARANCE
Proliferation phase overlaps the postmenstruation phase and occurs from days 6-14
Increasing estrogen levels regenerates the functional layer
Coincides with the follicular phase of the ovary
Early Phase (Fig. 20-2)
Days 6- 9
Thin echogenic endometrium in measuring 4-6 mm
Late Phase (Fig. 20-3)
Days 10-14 (Preovulatory)
A triple-line appearance measuring around 6-10 mm
Thick hypoechoic functional layer and hyperechoic basal layer
DESCRIPTION
SONOGRAPHIC APPEARANCE
Also known as postovulatory or premenstrual phase (Figs. 20-4 and 20-5)
Days 15-28
Functional layer continues to thicken
Progesterone level increase stimulates changes in endometrium
Functional layer appears hyperechoic
Basal layer appears hypoechoic
May demonstrate posterior acoustic enhancement
Greatest thickness in this phase measuring 7-14 mm
Ovaries
DESCRIPTION
SONOGRAPHIC APPEARANCE
Begins at the start of menstruation
Ends at ovulation
Variable length but generally 14 days
FSH stimulates the growth of primary follicles
Between days 5 and 7, a dominant secondary follicle is determined
Dominant follicle will grow 2-3 mm/day
Estrogen levels increase
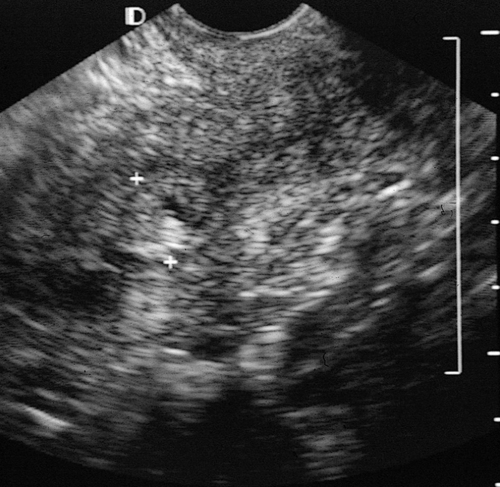
Early Phase—Days 1-5 (
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access