Physical Assessment and Classification
Michael Narvey
Mary Ann Fletcher
The approach to the newborn examination differs in several ways from that of the adult patient. It is imperative that one seizes opportunities as they arise, rather than force an unwilling infant to an assessment based on the examiner’s preferred order. Such forcing often culminates in the infant crying, which although informative may render a complete examination impossible at that time. Instead, during a quiet moment, one may appreciate the heart sounds or the clarity of breath sounds. Similarly during an awake, active period, simple observation may yield a plethora of information regarding the neurologic status of the infant. In the acutely ill infant, delaying the complete examination until such time that the infant may be handled safely is prudent. Inspection, palpation, percussion, and auscultation are all important tools for examination at any age and are incorporated into the neonatal assessment. It is important to provide a thorough systematic assessment of the newborn, but flexibility must be inherent in the approach.
Antenatal ultrasound screening and more recently the evaluation of fetal abnormalities by MRI have provided physicians with the capability of preparing for the delivery of newborns with anticipated problems. For example, antenatal discovery of congenital diaphragmatic hernia allows planned delivery in a tertiary care hospital with neonatal staff present at delivery. Despite improvements in triaging of deliveries, the physical examination at birth remains a critical tool in the management of all newborns. In the above example, assessment of vital signs, work of breathing, color, and the presence of other anomalies at birth determine subsequent management, not just the diagnosis itself. In other cases, significant anomalies may be present but their impact on the newborn not appreciated until examination after birth.
Physical assessment in neonates serves to determine anatomic normality for the first time in a new life and the state of health in someone unable to describe their symptoms. A challenge is to determine which findings will be transient or are merely variations of normal and which are markers of major malformations or syndromes. Most of the clinical descriptions of specific syndromes are made of findings that become typical only after there has been sufficient growth and maturation. An example is the subtlety or absence of obvious findings in aborted fetuses or extremely premature infants with Down syndrome.
Because many of the physical signs of early disease also present as part of the normal physiologic changes occurring at birth or in the newborn period, differentiating the markers of subtle illness from transitional variations is a particular challenge in neonatal physical diagnosis. Additionally, there are unique findings that appear quite dramatic but carry little medical significance. Once the examiner has determined that findings represent a disease process, he or she then has to decide just how sick that infant is, or is likely to become. To that end, there have been devised a number of acuity of illness scores that range from the very simple to complex systems that include physiologic monitoring and laboratory values (1,2,3,4,5). The primary advantage of such scoring systems is in forcing a systematic and quantitative assessment that can be compared among observers and over time. Such scores have been used as indicators of mortality risk (5).
The first neonatal examination occurs immediately after birth in the assigning of Apgar scores at 1 and 5 minutes of age and every 5 minutes thereafter until the total is above 7. The scores summarize encapsulated assessments of the cardiopulmonary and neurologic systems after inspection for color, heart rate, respiratory efforts, tone, and muscle activity and assigning a value of 0, 1, or 2 for each of the five observations. Also part of this first examination is inspection for designation of gender and a cursory inspection for major anomalies. Any obvious abnormality merits more immediate evaluation, but the definitive examination in healthy infants should take place after initial transition and the first bath.
The first complete examination ordinarily occurs within the first 24 hours after birth, but if any portion of an assessment is deferred or abnormal at that time reexamination prior to discharge is warranted. For infants discharged before 48 hours after delivery, an examination should take place within 48 hours of discharge by a health professional competent in newborn assessment (6).
During the first outpatient visit, the physician should fully reevaluate the infant, especially those systems not as easily assessed immediately after birth, e.g., the eyes, and those that undergo the greatest changes during transition, e.g., the cardiovascular and hepatobiliary systems. The areas emphasized with subsequent well-baby examinations include neuromuscular and sensory development, the heart, and the hips, as well as parameters of growth including head circumference, length, and weight.
This chapter is a brief discussion of the steps for assessing the newborn infant and interpreting some of the findings. A thorough textbook on how to perform and interpret the physical examination in neonates is available (7).
NEWBORN HISTORY
It is tempting to start the physical examination of neonates before reviewing the history and available laboratory information of the mother. If a newborn is critically ill, the clinician should initiate therapy for stabilization after a cursory examination and before obtaining the complete history, but too much delay can lead to missed or partial diagnoses. Historic information is just as important for neonates as for any other patient. Even if it is more practical to examine an apparently healthy newborn before obtaining the history, a complete evaluation includes all available information. Knowledge of certain historic details may increase one’s vigilance for signs of drug withdrawal in a baby born to a drug abuser, for instance. A key part is the mother’s pregnancy history as well as her prior medical and social history. Other essential elements include general family history, postnatal history, and information about the placental examination.
Maternal history includes the mother’s age, gravidity, parity, time and type of previous fetal losses, general fertility issues, and premature births and their outcomes; maternal illness before or during pregnancy; extent and location of prenatal care; results of any prenatal laboratory tests, especially those for hepatitis, human immunodeficiency virus (HIV), and sexually transmitted diseases; labor and delivery history including duration, assessments of fetal well-being, anesthesia, and route of delivery, drug, alcohol, and tobacco use; prescription and nonprescription medication use; and her vocation. The general family history includes current or significant past medical illnesses in other family members, including siblings; physical traits or appearance, including birth weights of other siblings; consanguinity; social information, educational levels, and vocations; and ethnic or racial background. Helpful information about the newborn period of siblings includes success in breast-feeding, infections, congenital anomalies, genetic conditions, jaundice, and other concerns. To include the postnatal course as part of the newborn history, the clinician should review events surrounding the birth and response to resuscitation, vital signs, feeding, eliminations, and behavior. If there were any complications or requirement for anything other than routine care, this information is a key part of the total neonatal history.
Placental Information
Often more overlooked than history in evaluating neonates is information about the placenta and the clues it provides about the gestational history. Several features of the placenta and cord can be readily assessed on gross examination by anyone at the time of delivery. The placenta should be examined for size, odor, color, and the number and character of fetal membranes. In the last trimester the ratio of fresh placental weight to infant weight is normally 1:6. There should be a uniform thickness and density throughout. Depressions and adherent clots or changes in firmness on the maternal surface suggest abruption or infarction. The placenta is essentially odorless except for a slight odor of fresh blood. Malodor may indicate the presence of infection although this is controversial.
The color of the fetal surface changes with gestational age (GA), but pallor or plethora suggest aberrations in fetal blood volume or hemoglobin level. Elevated bilirubin in the amniotic fluid stains the placenta bright yellow. Meconium will discolor the fetal surface greenish-brown but so too can old blood. If either meconium passage or bleeding occurred more than 1 day prior to delivery, it can be difficult to differentiate the two by gross examination.
The fetal surface should be examined for cloudiness of fetal membranes, which suggests an inflammatory reaction but not necessarily due to infection. Nodules on the amnion indicate prolonged, extreme oligohydramnios. Fetal pulmonary hypoplasia is highly probable in this setting and is a key finding in renal agenesis. Their presence suggests futility if resuscitation is underway.
In multiple gestations with a single placenta, the dividing membranes should be assessed. Membranes can be teased apart and counted: four layers indicate dichorionic placentation and two layers indicate a monochorionic placenta. With a dichorionic placenta or completely separate placentas and same gender twins, one cannot say if they are identical or fraternal from the placental examination. Monochorionicity has traditionally been viewed as patho-gnomonic for identical twins; however, a recent report refutes this assertion (8). Just as monozygotic twins can have separate placentas, dizygotic twins can have tightly fused placentas that appear to be one mass. If there are any remnants of vessels seen in translucent dividing membranes held to a light, there are four membrane layers. If there is only a transparent membrane with no chorionic remnants, it is likely to contain only amnion.
GESTATIONAL AGE ASSESSMENT
For standard reporting of reproductive health statistics and as a prerequisite to determining normality, all infants should be classified by GA and birth weight (6). Ultrasonography has improved the accuracy of pregnancy dating, but discrepancies in dates, physical appearance, or size require further evaluation. If there has been no prenatal care, physi-cal assessment remains the primary clinical determinant of GA.
GA is noted in completed weeks after the onset of the last menstrual period (LMP). For example, a fetus who is 37 weeks and 2 days is in its 38th week of gestation. A term infant is any infant whose birth occurs from the beginning of the first day of week 38 through the end of the last day of week 42 after the onset of the LMP (i.e., 260 to 294 days of gestation). A preterm infant is one born before 37 completed weeks or at 36 weeks and 6 days (259 days) or less. A postterm infant is one whose birth occurs from the beginning of the first day of week 43 (i.e., after 294 days or at 42 weeks and 1 day or more). Correct classification of GA has assumed great importance when discussing the outcome of preterm infants. GAs should never be rounded up. For example, a preterm infant of 24 weeks and 6 days should be considered and classified as 24, not 25 weeks. Classifying infants born at term, preterm, or postterm helps to establish the level of risk for neonatal morbidity and long-term developmental problems. The terms premature and postmature often are used clinically to connote physical or physiologic findings not always correlating with GA. Postdates is an obstetric term meaning a pregnancy that has continued to any time after the expected date of confinement but is not necessarily postterm.
Assessment Techniques
Estimation of GA by physical examination is possible because there is a predictable pattern of physical changes that occur throughout gestation. The most popular score for GA assessment was originally developed in part by Saint-Anne-Dargassies (9), Amiel-Tison (10), and Dubowitz and associates (11). These systems have been applied to infants with GAs of 22 to 27 weeks despite the fact that no infants below 28 weeks were included in their development. In these very premature infants, the GA was consistently overestimated by up to 2 weeks when compared to reliable ultrasound dates. Conversely, in postterm pregnancies they tended to underestimate the age of postterm infants (12). A further modification by Ballard and associates (13), which included infants with GAs ≥26 weeks, purportedly improved reliability. However, even in infant cohorts of <1,500 g and <2,500 g, the Ballard score similarly yielded a 1- to 2-week error, being greatest at lower birth weights (14,15,16,17). A final modification produced the New Ballard Score (NBS), which claimed to improve the accuracy of age assessment to within 1 week (Fig. 19-1) (18). The strength of this study was inclusion of infants ≥20 weeks, designed to improve accuracy because of larger numbers of extremely premature infants. However a recent study in 24- to 27-week premature infants refuted these findings, showing persistent miscalculation by up to 2 weeks (19). Some have attributed the tendency to overestimate true GA to accelerated neurologic maturity (14,18). It is likely that factors contributing to preterm birth cause stress in the developing fetus and bring about faster neurologic maturation compared to unstressed fetuses in continuing pregnancies. Using last menstrual period (LMP) or early ultrasound as the gold standard, some studies show a closer correlation between physical criteria alone and GA compared to neurologic or total Ballard score. In a multicenter study, infants who were small for their GA had consistent overestimation of their GA. (14).
Due to the inaccuracy of the NBS in extreme prematurity, one must continue to use maternal LMP and early ultrasound as the gold standard for determining GA (see Chapter 12). This becomes imperative when deciding aggressiveness of support in an infant born at 22 to 23 weeks by dates. Despite the aforementioned concerns, the NBS remains the best method available to estimate GA in the presence of uncertain dates.
Other methods for GA assessment have emerged over the years. Prior to gestation of 27 weeks, the cornea is too hazy to permit examination of intraocular structures. The vessels in the anterior vascular capsule of the lens mature in a predictable enough pattern in the last trimester to allow determination of GA with a 2-week margin of error in infants at 28 to 34 weeks of gestation. (20) The exam must be performed within the first 24 to 48 hours of life as the vessels atrophy rapidly after this time. It may prove useful when a neurologic abnormality and uncertain dates render the NBS inadequate. As well, it has been validated in infants who are small for GA, which compromises the accuracy of the NBS (21).
One final technique is the use of changes in skin reflectance during fetal development to determine GA of infants at 24 to 42 weeks of gestation (22). A reflectance spectrophotometer at a wavelength of 837 nm obtains a measurement of skin reflectance independent of melanin, yielding an estimate of GA unaltered by skin color. Initially considered for use in black infants who were thought to be more neurologically mature at birth than other ethnic groups, the requirement for special equipment and discovery that GA assessment tools were not influenced by racial differences likely prevented widespread use of this technique (23).
Accurate estimation of GA requires experience and consideration of the infant’s history and overall condition at the time of scoring; for example, maternal medications or drugs and the infant’s fetal position or sleep state affect the neuromuscular response in a normal infant. Significant hypertonia or hypotonia is particularly powerful in affecting the neuromotor scores but does not affect the physical maturity score. Examination as soon as possible after initial stabilization or by 12 hours increases the accuracy in gestations shorter than 28 weeks (18). The use of NBS is particularly
attractive for neonates who are immature and instrumented because it does not require lifting the infant. Although described here separately from other components of the examination, the steps for assessing GA can be done as part of the general physical examination and can provide information for the neurologic evaluation. The neurologic examination of infants during the first year continues to use a number of these assessment elements (24,25).
attractive for neonates who are immature and instrumented because it does not require lifting the infant. Although described here separately from other components of the examination, the steps for assessing GA can be done as part of the general physical examination and can provide information for the neurologic evaluation. The neurologic examination of infants during the first year continues to use a number of these assessment elements (24,25).
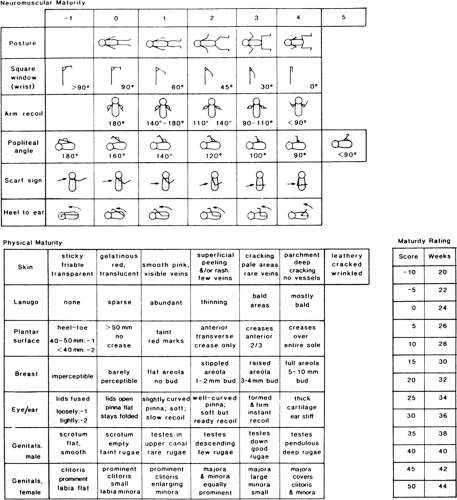 Figure 19-1 Assessment of maturity by the expanded Ballard score (18). |
Neuromuscular Maturity
The resting posture is that observed with the infant in a quiet unrestrained environment. Tone increases in a caudocephalad direction to a pattern of full flexion at term (Fig. 19-1).
The square window is assessed by flexing the wrist and measuring the minimal angle between the palm and flexor surface of the forearm. This angle decreases with advancing
GA. Conditions of marked intrauterine compression, such as severe oligohydramnios, increase wrist flexion. As an extremely premature newborn advances through corrected GA, he or she will not continue to develop as much wrist flexion after birth as the infant would have had he or she stayed in utero.
GA. Conditions of marked intrauterine compression, such as severe oligohydramnios, increase wrist flexion. As an extremely premature newborn advances through corrected GA, he or she will not continue to develop as much wrist flexion after birth as the infant would have had he or she stayed in utero.
The scarf sign indicative of shoulder and superior axial tone is assessed by pulling the hand across the chest to encircle the neck as a scarf and observing the position of the elbow in relation to the midline. There is decreased range and a higher score if there is marked obesity, chest wall edema, an abnormally shortened humerus, or shoulder girdle hypertonicity. Brachial plexus injury or generalized hypotonia produces a spuriously low score.
With the infant supine and head midline, arm recoil is assessed by first flexing the elbow and holding the arm against the forearm for 2 to 5 seconds. The elbow is then fully extended and released with observation of how quickly and fully the infant resumes a flexed posture. Assessing recoil should not be done as part of testing arm traction or with forceful extension because other responses may interfere with a normal reaction. Any pathology affecting the motor strength or tone of the arm will decrease this score.
To determine the popliteal angle, one should first flex the hips with the thighs alongside the abdomen rather than over the front. With the hips held in flexion and the pelvis flat, the knee is then extended as far as possible to estimate the popliteal angle. If an infant was in frank breech presentation with legs extended, the popliteal angles would be greater than expected for age.
In the heel-to-ear maneuver, the legs are held together and pressed as far as possible toward the ears without lifting the pelvis from the table. The angle made by an arc from the back of the heel to the table decreases with maturity.
Physical Maturity
Skin in the most premature infants is gelatinous and almost transparent, allowing the abdominal vessels to be visible. It becomes opaque with maturity as it thickens and keratinizes, eventually shedding the lubricating vernix after it dries and cracks.
Lanugo, which is the fine hair evenly distributed over the body, first emerges at 19 to 20 weeks, but for a few weeks after initial emergence it is not readily apparent. Maximally apparent at 27 to 28 weeks, lanugo sheds first from the areas of greatest contact. Lanugo is distinct from the more pigmented body hair that may be quite prominent in infants of medium to dark complexion.
Assessment of the plantar surface includes measuring the foot because its length reliably corresponds to early GA. With normal muscle activity and uterine compression, creases develop in the sole, progressing from the toes toward the heel. Inappropriate sole creasing is seen in infants with serious neuromotor deficit in the lower extremities (e.g., decreased creasing or only deep vertical creasing) or with oligohydramnios (e.g., increased creasing).
The breast develops with an increase in color, stippling of the areola, and increase in the size of the breast tissue. Although the volume of the breast somewhat depends on fetal nutrition and fat deposition, areolar development with increasing GA is more consistent and independent of these factors.
Ear cartilage becomes firmer with gestation if there is no continuous, extrinsic pressure and the auricular muscles have normal anatomy and activity. Concurrently, as gestation advances, the number of ear folds increase as well. Unfusing of the eyelids can occur over several weeks, and a fused condition by itself is not a sign of extreme, nonviable immaturity. Opening starts by 22 weeks; complete unfusing is evident by at latest 28 weeks (18).
Maturity of the external genitalia is one of the more reliable individual indicators of GA (18). Due to timed descent in the third trimester, testicular progress through the canal into the scrotum is a GA marker. The testes are usually palpable high in the scrotum at 36 weeks and fully descended by 40 weeks. For the scrotum to develop fully into a pendulous, rugose, term appearance, testicular descent must occur at some time, even if the sac is empty at the time of birth.
The appearance of term female genitalia depends on fat deposition and is abnormally immature in a poorly nourished infant. The clitoris approaches term size well before 38 weeks so it is disproportionately large in premature females (26,27). The appearance of a pigmented vertical line, the linea nigra, above the pubis toward the umbilicus suggests a GA of at least 36 weeks.
Influences on Age Assessment Results
If there is a discrepancy between expected and achieved scores, factors that influence the demonstrated findings should be sought before assigning GA.
Resting posture reflects progressive flexion into the position assumed when a term fetus occupies virtually all available intrauterine space and is no longer in a freely floating state. To minimize the volume occupied, this flexion logically progresses in a caudal to cephalic sequence. Compression from oligohydramnios accelerates flexion; it gives an artificially advanced estimate of maturity. Conversely, poor fetal motor activity over a long period spuriously decreases estimated age. Fetuses with markedly decreased motor activity and polyhydramnios have decreased plantar and palmar horizontal creasing and inappropriately immature posturing. Any condition affecting the position or activity of the lower extremities, such as frank breech presentation with hyperextended knees or myelomeningocele with paresis leads to an aberrantly lowered neuromotor score. Similarly, an infant who is hypotonic from illness or sedation has less flexion than normal for true GA.
GROWTH
Measurement Techniques
Infants weighing less than 2,500 g are low birth weight (LBW) regardless of GA; very low birth weight (VLBW)
refers to a weight less than 1,500 g, and extremely low birth weight (ELBW) indicates an infant weighing less than 1,000 g. Classification by these weight groups helps establish the level of risk for neonatal and long-term morbidity and mortality, particularly when the weight classification is coupled with an accurate GA (28).
refers to a weight less than 1,500 g, and extremely low birth weight (ELBW) indicates an infant weighing less than 1,000 g. Classification by these weight groups helps establish the level of risk for neonatal and long-term morbidity and mortality, particularly when the weight classification is coupled with an accurate GA (28).
Of all measurements, crown-heel length is the most subject to variability, because it depends on achieving full extension of an infant who is more naturally in flexion. This measurement is performed with the infant supine, neck neutral, leg fully extended, and ankle flexed to 90 degrees. If there is deviation from an expected norm, the first step in evaluation is to remeasure the infant for confirmation. Although not part of routine practice, a measuring board definitely improves accuracy.
When anomalies of the lower extremities make crown-heel length implausible, the crown-rump measurement may still be feasible. Crown-rump length is measured with the infant supine and the hips flexed 90 degrees. Congenital dwarfism may be classified as those with a short trunk, short legs, or both. These subtypes can be readily differentiated by the crown-rump to total length ratio. From 27 to 41 weeks of gestation the value is fairly consistent at 0.665 ± 0.027 (29). The ratio is normal if a condition causes proportional reductions in length of the upper and lower body; increased if the legs are shortened to a greater degree; and decreased if the trunk is foreshortened. Standards for separate lengths of upper and lower limbs are available (30,31).
The head circumference is the largest dimension around the head obtained with a tape placed snugly above the ears. This is the occipital frontal circumference (OFC). Head circumference undergoes a marked increase during the last trimester, averaging 25 cm at 28 weeks and 35 cm at term (32). The average head circumference is 0.5 cm greater in male compared with female neonates (33). Due to greater reliability of repeated measurements, paper rather than reusable cloth tape measures should be used (34). Minor changes in head circumference occur during the first week after birth as scalp edema and molding resolve. The molding seen after prolonged breech positioning can lead to an OFC that is as much as 2 cm higher than it will be after molding resolves.
The OFC predictably falls on the same percentile curve as the length. If the OFC differs from length by more than one quartile, the cause should be sought because head size in part reflects brain growth. The most frequent reason for a head percentile to exceed that of length is familial. In this situation the head circumference follows a persistently higher but consistent growth curve. In contrast, pathologic macrocephaly tends to cross to higher percentile curves as it progresses. A decreased rate of head growth, manifested by a flat curve or by dropping to a lower percentile, may indicate poor brain growth, atrophy, or premature suture fusion (craniosynostosis [CS]). As OFC may be normal in some forms of CS, the head width index (maximal biparietal diameter divided by the OFC) and head length index (glabella to occipital prominence divided by the OFC) may be more informative (35). For example, a patient with scaphocephaly secondary to sagittal suture closure may have a normal OFC but have an abnormally small width index and excessive length index. Normal ranges for these indices are available (35). The fetal head circumference exceeds the abdominal circumference until 32 weeks. Between 32 and 36 weeks, the two circumferences are equivalent, and after 36 weeks the abdominal circumference normally is greater.
Interpretation of Growth Parameters
Interpretation of growth parameters requires plotting the measurements on percentile charts constructed from a similar race and environmental population. If birth weight falls between the 10th and 90th percentiles for a given GA, the infant is appropriate for gestational age (AGA); if less than the 10th percentile, the infant is small for gestational age (SGA); and if above the 90th percentile, the infant is large for gestational age (LGA). Some literature cites the 3rd and 97th percentiles as outer limits, but for most clinical purposes this broader range underselects for some at-risk infants, particularly in the lower sizes. Accuracy in GA assessment is critical in determining if a weight is appropriate. AGA infants born at term are at lowest risk for problems associated with neonatal mortality and morbidity (28).
Infants are considered symmetric if the three parameters of weight, length, and head circumference fall on the same curve. The infant is asymmetric if the parameters are on different curves, usually with the weight on a curve lower than those of the head circumference or length. If an infant has either a slowing of intrauterine growth rate documented by serial fetal sonography or a presumed slowing by very low weight for length measurements, he or she is classified as having intrauterine growth retardation (IUGR). All infants who fall below the 10th percentile for weight are both SGA and IUGR. Infants above the 10th percentile are AGA but may be IUGR if they did not achieve their expected growth potential. An infant who demonstrates a deceleration in growth from the 50th to the 20th percentile during the last trimester due to maternal hypertension is such an example.
Infants who are SGA, IUGR, or LGA are at risk for perinatal and long-term problems. Several of the problems encountered by LGA infants include the following:
Iatrogenic prematurity due to overestimation of GA by late size estimates
Increased requirement for delivery by cesarean section
Pulmonary hypertension
Shoulder dystocia
Birth injuries
Ecchymoses
Local fat necrosis associated with forceps applications
Cephalohematoma, skull fracture
Brachial plexus injuries
Paralysis of diaphragm
Fracture of clavicle or humerus
Polycythemia
Jaundice
Hyperviscosity syndrome
Seizures
Renal vein thrombosis
Increased total blood volume
Poor feeding
Hypoglycemia
EXAMINATION
Examination Conditions
A routine neonatal examination, normally 5 to 10 minutes, should take place in a quiet, warm environment. The room’s light should be bright enough to detect skin markings and color but not so bright as to discourage open eyes. When an infant is ill, attention to optimizing the environment and recognizing the potential effect of noxious nursery surroundings on his or her state is fundamental.
Even healthy infants do not tolerate handling in extended examinations. The sicker or more immature they are, the less they tolerate manipulation and environmental assaults. For all examinations, the prime consideration must be that no harm should come by the process. In routine care situations, having one or both parents present during an examination allows discussion about physical findings and offers the opportunity to point out behaviors that can help them better understand their infant. They can address directly any questions about history or therapy at that time as well.
General Assessment
The specifics of neonatal examination are discussed in the following sections. Some systems that are discussed in more detail in other chapters are given less emphasis in this chapter than they would merit in an actual examination.
Inspection
Inspection begins before making any physical contact and from enough of a distance to encompass the infant as a whole. An immediate assessment of wellness can come from simply noting the state, color, respiratory effort, posture, and spontaneous activity. Even simple observations of spontaneous movement patterns can suggest future neurologic deficits or well-being (36).
State
Important indicators of infant well-being are the states or levels of arousal the infant achieves throughout the examination and throughout the day as described by the parents or nursing staff. One categorization of states listed here was originally defined by Prechtl and Beintema (37). Modifications have been made but are not clinically important for general assessments (38,39,40,41).
Deep sleep
Light sleep
Awake, light peripheral movements
Awake, large movements, not crying
Awake, crying
During examination, a healthy infant should demonstrate several levels of arousal. The most useful states for assessing an infant are those of light sleep and quiet awake so irritating maneuvers are held until the conclusion of the assessment. What it takes to assist an infant in moving from one state to another or how well he or she does it without assistance is noteworthy. Because the deep sleep that follows a recent feeding may give an appearance of lethargy on arousal, knowing the feeding history and pattern is prerequisite to determining aptness of state.
Newborns spend nearly two-thirds of each day in sleep (42). Each 24-hour period involves cycling between periods of active sleep (AS) and quiet sleep (QS). These periods are also known as rapid eye movement (REM) and non-REM sleep, respectively. During AS, infants demonstrate phasic limb movements, eye movements, and irregular respirations. Breathing is typically rapid and shallow interspersed between periods of more regular respiration (43). In comparison, QS is characterized by regular respirations and the absence of eye and limb movements. As GA increases, the proportion of time spent in QS increases (44). Stress during the perinatal period may alter the proportion of time spent between AS and QS as firstborns and infants born after cesarean section spend more time in AS than babies from subsequent pregnancies or vaginal deliveries (42).
Quieting an infant may require anything from simply stopping the handling to holding and talking to him or her. The amount of time spent in unstimulated crying is normally limited in the first 24 hours but may increase significantly each day thereafter. Excessive crying that requires more than routine consoling, particularly if there are no intervals of quiet alert states, indicates abnormal irritability, but other causes include a proper response to pain or to a cold environment (45,46).
Color
Color assessment includes judging perfusion and skin color for the presence of cyanosis, (see color plate) jaundice, pallor, plethora, or any unusual pigmentation.
Respiratory Effort
The degree of respiratory effort is a primary indicator of how distressed or comfortable a newborn infant is, even if the cause of distress is not pulmonic. The examiner can observe the respiratory rate, depth of excursions, use of accessory muscles with retractions or nasal flare, any emitted sounds (e.g., grunting or wheezing), and crying pattern. Understanding the infant’s pattern of respiratory
effort can suggest a specific illness and direct the examination. As the severity of a condition increases, these distinctions may be lost (Table 19-1).
effort can suggest a specific illness and direct the examination. As the severity of a condition increases, these distinctions may be lost (Table 19-1).
TABLE 19-1 PATTERNS OF NEONATAL RESPIRATORY EFFORTa | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||
Posture
The normal resting postures at different GAs are shown in Fig. 19-1. While observing neck position, the examiner looks for symmetry between the sides and compares the upper and lower extremities. If there is lateral asymmetry and the head is turned to one side, there may be an asymmetric tonic neck reflex with the extremities on the mental side in extension and those on the occipital side in flexion. In that case, the head should be turned to the opposite side to verify that the asymmetry reverses.
If the fetal presentation is nonvertex or unknown or there is asymmetry or deformation, it is helpful to assist the infant in assuming a position reflecting his or her intrauterine attitude. The physician can fold the extremities into the fetal position by applying moderate pressure to a relaxed infant’s feet while gently shaking the infant’s legs and by directing the arms toward the thorax through gentle pressure on the elbows.
Spontaneous Activity
The examiner should observe what the infant does in light sleep and awake states. Does the infant stretch, move all extremities equally, open and close hands, root and start sucking when something touches his or her face, and yawn with great facial expression, or does the infant lie quietly and move only in response to stimulation?
Premature infants spend more time sleeping but should have spontaneous activity and resting postures commensurate with their GA (47). Because they habituate and become disorganized and stressed quickly on handling, inspection before contact in a benign environment is important.
Vital Signs
Temperature
It is unusual for neonates to develop fevers except in response to increased environmental temperature. If an infant’s skin temperature is above 38°C and remains elevated after the environment returns to normal, a rectal temperature should be obtained. Unless the temperature has been elevated for a prolonged time, the rectal temperature is less likely to be affected by environment, and evaluation for infectious or neurologic causes is indicated (48). Recurrent or profound hypothermia also requires additional evaluation.
In a warm environment, overbundling may cause temperature elevation into the febrile range (49). The infant’s postural response to hyperthermia is arm and leg extension, decreased spontaneous activity, and increased sleep duration in order to maximally dissipate heat. Conversely, hypothermic infants assume a flexed posture to conserve heat. During the first week of life, only 30% of infants born at less than 30 weeks are capable of limb extension, but by 2 weeks this number increases to 87% (50). As such, premature infants in the first week of life and hypotonic or myopathic infants are most at risk for temperature instability because they are less capable of altering position to aid heat dissipation or conservation.
Term infants in the first day of life sweat in response to overheating, but not as efficiently as in a child or adult (51). Infants less than 36 weeks, in comparison, are incapable of sweating on the first day but do so by 2 weeks of age (52). Furthermore, the minimal temperatures required to induce sweating are higher in preterm than in term infants. The first site capable of sweating is the forehead with recruitment of other sites happening in a caudal direction. Visible sweating at rest or on feeding in an afebrile infant is abnormal and may indicate distress, typically from cardiac disease.
Respiratory Rate and Heart Rate
The respiratory rate is obtained by looking at the upper abdomen for a full minute. As soon as an infant is touched, the respiratory rate and depth change. The normal respiratory rate is 30 to 60 inspirations per minute in a term infant, with lower rates occurring after the period of cardiopulmonary transition. When awake, some normal infants breathe shallowly and rapidly but are able to slow sufficiently to feed well.
The heart rate is 110 to 160 beats per minute (bpm) in healthy term infants, but it may vary significantly during deep sleep or active awake states. Preterm infants have resting heart rates at the higher end of the normal range. Tachycardia, with a rate persistently greater than 160 bpm, may be a sign of many conditions, including central nervous system (CNS) irritability, congestive heart failure, sepsis, anemia, fever, or hyperthyroidism. Conversely, low resting heart rates may be observed following mild perinatal asphyxia.
Blood Pressure
Measuring blood pressure is not a routine part of vital signs in most newborn nurseries but is used for infants requiring special care and for evaluating coarctation of the aorta. There are wide variations of normal at different GAs (53,54,55,56). The Committee on Fetus and Newborn of the American Academy of Pediatrics states that hypertension should be diagnosed only after three separate measurements (57).
The range of normal blood pressure in neonates depends on the method used for assessment and GA (see Appendix C-1 for blood pressure values). The values obtained by the blanching and flush methods are mean pressures and are lower than those registered by direct intravascular or Doppler monitoring. The flush method for obtaining mean pressure is easier in an active infant and requires only a sphygmomanometer (58). The Doppler methods, although providing diastolic and systolic pressures, require electronic equipment and a quieter patient. Two important elements for obtaining accurate blood pressure are a quiet infant and a properly sized cuff with a width two-thirds the length of the upper arm.
Facies
Assessment of facies includes looking for symmetry, size, shape, and the relations of all parts of the face and how the infant holds or uses them. A seemingly unusual facial appearance dictates analyzing the individual components to decide if the constellation represents malformation, deformation, a syndrome, or merely familial appearance.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


