Phototherapy
For comprehensive reviews of this subject, the reader is referred to the monograph by Jahrig and associates (479), and to a recent chapter by the author (480).
It helps to understand how phototherapy works if we consider that light is an infusion of discrete photons of energy that correspond to the individual molecules of a drug in a conventional medication. Absorption of these photons by bilirubin molecules in the skin leads to the therapeutic effect in much the same way as binding of drug molecules to a receptor has a desired effect. Tables 35-36 to 35-38 list the factors that influence the dose and efficacy of phototherapy and define the radiometric quantities used in assessing the dose.
Terminology
Light Spectrum
The spectrum of light delivered by the phototherapy unit is determined by the type of light source and any filters used. Because of the optical properties of bilirubin and skin, the most effective lights are those with wavelengths that are predominantly in the blue-green spectrum (481).
TABLE 35-36 FACTORS THAT DETERMINE THE DOSE OF PHOTOTHERAPY | |
|---|---|
|
TABLE 35-37 FACTORS THAT AFFECT THE DOSE AND EFFICACY OF PHOTOTHERAPY | ||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||
There is a common misconception that ultraviolet (UV) light is used for phototherapy. None of the light systems described emit any significant amount of UV radiation, and the small amount of UV light that is emitted by fluorescent tubes is in longer wavelengths (>320 nm) than those that cause erythema (479). In any case, almost all UV light produced is absorbed by the glass wall of the fluorescent tube and by the Plexiglas cover of the phototherapy unit.
Irradiance
Irradiance is the radiant power incident on a surface per unit area of the surface.
TABLE 35-38 RADIOMETRIC QUANTITIES USED | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||
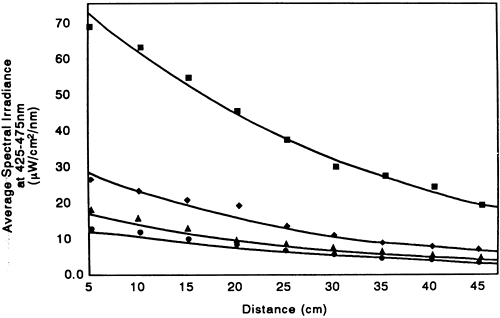
The irradiance in a specific wavelength band is called the spectral irradiance and is expressed as μW/cm2/nm (see Table 35-38). There is a direct relationship between the efficacy of phototherapy and the irradiance used (Fig. 35-26) (482) and the irradiance is directly related to the distance between the light and the infant (Fig. 35-27) (472).
The Dose-Response Relationship of Irradiance
Figure 35-26 shows that there is a direct relationship between the irradiance used and the rate at which the serum bilirubin declines under phototherapy (482). The data in Fig. 35-26 suggest that there is a saturation point
beyond which an increase in the irradiance produces no added efficacy. We do not know, however, that a saturation point exists. As the conversion of bilirubin to excretable photoproducts is partly irreversible and follows first-order kinetics, there may not be a saturation point so we do not know the maximum effective dose of phototherapy.
beyond which an increase in the irradiance produces no added efficacy. We do not know, however, that a saturation point exists. As the conversion of bilirubin to excretable photoproducts is partly irreversible and follows first-order kinetics, there may not be a saturation point so we do not know the maximum effective dose of phototherapy.
 Figure 35-26 Relationship between average spectral irradiance and decrease in serum bilirubin concentration. Full-term infants with nonhemolytic hyperbilirubinemia were exposed to special blue light (Phillips TL 52/20W) of different intensities. Spectral irradiance was measured as the average of readings at the head, trunk, and knees. Drawn from the data of Tan (482). (From Maisels MJ. Why use homeopathic doses of phototherapy? Pediatrics 1996;98:283-287, with permission.) |
Effect on Irradiance of the Light Spectrum and the Distance between the Infant and the Light Source.
Figure 35-27 shows that the light intensity (measured as spectral irradiance) is inversely related to the distance from the source. The relationship between intensity and distance is almost (but not quite) linear, indicating that these data do not obey the law of inverse squares, which states that the light intensity will decrease with the square of the distance (472). This law applies only to a point source of light and the light source in phototherapy units has features of a cylindrical and planar source, not a point source. Figure 35-27 also demonstrates the dramatic difference in irradiance produced within the 425- to 475-nm band by different types of fluorescent tubes.
Spectral Power
This is the product of the skin surface irradiance and the spectral irradiance across this surface area. Because irradiance and the surface area of the infant exposed to phototherapy are key elements in determining the efficacy of phototherapy, the use of spectral power is the only meaningful way to compare the dose of phototherapy received by infants under the different phototherapy systems (472). Calculations of spectral power show why a much more effective dose of phototherapy is delivered to the infant by using the appropriate fluorescent tubes than can be delivered using a fiberoptic phototherapy system (472).
Mechanism of Action
Phototherapy detoxifies bilirubin by converting it to photoproducts that are less lipophilic than bilirubin and can bypass the liver’s conjugating system and be excreted without further metabolism (10). It is not known exactly where the process of phototherapy takes place, but it probably does not take place in the skin cells. It is more likely that it works on bilirubin bound to albumin in the superficial capillaries or in the interstitial space (483).
Bilirubin Photochemistry
When bilirubin absorbs light, photochemical reactions occur. Although many such reactions have been observed in vitro, only three have been shown to occur in vivo during phototherapy.
Configurational(Z → E) Isomerization
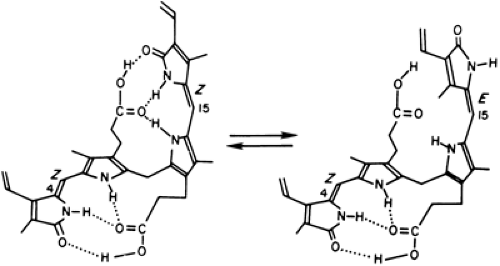
Isomers are substances that have the same molecular formula but different physicochemical properties. There are four possible configurational isomers of bilirubin (Fig. 35-28). In infants receiving phototherapy, the stable 4Z,15Z isomer is converted predominately to the 4Z,15E isomer (Figs. 35-28 and 35-29).(10) The formation of 4Z,15E bilirubin is spontaneously reversible in the dark and occurs rapidly in bile. Thus the 4Z,15E bilirubin formed in the skin and excreted by the liver is readily converted back to ordinary unconjugated bilirubin. The conversion of the 4Z,15Z isomer to the 4Z,15E isomer is also reversible by light (10).
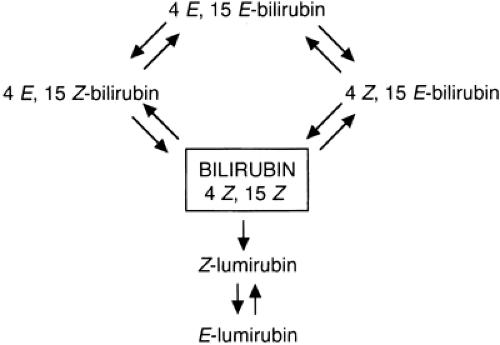 Figure 35-28 Configurational and structural isomers of 4Z, 15Z bilirubin in infants undergoing phototherapy. |
When infants are exposed to phototherapy, photoisomerization occurs almost instantaneously, but the clearance of the light-generated 4Z,15E isomer is very slow (T½∼15 hours). Thus, although configurational isomerization is extremely rapid and accounts for the bulk of the photochemical outcomes, it probably plays only a minor role in lowering the serum bilirubin concentration because “although it is formed fastest, it has nowhere to go” (484).
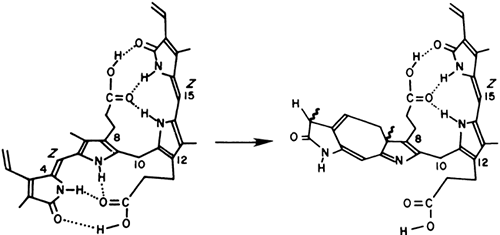
Structural Isomerization
In this reaction (Fig. 35-30), intramolecular cyclization of bilirubin (an irreversible process) occurs in the presence of light to form a substance known as lumirubin that can be excreted in bile (without the need for conjugation) and in urine (but at a much lower rate than in bile) (484). During phototherapy, the serum concentration of lumirubin is about 2% to 6% of the TSB, which is much lower than the concentration of the configurational isomers that form about 20% of the total bilirubin. But, because lumirubin is cleared from the serum much more rapidly than the 4Z,15E isomer, it is likely that lumirubin formation is mainly responsible for the phototherapy-induced decline in serum bilirubin in the human infant (484). It is quite possible, however, that the contribution of the other isomers, 4E,15Z and 4E,15E bilirubin, also is important (485).
Photooxidation
Bilirubin can be photooxidized to water-soluble, colorless products that can be excreted in the urine. This is a slow process and is probably only a minor contributor to the elimination of bilirubin during phototherapy.
Figure 35-31 summarizes the general mechanisms of phototherapy in neonatal jaundice.
Clinical Use and Efficacy of Phototherapy
There are more than 50 published controlled trials of the clinical use of phototherapy (see Maisels (217) for a description and analysis of these studies), confirming that phototherapy is effective in preventing and treating hyperbilirubinemia and dramatically reduces the need for exchange transfusion (217).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree