Rakesh B. Vadhera, MD, FRCA, FFARCS
HEREDITARY NEUROPATHY WITH LIABILITY TO PRESSURE PALSIES
HEREDITARY BRACHIAL PLEXUS NEUROPATHY
LIMB-GIRDLE MUSCULAR DYSTROPHIES
DUCHENNE AND BECKER MUSCULAR DYSTROPHY
POLYMYOSITIS AND DERMATOMYOSITIS (INFLAMMATORY MYOPATHIES)
LUMBAR RADICULOPATHY AND PLEXOPATHY
SCIATIC AND COMMON FIBULAR (PERONEAL) NEUROPATHY
INTRODUCTION
Neuromuscular disorders during pregnancy can be either hereditary or acquired. The physiologic changes of pregnancy may increase the risk of complications from these neuromuscular disorders, sometimes affecting both mother and fetus. Patients may develop compression neuropathies and radiculopathies during pregnancy, labor, and delivery.
Acquired neuropathies can be divided into mononeuropathies (affecting only one nerve), mononeuropathy multiplex (affecting single nerves at different sites of the body), or polyneuropathies (that are diffuse, usually symmetric and generalized). Mononeuropathy is usually caused by compression or trauma of a nerve at a specific site. These peripheral entrapment neuropathies are common during pregnancy and may lead to severe discomfort. Pregnancy itself may predispose patients to some of these entrapment neuropathies, which are mostly benign in their evolution and prognosis and will resolve spontaneously in the postpartum period. Delivery may predispose patients to compression or stretching of some nerves and plexuses that may precipitate symptoms. Prompt clinical evaluation and, when necessary, an electrophysiologic evaluation may aid in the diagnosis and subsequent management. Polyneuropathies are caused by systemic diseases or axonal nerve injuries resulting from metabolic or toxic etiologies or from demyelinating diseases of peripheral nerves.1
Hereditary nerve and muscle disorders may place patients at risk during pregnancy. These patients need additional counseling about the possible transmission of the disease to the fetus.
Table 23-1 summarizes the classification of the most common peripheral neuropathies.
TABLE 23-1 | Peripheral Neuropathies Classification |
CHARCOT-MARIE-TOOTH DISEASE
Charcot-Marie-Tooth (CMT) is a hereditary peripheral neuropathy, also called hereditary motor sensory neuropathy (HMSN) that includes several disorders caused by mutations in various myelin genes that affect its structure, formation, and maintenance. It is a chronic demyelinating disorder of peripheral nerves affecting both motor and sensitive roots.2 Patients usually experience distal leg weakness and distal muscular atrophy, foot deformities, and sensory deficits (Figure 23-1). Deep tendon reflexes can be diminished or absent. Depending on the severity of the disease, it can affect respiratory muscles and thoracic vertebral anatomy, impacting patient respiratory function during pregnancy and affecting delivery and anesthetic care.
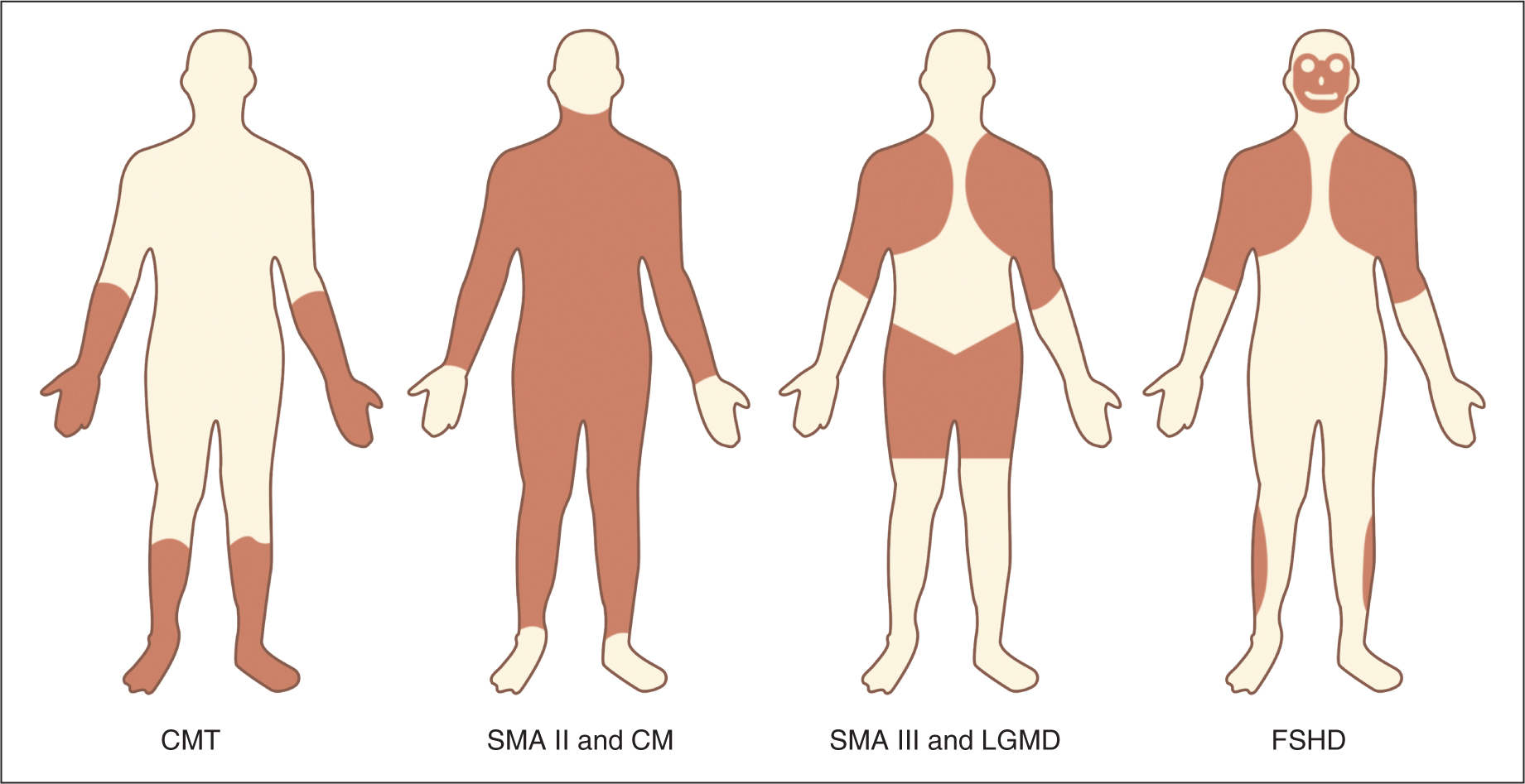
FIGURE 23-1. Distribution of affected muscles and peripheral nerves in different neuropathies. CMT, Charcot-Marie-Tooth disease; LGMD, Limb-girdle muscular dystrophy; FSHD, facioscapulohumeral dystrophy; LGMD, Limb-Girdle Muscular Dystrophy; SMA, spinal muscular atrophy. Reproduced with permission from Awater C, Zerres K, Rudnik-Schöneborn S; Pregnancy course and outcome in women with hereditary neuromuscular disorders: comparison of obstetric risks in 178 patients, Eur J Obstet Gynecol Reprod Biol. 2012 Jun;162(2):153-159.
CMT is classified as types 1 through 7, with more than 40 different mutations identified on over 25 genes, making it a genetically heterogeneous disease with a common phenotype.3 There are many subtypes in each classification based on the inheritance pattern, age of onset, nerve conduction velocity studies, and genes affected.4 The prevalence of CMT1 and 2 is 40 per 100,000 and its incidence is estimated to be 10 to 30 per 100,000.5
The most common form of hereditary neuropathy is CMT1. Its onset is during the first to third decade of life with predominantly motor symptoms such as distal lower extremity weakness accompanied by hyporeflexia. Ambulation is maintained in most cases and patients can expect a normal life expectancy. Peripheral nerves are enlarged and usually palpable. Other symptoms include tremor and gait ataxia. There are several subtypes of CMT and discussion of them is beyond the scope of this chapter.7
Pregnancy Considerations
As the disease progresses, patients develop increased muscle weakness and wasting and sensory loss resulting in progressive morbidity and loss of quality of life.8 During pregnancy about one-fifth of the patients may present with deterioration of their symptoms.9 According to published retrospective studies, symptoms and severity were unchanged during pregnancy in patients with adult onset CMT. In patients with disease presenting earlier in life, these studies reported worsening of symptoms during pregnancy.10,11
In patients with preexisting limitations and symptoms, there is a higher risk of preterm delivery, fetal malpresentation, and risk of worsening of maternal respiratory symptoms that may require increased monitoring. Occasionally, maternal respiratory compromise may lead to intrauterine growth restriction.12 Increased postpartum hemorrhage from uterine atony has been reported in patients with CMT and has been suspected to be secondary to poor innervation of the uterus with subsequent failure to contract postpartum.13
Despite the latter concerns, no significant increase in perinatal mortality has been consistently reported.9,14
Anesthesia Considerations
Extreme care is required in patients with chronic muscle wasting when using muscle relaxants as the response to them is commonly exagerated.15 The use of propofol as an induction agent is preferred over thiopental.16
Secondary to the changes in muscle tone and wasting, there may be spinal abnormalities leading to technical difficulty during neuraxial anesthesia placement. Patients may also develop a respiratory restrictive pattern with poor respiratory function and have increased sensitivity to central nervous system depressant drugs such as opiods.17
The use of regional anesthesia has been reported as a safe alternative for labor analgesia and for cesarean sections when indicated.8,14,18–21 Most reports regarding the use of regional anesthesia either for labor or surgical delivery do not report increased rates of complications except for a delay in resolution of the peripheral block. Avoidance of succinylcholine is recommended to avoid sudden severe hyperkalemic responses.22
HEREDITARY NEUROPATHY WITH LIABILITY TO PRESSURE PALSIES
Patients with hereditary neuropathy with liability to pressure palsies (HNPP) have increased susceptibility to peripheral nerve damage due to mechanical traction or compression. It is inherited as an autosomal dominant disorder with variable penetrance that presents as a generalized demyelinating neuropathy between the second and third decades of life. This disease usually manifests as sudden painless recurrent events of mononeuropathies. Affected nerves include the fibular, ulnar, brachial plexus, radial, and median. Symptoms are commonly elicited by minor traction or trauma and are usually self-limited. About 30% of the patients may have painless brachial plexopathy. The diagnosis is confirmed with sural nerve biopsy and the presence of sausage like thickenings of myelin called tomacula,23 segmental demyelination, and axonal loss.24 The prevalence in the general population is estimated at 16 per 100,000.25 Treatment is supportive.
It is important to differentiate HNPP from hereditary neuralgic amyotrophy (HNA)—see the following text. The latter can cause episodes of painful brachial plexopathy and has been linked to infections during childbirth.26
Pregnancy Considerations
Patients with HNPP may develop neuropathies during pregnancy and delivery from compression and traction,26–28 which may be misdiagnosed as a neuropathy of iatrogenic etiology leading to litigation. A thorough medical history of prior events may be necessary in these patients to reach a diagnosis.
Because of the minimum trauma necessary to produce neuropathies on these patients; it is very important to educate the patient about her condition and the risks during pregnancy and delivery. Care should be taken to avoid trauma or traction of nerves during labor and delivery.
Anesthesia Considerations
Patients should be aware of the increased risk. They have to develop mononeuropathies during pregnancy and delivery, and appropriate counseling is mandatory before performing anesthesia.
HEREDITARY BRACHIAL PLEXUS NEUROPATHY
Hereditary brachial plexus neuropathy (HBPN) is an autosomal dominant disorder characterized by sporadic acute attacks of asymmetrical pain accompanied by weakness, atrophy, and sensory loss across the brachial plexus distribution.13,29 Patients may have patchy multifocal unilateral or bilateral symptoms across shoulder girdle and upper limb area. Biopsies of the affected nerves during attacks show an inflammatory component.
PREGNANCY CONSIDERATIONS
Attacks may be precipitated during pregnancy and in the immediate postpartum period and usually recur during subsequent pregnancies.30 Mode of delivery has not been associated with symptoms and as such should be dictated by obstetrical indications. Pain from attacks may improve with the use of steroids.30 Some retrospective data suggest that the prophylactic use of steroids before delivery and/or surgery in patients with known severe postpartum or postsurgical crisis may prevent or decrease the severity of the attacks by providing immunosuppression.29
FACIOSCAPULOHUMERAL DYSTROPHY
Facioscapulohumeral dystrophy (FSHD) is the third most common muscular dystrophy that is caused by a defect in the double homeobox protein 4 gene (DUX4).31 It is an autosomal dominant disorder of variable penetrance that involves the muscles of facial expression and shoulders (see Figure 23-1). The disease manifests as slowly progressive muscle weakness with variable age of onset from early childhood to the fourth decade of life.
Patients usually remain ambulatory and the progression of the disease is slow, allowing for a near normal life span. Protrusion of the abdomen due to lower abdominal muscle weakness, exaggerated lumbar lordosis, and scapular winging are common features. In rare cases, patients may present dysphagia when jaw and lingual muscles are affected.32 Respiratory muscles are usually spared and less than 1% of patients manifest respiratory insufficiency.33 Other associated symptoms of FSHD are chronic pain (50%-80%), retinal vascular disease with normal visual acuity, and hearing loss in severe cases with early onset.
When patients are aware of their diagnosis, it is important to discuss with them the increased risk for falling and difficulty caring for the newborn after delivery due to an increase in pain and weakness of shoulders and legs. Cardiomyopathy is less common in these patients, but cases of arrhythmias have been described.
Pregnancy Considerations
Patients with FSHD are at increased risk of infections during pregnancy.34 Abdominal and truncal weakness, when present, may prolong the second stage of labor and increase the need for assisted operative vaginal deliveries and cesarean sections.34
About one quarter of patients will experience exacerbation of weakness and pain that may not be alleviated after delivery.34,35 Deterioration that lead to significant handicap during the postpartum period was reported in 12% of patients in another report.9
Anesthesia Considerations
Preoperative electrocardiography (ECG) is necessary to evaluate for conduction abnormalities that may be present in this women. Regional or general anesthesia is considered safe. Monitoring of muscle relaxants may be challenging and peripheral nerve stimulators may need to be placed in the lower extremities to adequately assess the extent of the block.36 All patients with muscular dystrophies are at risk of rhabdomyolysis and care is required before administration of muscle relaxants.
LIMB-GIRDLE MUSCULAR DYSTROPHIES
Limb-girdle muscular dystrophies (LGMD) are a group of diseases with heterogeneous causes that usually affect proximal muscles of the shoulder or pelvic area and girdle weakness is characteristic (see Figure 23-1). They are hereditary diseases with either autosomal dominant or recessive inheritance.37,38
Patients may have cardiac conduction abnormalities and rarely can present with cardiomyopathies. It is important to inquire about cardiac symptoms such as palpitations and syncope throughout pregnancy. In addition, some patients may present with respiratory insufficiency as the disease progresses.
Pregnancy Considerations
Limited data has reported deterioration of the disease during pregnancy in approximately 50% of cases.9
LGMD does not seem to increase the incidence of preterm delivery or miscarriages. Patients with severe symptoms may have increased respiratory compromise that may become significant during the third trimester. Neonatal outcomes are unaffected by the disease. Increased need of operative vaginal deliveries and cesarean sections for fetal malpresentations has been described.9,35
Anesthesia Considerations
Both neuraxial and general anesthesia have been used safely in patients with LGMD.39,40 Patients have increased sensitivity to sedatives and muscle relaxants although few case reports are present in the literature.9,41,42 Patients under general anesthesia are prone to developing cardiac arrhythmias and malignant hyperthermia (MH) like syndrome with rhabdomyolysis. Succinylcholine should be avoided to prevent severe hyperkalemia. Most agree that avoidance of inhaled anesthetics will provide better management and avoid the risks of rhabdomyolysis and MH.41 Induction with propofol may be a safe alternative.41,43,44
MYOTONIC DYSTROPHIES
Myotonic dystrophy (DM) is a multisystemic slowly progressive disease that affects mostly limb, neck, and facial muscles producing weakness with myotonia (slow relaxation of the muscle following a prolonged contraction) and wasting. It progressively affects the central nervous system, the eyes, the heart, and the endocrine system. Patients rarely complain of myalgia and pain. It is currently classified into two subgroups according to their genetic and clinical presentations. Its incidence is approximately 13 per 10,000 and the general prevalence is estimated to be 1 per 8000 in Western Europeans. It is considered to be the most frequently inherited neuromuscular disorder in adults.45 Patients suffering from both subtypes of DM have a reduced life expectancy.13,46
Type 1
Type 1 (DM1), also known as Curschmann-Steinert disease, is inherited as an autosomal dominant disease and caused by an increase of repeats in the dystrophia myotonica-protein kinase (DMPK) gene located on chromosome 19.47,48 It accounts for 98% of cases of DM. It is characterized by muscle weakness and wasting predominantly among cranial muscles (facial, temporalis, masseter, sternocleidomastoid muscles, and vocal cord) and the distal limb musculature.49 Patients may present with periodic myotonia, progressive myopathy, insulin resistance, defects in cardiac conduction, neuropsychiatric symptoms, and cataracts. Males may have testicular atrophy and frontal baldness.50 It has also been associated with mitral valve prolapse. Young patients may present with a first-degree atrioventricular block on ECG before the onset of other symptoms. In addition, it can affect muscles in the gastrointestinal tract, respiratory and cardiac muscle, eyes, and endocrine system.
Pregnancy Considerations
Symptoms of DM1 are usually exacerbated during pregnancy, most significantly during the second and third trimester. Patients also have a higher risk of congestive heart failure (CHF).
Because of the age of onset of the disease, patients usually become pregnant before their diagnosis and may only complain of distal weakness and fatigue.
Patients with DM1 have an increased risk of ectopic pregnancy (up to 4% of gestations), abnormal implantations, and urinary tract infections (UTIs). Maternal complications during pregnancy add to this risk primarily in patients with DM1 and not as significantly in DM2.45,51 In addition, pregnancy increases the incidence of maternal complications, including respiratory infections, cardiac disease, complications during anesthesia, apathy, and sleepiness. All of these can lead to neglect that can affect medical care and social development of the newborn.52 Symptomatic patients also have an increased risk of miscarriage and late spontaneous abortions, preterm labor, preterm delivery, and placental anomalies.45
Patients can experience severe weakness and respiratory compromise when magnesium sulfate is used; even in patients with mild disease.53
During delivery, parturients with DM1 have ineffective uterine contractions with prolonged labors and an increased risk of fetal malpresentations. Poor uterine contractility also increases the risk for postpartum hemorrhage. The congenitally affected fetus may be hypotonic with impaired swallowing which leads to polyhydramnios.
Patients can opt to have prenatal diagnosis with amniocentesis, chorionic villous biopsy or PGD when in vitro fertilization is used to achieve pregnancy. Because it is an autosomal dominant disease, 50% of children will inherit the disorder.
Anesthesia Considerations
Cardiac involvement may include conduction and contractile anomalies. For delivery, regional anesthesia is preferred over GA. Patients with DM1 are very sensitive to induction agents and opiods with prolonged respiratory depression in the postoperative period.54 The risk of postoperative ileus is also increased. Succinylcholine has been used in patients with DM without complications, although when possible it should be avoided (due to risks of myotonic contractions, making intubation difficult and rhabdomyolisis).49 Patients with DM may be at increased risk of MH. Rocuronium for rapid sequence intubation and sugammadex for its reversal have been used successfully where available.55 Patients should be promptly evaluated during pregnancy before delivery. Appropriate testing may include ECG and echocardiography to evaluate for conduction abnormalities, cardiomyopathy, and valvular disease.
Type 2
Myotonic dystrophy type 2 (DM2) is a multisystemic genetic disease with similar manifestations as DM1 but does not have a congenital form.56 Clinical manifestations include myotonia, weakness, generalized pain and stiffness, cardiac conduction abnormalities, and iridescent posterior cataracts.
DM2 has a benign course during pregnancy.51 It usually does not affect anesthetic management or delivery of the patients. DM2 has not been linked to an increased risk of polyhydramnios or stillbirth; likely due to absence of a congenital form of the disease.
DUCHENNE AND BECKER MUSCULAR DYSTROPHY
Although Duchenne muscular dystrophy (DMD) and Becker muscular dystrophy (BMD) are primarily seen in males, because they are recessive X-linked disorders, normal female carriers require prenatal counseling. Patients need to be advised of the risks of transmission and the prenatal diagnosis options available. The incidence is 1 per 3500 live male births for Duchenne’s and 1 per 18,000 in Becker’s muscular dystrophy. The genetic site of the defect is on the short arm of Xp21 region for dystrophin gene protein. Dystrophin protein is present in the body in skeletal muscle, cardiac smooth muscle, and the brain (Figure 23-2).
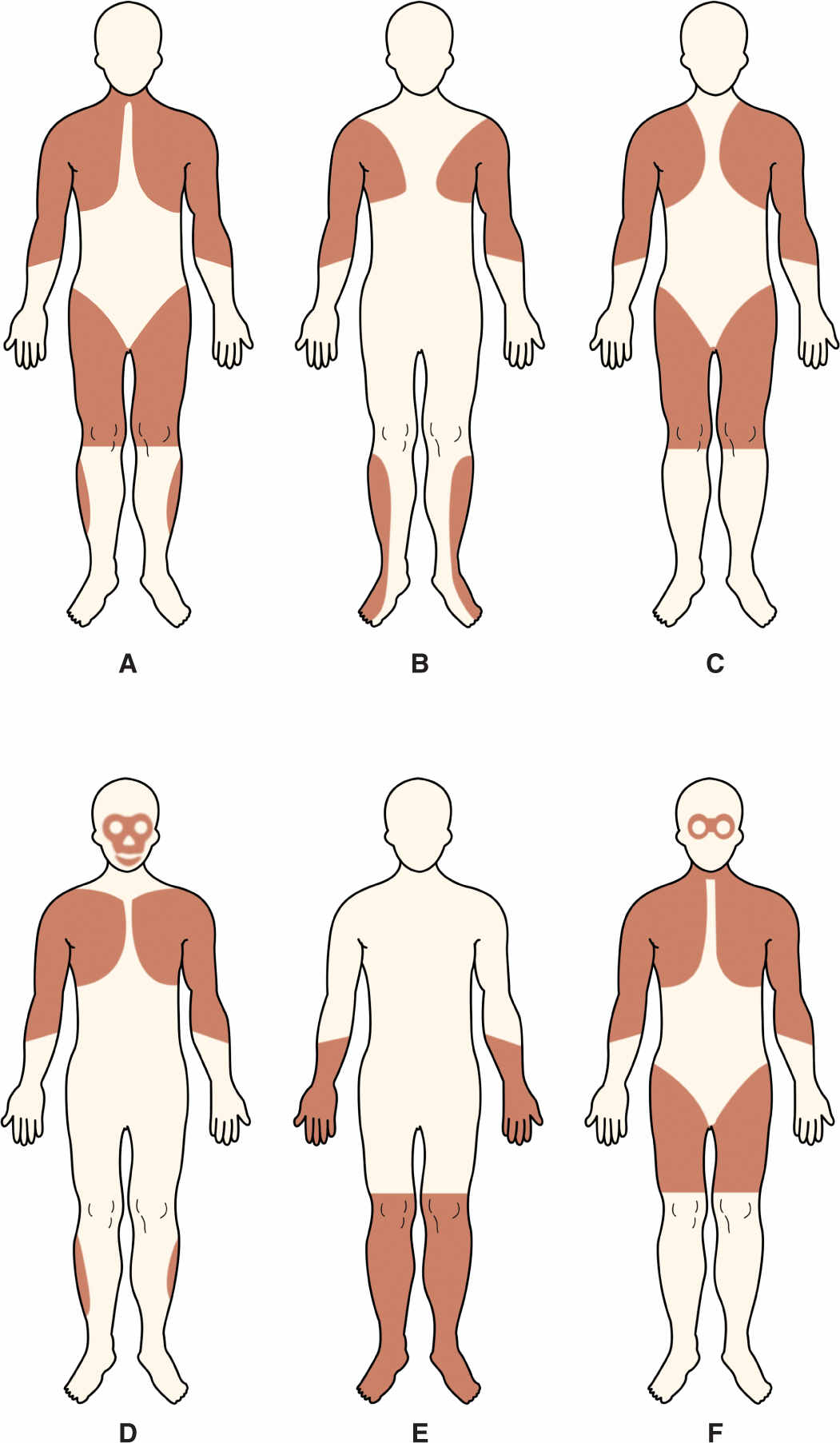
FIGURE 23-2. Distribution of predominant muscle weakness in different types of dystrophy: A, Duchenne type and Becker type; B, Emery-Dreifuss; C, limb girdle; D, facioscapulohumeral; E, distal; and F, oculopharyngeal. Reproduced with permission from Emery AE: The muscular dystrophies, BMJ. 1998 Oct 10;317(7164):991-995.
POLYMYOSITIS AND DERMATOMYOSITIS (INFLAMMATORY MYOPATHIES)
Polymyositis and dermatomyositis are also called idiopathic inflammatory myopathies; they are a group of rare acquired diseases of the muscle of unknown etiology. The disease is rare during pregnancy as the onset of symptoms is usually after childbearing age.13,57 The prevalence is estimated to be 2.4 to 10.7 per 100,000 in the general population but much lower in women during childbearing age.58–60
Polymyositis presents as weakness of limbs, neck, and pharynx primarily. It is believed to be caused by an autoimmune cell-mediated damage to striated muscle.61,62 Dermatomyositis presents as progressive muscle weakness accompanied by a rash on the face, trunk, and extensor surfaces of the extremities. Serologically there is an increase in creatine kinase levels. Vasculitis also may coexist.62–64
Pregnancy Considerations
If the disease is on remission, exacerbations during pregnancy are rare. In patients with active disease, prematurity and intrauterine growth restriction may complicate pregnancy. Exacerbations during pregnancy are commonly treated with corticosteroids.65,66
Steroid treatment during pregnancy may be associated with gestational diabetes, hypertension, osteoporosis, premature rupture of membranes, and higher risk of infections. Use of intravenous immune globulin (IVIG) is an effective alternative in refractory cases.67–69 Similar to other collagen diseases, periconceptional activity is related to exacerbations during pregnancy.13,65,66 With active disease there is a higher risk of preterm delivery, intrauterine growth restriction, stillbirth, and early pregnancy loss.
Route of delivery is dictated by obstetrical reasons. Rarely, patients that deliver vaginally may develop rhabdomyolysis and myoglobinuria in the postpartum period secondary to muscle injury during the delivery process.57,70,71 The risk of postpartum hemorrhage is not increased because dermatomyositis does not affect smooth muscle. Newborns are not at risk for acquiring the disease, although asymptomatic newborns may present with increased CK levels up to 4 months after delivery.13,72
Anesthesia Considerations
Few case reports of anesthesia in patients with polymyositis for any surgery have been published in the literature.73–77 Onset of action of muscle relaxants is slow but increased sensitivity leads to a slower recovery from them. It is recommended to avoid succinylcholine for intubation as these patients are at increased risk of rhabdomyolysis and hyperkalemia. Muscle relaxant antagonists may cause arrhythmias and weakness. It is necessary to monitor muscle relaxation with a peripheral nerve stimulator and try to use minimal to no muscle relaxation or use regional anesthetic techniques when possible.
MYASTHENIA GRAVIS
Myasthenia gravis (MG) is an autoimmune disorder involving the neuromuscular junction with functional loss of the nicotinic acetylcholine receptors secondary to the presence of auto antibodies against such receptors.78 MG is characterized by episodes of muscle weakness worsened by activity and exercise and improved with rest. With exercise, patients may develop difficulty with speech, chewing, swallowing, and can even have difficulty with coordination of pharyngeal functions that may lead to increased risk of aspiration of oral contents. Typically, in patients with ocular symptoms such as diplopia and ptosis, with progression of the disease, weakness may progress to affect bulbar, limb, and respiratory muscles. Up to 20% of patients may develop a myasthenic crisis in which respiratory muscles are involved requiring ventilator support.79–81
Up to 75% of affected individuals have coexistent thymic hyperplasia or a thymoma.80–84
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


