5 Pelvic pain
Chronic Pelvic Pain
Why do patients with chronic pelvic pain often cause ‘heartsink’ in their GPs?
Chronic pelvic pain (CPP) can be defined as recurrent or constant pelvic pain of at least 6 months’ duration, unrelated to periods, intercourse or pregnancy. A more detailed definition is given in Box 5.1. It is one of those enigmatic presentations that frustrate GPs because of the difficulties they have in both diagnosing the problem and then implementing effective treatment.
BOX 5.1 The American College of Obstetricians and Gynecologists’ (ACOG) definition of chronic pelvic pain
(From ACOG1)
How common a problem is chronic pelvic pain?
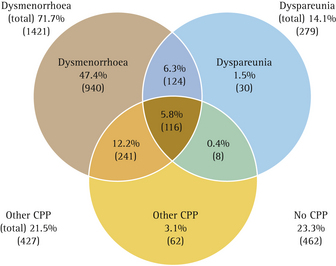
It is a very common presentation. The annual prevalence in the primary-care setting in women aged between 15 and 73 years is 38/1000. This is almost the same as the prevalence of migraine, asthma and back pain.2 A community-based study undertaken in the USA has found a prevalence of 15% for pelvic pain of >1 year’s duration.3 It is the indication for about one-third of laparoscopies and 10–15% of hysterectomies performed in the USA.4 A recent Australian study reported on pelvic pain experienced by women over the last 12 months, documenting the relationships between dyspareunia, dysmenorrhoea and chronic pelvic pain.52 This is well illustrated in Figure 5.1.
How should chronic pelvic pain be approached?
While there are no differences in the prevalence across social class or with marital or employment status,5 psychosocial factors that may impact on the development of CPP include:6
How a woman deals with her pain and social isolation can also exacerbate the situation.7
Numerous studies have documented the higher prevalence of both childhood and adult physical and sexual abuse in women who complain of CPP when compared with pain-free populations.8–11
Unfortunately, several adverse outcomes can arise from unresolved CPP. The severity of the pain can increase, often leading to the implementation of unproven surgical or medical intervention. Disability, or at least impaired health status, may come about. Depression and substance abuse can also ensue. Women with CPP may also have inappropriate healthcare utilisation. One study found that women with CPP had undergone five times as much previous surgery and sought treatment for four times as many somatic complaints when compared with women without pain.10
What conditions can cause pelvic pain?
Several conditions can result in CPP. They may be gynaecological, gastrointestinal or genitourinary in nature (Table 5.1) and symptoms can arise from any of these systems. For example, one community-based study12 has shown that about half of women with CPP have additional symptoms: 39% had irritable bowel syndrome and 24% had genitourinary symptoms. Furthermore, the prevalence of dysmenorrhoea and dyspareunia is higher in women with CPP than in those without CPP (81% and 41% respectively versus 58% and 14%). These results are concordant with other studies.3,13
TABLE 5.1 Major causes of chronic pelvic pain
| Gynaecological | Gastrointestinal | Genitourinary |
|---|---|---|
| Interstitial cystitis |
GPs should be aware that while conditions such as endometriosis and pelvic adhesions can be found in women with CPP, they do not necessarily cause the pain. There is a poor correlation between the severity of endometriosis and pain. Indeed the majority of patients with mild, moderate and severe disease are asymptomatic.14 Similar rates of both macroscopic and microscopic endometriosis have been found in women suffering from infertility and pelvic pain when compared with a pain-free group of women who had laparoscopic tubal ligation.15 There is also no difference in the prevalence of pelvic adhesions in patients with CPP compared with pain-free women,16 nor is there any benefit from lysis of the adhesions.17
Is there such a thing as pelvic congestion?
It has been suggested that other conditions are involved in the aetiology of CPP. These incidental or spurious conditions include uterine retroversion, peritoneal defects and pelvic venous congestion. The last of these is particularly controversial. Pelvic venous congestion is said to occur as a result of varices of the ovarian veins.18 Some say it is a common finding in women with CPP, but the pathophysiology of this condition is poorly understood19 and it is not clear whether ‘pelvic congestion’ is a normal or abnormal finding in women. A study of asymptomatic kidney donors showed a 9.9% prevalence of ovarian varices in the general population.20 While interventional radiology has been used to ‘treat’ pelvic congestion, other authors state that there is no objective evidence to suggest that it is a significant factor in CPP in women.21
What aspects of the history are important?
The more recent history of the condition should also be sought, by asking whom the patient has already seen about this condition and what tests and/or treatments have been carried out. It is worthwhile finding out exactly how disabling the condition is and whether or not it is interfering with the woman’s daily activities. Often disability has developed gradually and it may be useful to identify inflection points in the curve of disability brought about by external life events or events within the family.22
What investigative pathway should be used?
Some suggest that undertaking a history and physical examination should be sufficient for the evaluation of a woman with CPP, unless specific abnormalities are detected.6,23 Routine use of ultrasonography and laparoscopy is generally unrewarding and not indicated.24 However, in an effort to find a cause and appease the patient, many women will be sent for an ultrasound to look for ovarian cysts, fibroids and large hydrosalpinges or pyosalpinges. A laparoscopy then follows, seeking signs of endometriosis or pelvic adhesions.
More than 40% of laparoscopies are performed for the diagnosis of CPP. Although laparoscopic evaluation is sometimes considered a routine part of the evaluation, ideally the decision to perform a laparoscopy should be based on the patient’s history, physical examination and the findings of non-invasive tests. About 65% of women with CPP have at least one diagnosis detectable by laparoscopy and it is common to attribute causality to this diagnosis. Endometriosis is diagnosed in one-third of laparoscopies for CPP. Endometriosis requires histological confirmation to assure an accurate diagnosis. Adhesions are diagnosed in about one-quarter of laparoscopies. Ovarian cysts, hernias, pelvic congestion syndrome, ovarian remnant syndrome, ovarian retention syndrome, postoperative peritoneal cysts and endosalpingiosis are other diagnoses that are made laparoscopically in some cases.25
What non-drug management can I offer patients with chronic pelvic pain?
Cognitive behavioural therapy may be helpful, not only by assisting the patient to control the pain but also in reducing disability and promoting wellbeing. By teaching muscle relaxation, controlled breathing and the use of imagery, GPs can help their patients decrease their general level of arousal and divert their attention from the physical signals that preoccupy them. Cognitive techniques that address maladaptive and negative thinking, such as fear of cancer, should also be introduced and rehearsed with the patient. Cognitive behavioural pain management should also focus on stress management and, in particular, on methods that can be used by the patient to identify the cause of her stress and how to address these issues in a constructive way (e.g. through problem solving, assertiveness and time management).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree