Pelvic Lymphadenectomy
Robert E. Bristow
INTRODUCTION
The pelvic lymph nodes may be a site of early metastatic spread of cervical, endometrial, and ovarian cancers. Consequently, surgical removal of pelvic lymph nodes is an important component of surgical staging for these cancers and may serve as a diagnostic procedure, a therapeutic procedure, or both. For cervical cancer, pelvic lymphadenectomy is considered both diagnostic and therapeutic when performed in conjunction with radical hysterectomy. Pelvic lymphadenectomy performed for ovarian cancer apparently confined to the pelvis has been associated with improved progression-free survival but does not impact overall survival. The role of pelvic lymphadenectomy for endometrial cancer has not been conclusively determined; however, knowledge of lymph node status permits individualization of adjuvant therapy. Finally, removal of gross lymphadenopathy for patients with ovarian and endometrial cancers may be required to achieve optimal or complete tumor cytoreduction.
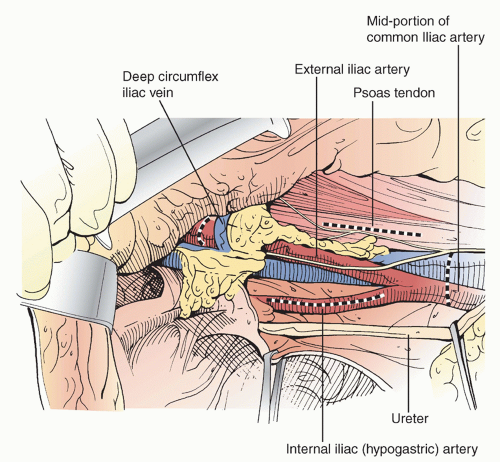
Pelvic lymphadenectomy reflects complete or nearcomplete removal of all lymph node tissue within well-defined anatomic boundaries. The important anatomic landmarks are: proximal—the mid-portion of the common iliac artery; distal—deep circumflex iliac vein; lateral—tendon of the psoas muscle and fascia of obturator internus; medial—internal iliac (hypogastric) artery and ureter; and posterior—obturator nerve or hypogastric vein (depending on the extent of resection) (Figure 11.1). An adequate nodal yield from pelvic lymphadenectomy has been variably defined. The Gynecologic Oncology Group requires documentation of at least 4 lymph nodes harvested from each side; however, a minimum total pelvic count of 11 lymph nodes has been shown to correlate with clinical outcome in endometrial cancer. A median total pelvic node count in excess of 30 lymph nodes is not uncommon but is also associated with a higher risk of complications. Pelvic lymph node sampling is a more limited procedure within the same general anatomic boundaries as pelvic lymphadenectomy; however, lymph node sampling is not associated with the same diagnostic accuracy as lymphadenectomy and is not a reliable method of excluding lymph node metastasis. Lymph node sampling is usually intended to remove any enlarged or clinically suspicious nodes. Pelvic lymph node dissection is a vague term that may describe a procedure ranging from lymph node sampling to lymphadenectomy.
PREOPERATIVE CONSIDERATIONS
In preparation for pelvic lymphadenectomy, all patients should undergo a comprehensive history and physical examination focusing on those areas that may indicate a reduced capacity to tolerate major surgery or place the patient at elevated risk for postoperative complications. Routine laboratory testing should include a complete blood count, serum electrolytes, age-appropriate health screening studies, a chest radiograph, and electrocardiogram for women aged 50 years and older. Preoperative computed tomography of the abdomen and pelvis (and chest, depending on clinical indications) is helpful to
evaluate the extent of disease and for surgical planning purposes.
evaluate the extent of disease and for surgical planning purposes.
Preoperative mechanical bowel preparation (oral polyethylene glycol solution or sodium phosphate solution with or without bisacodyl) is unnecessary for pelvic lymphadenectomy but may be recommended according to the surgeon’s preference for other concurrent components of the procedure (e.g., hysterectomy). Prophylactic antibiotics (Cephazolin 1 g, Cefotetan 1 to 2 g, or Clindamycin 800 mg) should be administered 30 minutes prior to incision, and thromboembolic prophylaxis (e.g., pneumatic compression devices and subcutaneous heparin) should be initiated prior to surgery. A self-retaining retractor (e.g., Bookwalter, Codman Division, Johnson & Johnson, Piscataway, NJ) with a fixed arm attaching the retractor ring to the operating table is advisable to optimize exposure, maximize patient safety, and reduce surgeon fatigue. Following is a brief description of the surgical procedure used (see also video: Pelvic Lymphadenectomy).
SURGICAL TECHNIQUE
 The patient may be positioned in the dorsal low-lithotomy (perineal lithotomy) position using Allen Universal Stirrups (Allen Medical Systems, Cleveland, OH) or supine on the operating table, depending on the requirements for concurrent procedures. Pelvic lymphadenectomy can be performed through a variety of incisions: low transverse, vertical midline, vertical lateral or paramedian, J-incision, extraperitoneal, laparoscopic, or robotically assisted. Similarly, the surgeon may choose from a variety of instruments to perform pelvic lymphadenectomy, including scissors, hemo-clips, the electrosurgical unit, a vessel-sealing device, and the Argon beam coagulator. The most important point, however, is to develop a routine and proceed through the dissection in a systematic fashion to ensure anatomic consistency from one case to the next.
The patient may be positioned in the dorsal low-lithotomy (perineal lithotomy) position using Allen Universal Stirrups (Allen Medical Systems, Cleveland, OH) or supine on the operating table, depending on the requirements for concurrent procedures. Pelvic lymphadenectomy can be performed through a variety of incisions: low transverse, vertical midline, vertical lateral or paramedian, J-incision, extraperitoneal, laparoscopic, or robotically assisted. Similarly, the surgeon may choose from a variety of instruments to perform pelvic lymphadenectomy, including scissors, hemo-clips, the electrosurgical unit, a vessel-sealing device, and the Argon beam coagulator. The most important point, however, is to develop a routine and proceed through the dissection in a systematic fashion to ensure anatomic consistency from one case to the next.A self-retaining retractor is placed with particular attention to exposure of the pelvic sidewall and elevation of the peritoneum in the area of the round ligament to expose the distal external iliac node (Jackson’s node). The lateral retractor blades should not be resting on the psoas muscle, as this can result in traumatic injury to the femoral nerve. Usually, the round ligaments would have been ligated and divided as part of a preceding hysterectomy. The suture ligature on the round ligament pedicle is elevated and the pelvic wall peritoneum is opened lateral and parallel to the external iliac and common iliac vessels. To improve exposure to the common iliac vessels, the descending and sigmoid colon are mobilized from its attachments to the left lateral pelvic wall and paracolic gutter. On the right side, the peritoneum surrounding the proximal ascending colon,




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree