Chapter 62 Pediatric Emergencies and Resuscitation
Injuries are the leading cause of death in American children and young adults and are responsible for more childhood deaths than all other causes combined (Chapter 5.1). Children are particularly vulnerable to injury for a number of reasons, including their small size, relative physical uncoordination, and limited ability to predict or understand danger. In addition, the immaturity of their developing bones, ligaments, and muscles; their thin body walls; and their relatively large heads, compared with total body surface area, make young children susceptible to serious or fatal injury from falls and collisions.
Serious injuries can become fatal when appropriate medical care is delayed.
Approach to the Emergency Evaluation of a Child
General Assessment
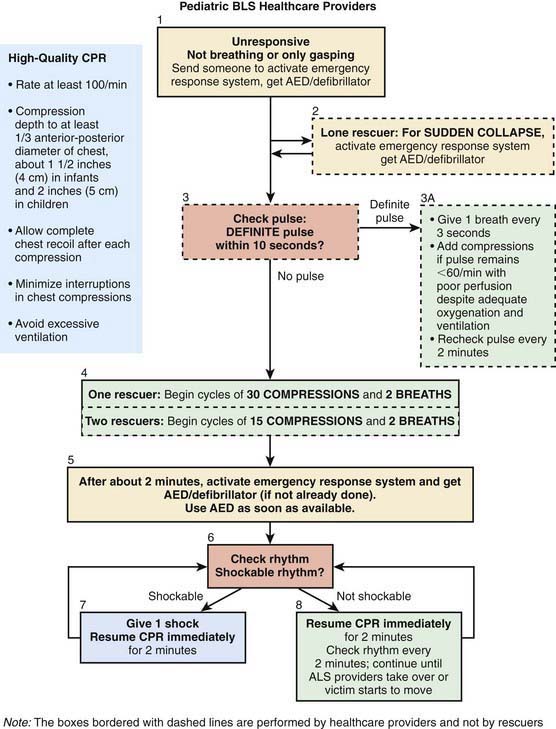
Once the caregiver and patient’s safety has been ensured, the caregiver performs a rapid visual survey of the child, assessing the child’s general appearance and cardiopulmonary function. This action should be very quick (only a few seconds) and should include assessment of (1) general appearance (determining color, tone, alertness, and responsiveness); (2) adequacy of breathing (distinguishing between normal, comfortable respirations and respiratory distress or apnea); and (3) adequacy of circulation (identifying cyanosis, pallor, or mottling). A child found unresponsive from an unwitnessed collapse should be approached with a gentle touch and the verbal question, “Are you OK?” If there is no response, the caregiver should immediately shout for help and send someone to both activate the emergency response system (EMS) and locate an automated external defibrillator (AED) (Fig. 62-1). The provider should then determine whether the child is breathing and, if not, provide 2 rescue breaths as described later under Recognition and Treatment of Respiratory Distress and Failure. If the child is adequately breathing, then the circulation is quickly assessed. Any child with a heart rate below 60 beats/min or without a pulse requires immediate CPR, as described under Cardiac Arrest. If the caregiver witnesses the sudden collapse of a child, the caregiver should have a higher suspicion for a sudden cardiac event. In this case, rapid deployment of an AED is of paramount importance. The provider should very briefly delay care of the child to activate EMS and locate the nearest AED.
Primary Assessment
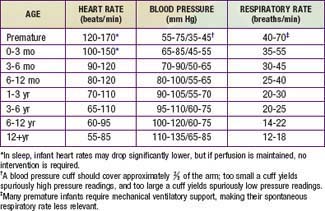
The exam and vital sign data can be interpreted only if the caregiver has a thorough understanding of normal values. In pediatrics, normal respiratory rate, heart rate, and blood pressure have age-specific norms (Table 62-1). These ranges can be difficult to remember, especially if used infrequently. However, several standard principals apply: (1) no child’s respiratory rate should be >60 breaths/min for a sustained period; (2) normal heart rate is roughly 2-3 times normal respiratory rate for age; and (3) a simple guide for pediatric blood pressure (BP) is that the lower limit of systolic BP should be <60 mm Hg for neonates; <70 mm Hg for 1 mo–1 yr olds; <70 mm Hg + (2 × age) for 1-10 yr olds; and <90 mm Hg for any child older than 10 yr.
Airway and Breathing
The most common precipitating event for cardiac instability in infants and children is respiratory insufficiency. Therefore, rapid assessment of respiratory failure and immediate restoration of adequate ventilation and oxygenation remain the first priority in the resuscitation of a child. Using a systematic approach, the caregiver should first assess whether the child’s airway is patent and maintainable. A healthy, patent airway is open and unobstructed, allowing normal respiration without noise or effort. A maintainable airway is one that is either already patent or can be made patent with a simple maneuver. To assess airway patency, the provider should look for breathing movements in the child’s chest and abdomen, listen for breath sounds, and feel the movement of air at the child’s mouth and nose. Abnormal breathing sounds (i.e., snoring or stridor), increased work of breathing, and apnea are all findings potentially consistent with airway obstruction. If there is evidence of airway obstruction, then maneuvers to relieve the obstruction should be instituted before the caregiver proceeds to evaluate the child’s breathing (see under Recognition and Treatment of Respiratory Distress and Failure, Initial Management).
Disability
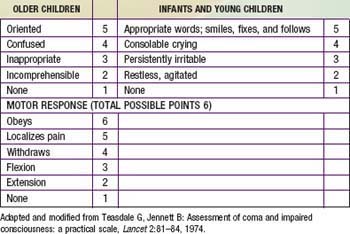
In the setting of a pediatric emergency, disability refers to a child’s neurologic function in terms of the level of consciousness and cortical function. Standard evaluation of a child’s neurologic condition can be done quickly with an assessment of pupillary response to light (if one is available) and use of either of the standard scores used in pediatrics: the Alert, Verbal, Pain, Unresponsive (AVPU) Pediatric Response Scale and the Glasgow Coma Scale (GCS) (Tables 62-2 and 62-3). The causes of decreased level of consciousness in children are numerous and include conditions as diverse as respiratory failure with hypoxia or hypercarbia, hypoglycemia, poisonings or drug overdose, trauma, seizures, infection, and shock. Most commonly, an ill or injured child has an altered level of consciousness because of respiratory compromise, circulatory compromise, or both. Any child with a depressed level of consciousness should be immediately assessed for abnormalities in cardiorespiratory status.
Table 62-2 AVPU NEUROLOGIC ASSESSMENT
| A | The child is awake, alert, and interactive with parents and care providers |
| V | The child responds only if the care provider or parents call the child’s name or speak loudly |
| P | The child responds only to painful stimuli, such as pinching the nail bed of a toe or finger |
| U | The child is unresponsive to all stimuli |
From Ralston M, Hazinski MF, Zaritsky AL, et al, editors: Pediatric advanced life support course guide and PALS provider manual: provider manual, Dallas, 2007, American Heart Association.
The Alert, Verbal, Pain, Unresponsive Pediatric Response Scale
The AVPU scoring system is used to determine both a child’s level of consciousness and cerebral cortex function. Unlike the GCS (see later), the AVPU scale is not developmentally dependent—a child does not have to understand spoken language or follow commands, merely respond to a stimulus. The child is scored according to the amount of stimulus required to get a response, from alert (no stimulus, the child is already awake and interactive) to unresponsive (child does not respond to any stimulus) (see Table 62-2).
The Glasgow Coma Scale
Although the GCS has not been validated as a prognostic scoring system for infants and young children as it has been in adults, it is commonly used in the assessment of pediatric patients with an altered level of consciousness. The GCS is the most widely used method of evaluating a child’s neurologic function and has 3 components. Individual scores for eye opening, verbal response, and motor response are added together, with a maximum of 15 points (see Table 62-3). Patients with a GCS score ≤8 require aggressive management, including stabilization of the airway and breathing with endotracheal intubation and mechanical ventilation, respectively, and, if indicated, placement of an intracranial pressure monitoring device.
Tertiary Assessment
The tertiary assessment occurs in a hospital setting, where ancillary laboratory and radiographic assessments contribute to a thorough understanding of the child’s condition. A basic blood chemistry profile, complete blood count, liver function tests, coagulation studies, and arterial blood gas analyses give fairly broad (but somewhat nonspecific) estimates of renal function, acid-base balance, cardiorespiratory function, and presence or absence of shock. Chest radiographs can be useful to evaluate both the heart and lungs, although more detailed estimates of heart function and cardiac output can be made with echocardiography. Arterial and central venous catheters can be placed to monitor arterial and central venous pressure (see under Vascular Access).
Recognition and Treatment of Respiratory Distress and Failure
Airway Obstruction
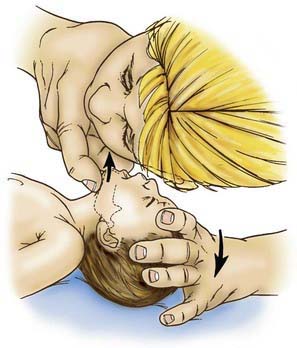
Airway obstruction is treated with a sequential approach, starting with the head-tilt/chin-lift maneuver to open and support the airway, followed by inspection for a foreign body, and finger-sweep clearance or suctioning if one is visualized (Fig. 62-2). Blind suctioning or finger sweeps of the mouth are not recommended. A nasopharyngeal airway (NPA) or oropharyngeal airway (OPA) can be inserted for airway support, if indicated. A conscious child suspected of having a partial foreign body obstruction should be permitted to cough spontaneously until coughing is no longer effective, respiratory distress and stridor increase, or the child becomes unconscious.
If the child becomes unconscious, the child should be gently placed on the ground, supine. The provider should then open the airway with the head-tilt/chin-lift maneuver and attempt mouth-to-mouth ventilation (Figs. 62-3 and 62-4). If ventilation is unsuccessful, the airway is repositioned, and ventilation attempted again. If there is still no chest rise, attempts to remove a foreign body are indicated. In an infant <1 yr old, a combination of 5 back blows and 5 chest thrusts is administered (Fig. 62-5). After each cycle of back blows and chest thrusts, the child’s mouth should be visually inspected for the presence of the foreign body. If identified within finger’s reach, it should be removed with a gentle finger sweep. If no foreign body is visualized, ventilation is again attempted. If this is unsuccessful, the head is repositioned, and ventilation attempted again. If there is no chest rise, the series of back blows and chest thrusts is repeated.
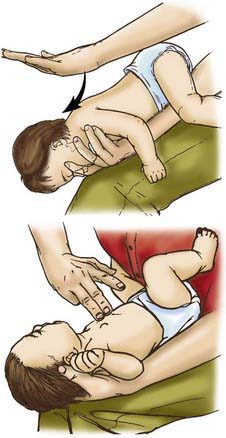
Figure 62-5 Back blows (top) and chest thrusts (bottom) to relieve foreign body airway obstruction in the infant.
(From Guidelines for cardiopulmonary resuscitation and emergency cardiac care. Emergency Cardiac Care Committee and Subcommittees, American Heart Association. Part V. Pediatric basic life support, JAMA 268:2251–2261, 1992.)
For a conscious child >1 yr old, providers should give a series of 5 abdominal thrusts (Heimlich maneuver) with the child standing or sitting (Fig. 62-6); this should occur with the child lying down if unconscious (Fig. 62-7). After the abdominal thrusts, the airway is examined for a foreign body, which should be removed if visualized. If no foreign body is seen, the head is repositioned, and ventilation attempted. If it is unsuccessful, the head is repositioned and ventilation is attempted again. If these efforts are unsuccessful, the Heimlich sequence is repeated.

Figure 62-6 Abdominal thrusts with the victim standing or sitting (conscious).
(From Guidelines for cardiopulmonary resuscitation and emergency cardiac care. Emergency Cardiac Care Committee and Subcommittees, American Heart Association. Part V. Pediatric basic life support, JAMA 268:2251–2261, 1992.)
Airway Narrowing
Airway support for these processes is dictated by both the underlying condition and the clinical severity of the problem. In cases of mild upper airway obstruction, the child has minimally elevated work of breathing (evidenced by tachypnea and few to mild retractions). Stridor, if present at all, should be audible with only coughing or activity. Children with these findings can be supported with nebulized cool mist and supplemental oxygen as needed. In cases with moderate obstruction, in which the child has a higher work of breathing and more pronounced stridor, nebulized racemic epinephrine and oral or intravenous (IV) dexamethasone can be added. Children with severe upper airway obstruction have marked retractions, prominent stridor, and decreased air entry on auscultation of the lung fields. Most children with significant airway obstruction are also hypoxic, and many appear dyspneic and agitated. A child in severe distress needs to be closely observed, as the signs of impending respiratory failure may be initially confused with improvement. Stridor becomes quieter and retractions less prominent when a child’s respiratory effort begins to diminish. The child in respiratory failure can be distinguished from one who is improving by evidence of poor air movement on auscultation and lethargy or decreased level of consciousness from hypercarbia, hypoxia, or both. When anaphylaxis is suspected as the cause for upper airway edema, providers should administer an intramuscular (IM) or IV dose of epinephrine as needed (Chapter 143). No matter the cause, any child in impending respiratory failure should be prepared for endotracheal intubation and respiratory support.
In cases of lower airway obstruction, therapies are targeted to both relieving the obstruction and reducing the child’s work of breathing. Inhaled bronchodilators, such as albuterol, augmented by oral or IV corticosteroids, remain the mainstay of therapy in settings of mild to moderate acute distress due to lower airway obstruction. Children with more significant obstruction appear dyspneic, with tachypnea, retractions, and easily audible wheezing. In these cases, the addition of an anticholinergic agent, such as nebulized ipratropium bromide, or a smooth muscle relaxant, such as magnesium sulfate, may provide further relief, although the evidence for these measures remains controversial (Chapter 138). Supplemental oxygen and IV fluid hydration can also be useful adjuncts. As in cases of upper airway obstruction, impending respiratory failure in children with lower airway obstruction can be insidious. When diagnosed early in a school-aged child who is cooperative, respiratory failure can be averted through judicious use of noninvasive support, with continuous positive airway pressure (CPAP), bilevel positive airway pressure (BiPAP), or heliox (combined helium-oxygen therapy). Endotracheal intubation should be performed only by skilled providers, preferably in a hospital setting, because there is a high risk of respiratory and circulatory compromise in patients with lower airway obstruction during the procedure.
Advanced Airway Management Techniques
Bag-Valve-Mask Positive Pressure Ventilation
Rescue breathing with a bag-valve-mask apparatus can be as effective as endotracheal intubation and safer when the provider is inexperienced with intubation. Bag-valve-mask ventilation itself requires training to ensure that the provider is competent to select the correct mask size, open the child’s airway, form a tight seal between the mask and the child’s face, deliver effective ventilation, and assess the effectiveness of the ventilation. An appropriately sized mask is one that fits over the child’s mouth and nose but does not extend below the chin or over the eyes (Fig. 62-8). An adequate seal is best achieved via a combination “C–E” grip on the mask, in which the thumb and index finger form the letter “C” on top of the mask, pressing the mask downward onto the child’s face, and the remaining three fingers form an “E” grip under the child’s mandible, holding the jaw forward and extending the head up toward the mask. Using this method, the care provider can secure the mask to the child’s face with one hand and use the other hand to compress the ventilation bag (Fig. 62-9).
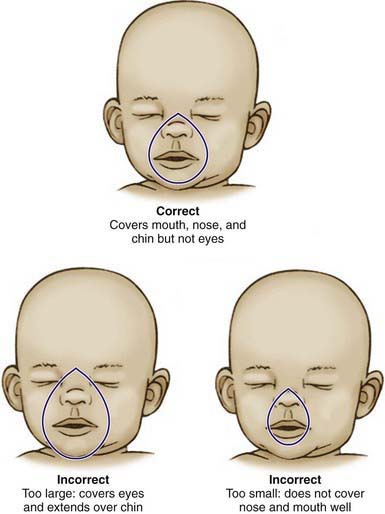
Figure 62-8 Appropriate sizing technique for pediatric bag-valve-mask apparatus.
(From American Academy of Pediatrics and the American Heart Association; Short J, editor: Textbook of neonatal resuscitation, ed 5, Elk Grove, IL, American Academy of Pediatrics, 2006, pp 3–16.)
The provider may have to move the head and neck through a range of positions to find the one that best maintains airway patency and allows maximal ventilation. In infants and young children, optimal ventilation is often provided when the child’s head is in the neutral “sniffing” position without hyperextension of the head (Fig. 62-10
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree