Pediatric and Adolescent Gynecology
Normal Genital Anatomy
The genital tract undergoes visible morphologic changes from infancy through childhood and adolescence.1,2 At birth, owing to the influence of maternal circulating estrogens, the labia majora are anteriorly placed and edematous. They are thickened and cover the introital opening. The clitoral proportion is also larger. The vestibule and hymen are pale and thickened, and can occlude visualization of the vaginal canal without manipulation. The vagina is rugated and moist, and vaginal secretions may be present. The cervix is visible, and the uterus may contain functioning endometrial tissue, which can result in estrogen-withdrawal bleeding in infancy.
During early childhood, the vulva remodels with thinning and attenuation of the labia majora and minora. The vestibule becomes erythematous with prominent vascular markings. It may now be unopposed by the labia, allowing for easy visualization of the vaginal orifice with minimal retraction. The hymen of a prepubescent female is normally easily visualized and is thin, often translucent, and inelastic. Normal variations in the shape and amount of hymenal tissue have been described (Fig. 74-1).3–5 The vagina has an erythematous appearance without rugations. Normally, the pH is mildly basic and a mixture of bacterial flora is present. The cervix is flush with the vaginal vault and the uterine fundus is poorly developed, with no endometrial development.
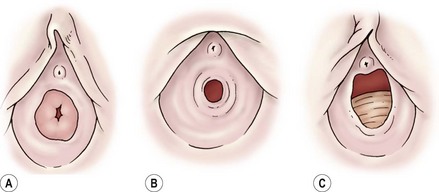
FIGURE 74-1 Normal anatomic variations of the hymen. (Adapted from Pokorny SF, Stormer J. Atraumatic removal of secretions from the prepubertal vagina. Am J Obstet Gynecol 1987;156:581–3.)
With the onset of puberty, the vestibule begins to lose its erythematous appearance. The hymen thickens and becomes elastic and redundant.6 The vagina grows in length and develops rugations. The cervix has a well-defined junction from the uterus, and the uterine fundus develops a rounded appearance. Endometrial tissue is present.
Follicular activity within the ovary, with small cyst formation, can be observed on imaging as early as 16 weeks of gestation.7 Three to 5% of children have small incidental ovarian cysts detected on ultrasound (US).8 Follicular growth followed by involution continue throughout childhood, with increased follicular activity and size coinciding with increasing age.9 Ovarian volume and position change with age, with the ovaries being intra-abdominal in childhood and assuming a pelvic position at puberty.
Genital Examination
An adequate light source and proper positioning are usually all that are needed to accomplish an examination in a prepubertal child.10 For visualization of the vulva, introital opening, and lower vagina, gentle downward traction on the labia in a lithotomy position is usually successful (Fig. 74-2). The knee–chest position may offer a clearer view of the hymen and lower vagina (Fig. 74-3).11 A colposcope (or otoscope) may be helpful to see the detail of the vestuble and lower vagina.12 The office use of vaginal speculums is discouraged in prepubertal children. When vaginal inspection is needed, it should be done using endoscopic instruments under sedation.13,14 By gently occluding the vaginal orifice, the entire vaginal canal can be visualized with hydrodistention.15 Speculum examinations of the vagina are usually well tolerated in postpubertal girls when a narrow-caliber straight blade speculum is gently inserted. Bimanual examinations can be accomplished through a rectal approach or, in adolescents, with a single digit inserted into the vaginal fornix. Imaging with abdominal ultrasound or, occasionally magnetic resonance imaging (MRI), is adjuvant to examination and provides additional information about the upper genital tract.16

FIGURE 74-2 Examination of the genitalia by labial traction. Gently grasping the posterior labia majora and pulling anteriorly and superiorly allows visualization of the genital structures.
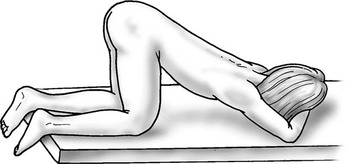
FIGURE 74-3 Knee–chest positioning. The lower vagina and hymen can occasionally be viewed more successfully by using the knee–chest position.
Vulvar Abnormalities
Vulvar pruritus, pain, and discharge are common complaints in children. An etiology can be obtained in most cases with careful external inspection and, if necessary, blind vaginal cultures. Biopsy is seldom indicated. Most often, symptoms involve irritation or eruption of the vulvar skin related to hygiene or common skin conditions. Atopic or irritant dermatitis are the most common diagnoses.17 Infections are associated with acute inflammation with mucosal erythema and the presence of a vaginal discharge.18 Common respiratory pathogens such as Streptococcus pyogenes and Haemophilus influenzae may occasionally cause acute genital symptoms.19,20 When a bacterial infection is suspected, cultures of the vagina can be obtained by using moistened urethral swabs, feeding tubes, or catheters.
Vulvar dermatoses can lead to acute vulvovaginal symptoms. Lichen sclerosis has the hallmark characteristic of a loss of skin markings with a sharply demarcated pale epithelial ring encircling the introitus, but sparing the vagina (Fig. 74-4). Signs of inflammation and trauma may be present, with purpura, fissures, and secondary infection associated with scratching. Principles of treatment include avoidance of irritation and loose clothing, mild soaps, and the generous use of emollients. Early treatment with ultrapotent corticosteroids may be effective in reducing symptoms of lichen sclerosis and minimizing long-term scarring. In 20% of patients, ultrapotent corticosteroids have been shown to reverse skin changes.21 Tacrolimus has also been reported to offer similar benefit to pediatric patients.22 Other dermatologic conditions such as psoriasis, eczema, and allergic dermatitis also may mimic vulvovaginitis.19

FIGURE 74-4 Lichen sclerosis diagnosed in a 5-year-old. A sharp demarcation of hypopigmented, thin epithelium is seen. This lesion is often associated with fissures and purpura.
Labial adhesions occur frequently in prepubescent girls (Fig. 74-5). Adhesions are thought to occur because of irritation or trauma to the unestrogenized labia. Adhesions can be associated with urinary tract infections, perineal wetness, symptomatic vulvitis, and an inability to access the urethra. When symptomatic, preferred treatment has historically been estrogen-based cream applied under traction to the labia. Newer investigations suggest that betamethasone cream may have equal efficacy.23,24 The need for adhesiolysis is low because of the efficacy of topical therapy, but may be necessary in both unusually dense adhesions or those that have required previous separation. Manual separation of the adhesions without anesthesia should be avoided because of the discomfort and the high risk of recurrence. For thin adhesions, office separation using long acting local anesthetics, such as EMLA cream, is a reasonable option.25
Genital Bleeding
Bleeding from the genital area in a prepubescent child is always abnormal (Box 74-1). Bleeding is most commonly extragenital, resulting from hematuria, rectal fissures, and vulvar epithelial irritation. Prolapse of the urethra can occur and may be associated with bleeding or even gangrenous changes (Fig. 74-6). Topical treatment with estrogen-based cream usually relieves the symptoms. If symptoms persist, excision of the redundant tissue may be necessary.26 Vaginal bleeding can be associated with precocious puberty or autonomous production, or with exogenous sources of hormonal stimulation. It is important to perform a detailed physical examination searching for evidence of breast development, estrogenization of the genital tract, or the presence of an abdominal mass. In the absence of a satisfactory explanation for the source of bleeding, vaginoscopy should be performed to exclude a foreign body, trauma, infection or, rarely, primary and metastatic tumors of the lower genital canal (Fig. 74-7).

FIGURE 74-6 Urethral prolapse was found in this 6-year-old child with a history of recurrent painless genital bleeding.

FIGURE 74-7 A 12-year-old adolescent, presenting with refractory dysfunctional uterine bleeding, is diagnosed with a neuroendocrine tumor of the cervix at vaginoscopy.
Acute genital bleeding in children requires immediate evaluation for the presence of serious injury or sexual abuse.27 If the source of bleeding is not readily apparent, if the entire lesion cannot be identified, or if the patient is not tolerant of the examination, vaginoscopy under sedation is needed.28,29 Straddle injuries are common during childhood from accidental falls onto blunt objects, resulting in soft tissue trauma from striking the perineum. Straddle injuries usually involve the mons, clitoris, and labia, sparing the vaginal ring or perineal body (Fig. 74-8). They may result in a hematoma, linear lacerations, or abrasions. Vulvar hematomas can be extensive but are more commonly self-limited. In the absence of acute ongoing hemorrhage, small or moderate hematomas can be managed conservatively with bed rest, ice, and pain control. Evacuation of extremely large hematomas causing distortion of the midline pelvic structures occasionally is necessary to facilitate recovery. Evacuation with debridement should be performed with the child under anesthesia by incising the medial mucosal surface and placing absorbable sutures for hemostasis and closure of dead space.

FIGURE 74-8 An extensive vulvar hematoma is seen after a straddle injury. (Courtesy of Diane Merritt, MD.)
Penetrating injuries can occur through accidental impalements onto irregular objects, but the possibility of sexual abuse must always be considered (Figs 74-9 and 74-10). In the prepubertal child, lacerations involving or occurring above the hymenal ring require vaginoscopy under general anesthesia. Because of the inelasticity of the vaginal epithelium, penetrating injuries can result in disruption of the vagina, with possible internal hemorrhage and hematoma formation.29 Injuries that cannot readily be explained by the history should be referred to child protection. Surgeons should familiarize themselves with the legal and social resources for sexual abuse and care that are available within their communities.

FIGURE 74-9 A 9-year-old girl has a penetrating posterior vaginal injury sustained after falling onto an open cabinet. A urinary catheter has been inserted in the urethra.
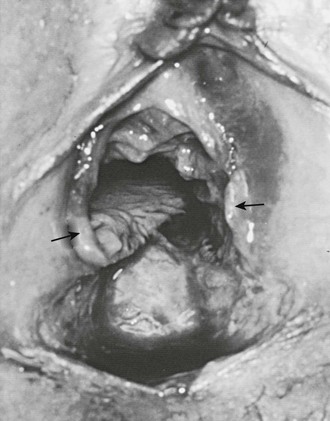
FIGURE 74-10 An 8-year-old victim of acute sexual assault has small bowel herniating through the apex of the avulsed vagina. Note the abundant, although transected, amount of hymenal tissue (arrows) present, indicating that she had not had significant stretch trauma to her hymen before this episode of rape. (From Pokorny SF, Pokorny WJ, Kramer W. Acute genital injury in the prepubertal girl. Am J Obstet Gynecol 1992;166:1461–6.)
Introital masses in children occasionally come to the attention of surgeons. Masses of the introitus or vagina are most commonly epithelial inclusion cysts of the hymen or lower vagina, and often spontaneously resolve. There is a rare possibility of embryonic rhabdomyosarcoma, a malignant primary tumor that appears as indolent, grape-like masses protruding from the vagina (Fig. 74-11). Other possibilities include condylomata acuminata, ectopic ureter, or an obstructive vaginal anomaly. Occasionally, the Bartholin gland or periurethral gland may occlude or form an abscess, leading to an acquired lateral mass. Transperineal ultrasound can be helpful. In cases that are unclear, biopsy or excision (or both) may be necessary.





