1 | Pathogens |
Normal Flora and Virulence
Of the many millions of existing microorganisms, only a few hundreds are capable of causing disease in humans. The number of pathogens relevant for gynecologists is probably far below a hundred.
Many bacteria coexist with humans on good terms. These “friendly“ bacteria belong to the normal flora present in the intestinal tract and on the skin and mucosae, where they perform functions that are partly beneficial and essential.
This is different with viruses. If detected, viruses are always pathologically significant. So far, no benefits to humans have been recognized.
Nevertheless, the majority of people are colonized by some viruses throughout life, e. g., with herpesviruses or papillomaviruses.
Whether or not an infection occurs depends, among other things, on the virulence of the individual pathogen. This refers to the degree of pathogenicity (the capacity to cause infections and inflammation). First, the pathogen must be able to invade the organism—or, in the case of viruses, to invade the cells in which to multiply— and, second, it must be able to cause disease. The property of virulence is developed differently in different pathogenic species, even in individual strains (for example, not every Escherichia coli strain has the same virulence).
Virulence factors include adhesion properties and the production of certain enzymes (neuraminidases, proteases, mucopolysaccharidases, streptokinases, coagulases, DNases, etc.) that are also called toxins (exotoxins, endotoxins).
The more virulent a pathogen, the less often is it detected as a colonizing germ (“normal flora”), and vice versa.
There are four different types of pathogens:
 viruses
viruses
 bacteria
bacteria
 fungi
fungi
 protozoa.
protozoa.
Viruses
These are the smallest pathogens. A virus particle (virion) consists of genetic information (either DNA or RNA) and a protein shell (capsid). Some viruses contain additional enzymes that are required for starting the cycle of viral replication within the infected cell. For example, the herpes simplex virus (HSV) contains thymidine kinase, and the human immunodeficiency virus (HIV) contains reverse transcriptase. It is the presence of these enzymes that provides us with an opportunity for developing and using virus-specific chemotherapeutic agents.
Some viruses also possess an envelope made up of lipoproteins. For the most part, this envelope is derived from the cell in which the virus has multiplied (host cell), and the specific viral antigens have become integrated into it. Because of this envelope, these viruses (HSV, hepatitis B virus, rubella virus, HIV) are very sensitive to environmental influences, such as desiccation, alcohol-containing solvents, etc.
The structures and sizes of individual viruses are shown in Fig. 1.1.
Viruses do not have a metabolism of their own and thus depend on the enzyme systems of their host cell for replication (obligatory cell parasites).
Certain viruses can only infect cells that express the appropriate receptors (tropism); for example, HIV infects T4 lymphocytes and cells of the central nervous system, while the hepatitis B virus infects liver cells.
The host cell is normally destroyed after viral replication (lytic cycle). With certain viruses, however, the virus may also transform its host and thus gives rise to a neoplastic cell (oncogenic viruses). Certain viruses have the capacity to remain in the cell as episomes that may later result in an endogenous infection (reactivation of the virus). Especially, herpesviruses and papillomaviruses have a tendency to do this.
Viruses are usually identified by immunological methods. Because they are so small, special procedures are required to make the reaction visible (neutralization, complement fixation, hemagglutination, fluorescence test, ELISA, PCR).
Bacteria
Characteristic Features and Staining Properties 
Bacteria are the smallest pathogens with a metabolism of their own and thus can multiply on nonliving substrates. Bacteria are superficial parasites with only a few exceptions (e. g., chlamydiae, listeriae, tubercle bacilli).
Bacteria vary considerably in size, shape, and pathogenic properties.
Normally, they can be stained and viewed under a microscope. However, this does not apply, for example, to mycoplasma, which cannot be stained because they lack a solid cell wall and are highly pleomorphic. It applies only partly to chlamydiae, which can multiply only within a host cell.
A common feature of all bacteria is that they possess DNA, RNA, and ribosomes for protein synthesis. Due to their own enzymatic metabolism, all bacteria can be killed by antibiotic and chemotherapeutic agents, or their reproduction can, at least, be inhibited.
In addition to their shape, Gram staining is an important criterion for distinguishing bacteria under the microscope.
Gram-positive Bacteria 
They possess a thick, relatively rigid cell wall consisting mainly of murein (peptidoglycan), which is usually covalently bound to teichoic acid. Most gram-positive bacteria are sensitive to penicillins, with the exception of penicillinase-producing staphylococci.
Gram-negative Bacteria 
The cell walls of these bacteria are less thick but multilayered. The peptidoglycan portion is less than 10%. Instead, the cell wall also contains lipopolysaccharides and lipoproteins.
The shape of gram-negative bacteria is extremely variable, ranging from very small anaerobic gram-negative cocci (Veillonella) and small rods (Mobiluncus) to forms of variable length, such as fusobacteria.
Treatment of gram-negative bacteria is rather difficult because they have various mechanisms of resistance (primary resistance, plasmids, (3-lactamases).
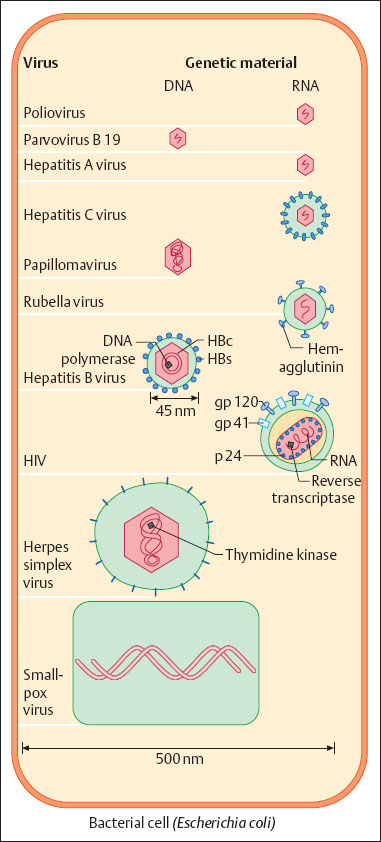
Fig. 1.1 Schematic illustration of viruses, showing their sizes in comparison with each other and with a bacterium (Escherichia coli). In part, structures are pointed out that are important for understanding either the diagnostic procedures (antigens) or the therapeutic approaches (enzymes).
Aerobic Bacteria 
Other distinguishing characteristics of bacteria are their growth requirements. We distinguish between aerobic and anaerobic bacteria.
Aerobic bacteria grow well in the presence of molecular oxygen, whereas anaerobic bacteria multiply only in the absence (< 1 %) of oxygen. With few exceptions (e.g., pseudomonads) the majority of aerobic bacteria also grow well or, even better, in an anaerobic atmosphere; they are therefore called facultative anaerobes. True anaerobes grow only in an oxygenfree atmosphere and are therefore referred to as obligatory anaerobes. There are also transitional forms.
Aerobic bacteria are the most common pathogens, and they most often cause acute infections.
Anaerobic Bacteria 
By contrast, anaerobes rather cause abscess-forming, less rapidly developing infections in soft tissues and in the abdominal region. They originate from the intestine, where synergy plays an important role.
Bacteria are usually identified by their growth requirements (substrates), colony shape on agar, metabolic functions, and microscopy. Other possible methods of distinction include antibiotic sensitivity tests, immunological methods, bacteriophage typing, biochemical analysis of the cell wall, and gas chromatography.
The doubling times of most bacteria lies between 20 and 60 minutes. It is longer for some bacteria (e. g., 24 hours for Treponema pallidum and for mycobacteria, and even 48 hours for chlamydiae), which explains why some infections take a slower course and require long-term treatment.
The most important bacteria occurring in the gynecologic region are listed in Table 1.1 according to their staining properties (Gram stain), their shape, and their growth requirements (aerobic vs. anaerobic).
Fungi
We distinguish yeasts (blastomycetes), mycelial fungi (hyphomycetes), and molds.
Yeasts (blastomycetes):
 Candida species (some of them form pseudomycelia) (Tables 1.2, 1.3)
Candida species (some of them form pseudomycelia) (Tables 1.2, 1.3)
 Malassezia furfur (causing pityriasis versicolor)
Malassezia furfur (causing pityriasis versicolor)
 Saccharomyces.
Saccharomyces.
Mycelial fungi (hyphomycetes with real ramifications), e. g., dermatophytes:
 Trichophyton rubrum
Trichophyton rubrum
 Epidermophyton floccosum
Epidermophyton floccosum
 Microsporum species.
Microsporum species.
Molds:
 Apergillus species.
Apergillus species.
The most relevant fungi for the gynecologist are yeasts and, among them, in particular Candida albicans. Candida cells are approximately five to 10 times larger than the average bacterium (Fig. 1.2). Reproduction occurs by budding, a feature that makes yeasts easy to recognize under the microscope.
Clinical infections with Candida are usually associated with yeast hyphens, i.e., pseudomycelia consisting of single elongated yeast cells. They exhibit enzymatic activities at the growing tip, and this allows them to penetrate into the deeper layers of the tissue (see Fig. 7.12, p. 73) where they bring about inflammatory reactions.
In gynecology, we are dealing only with opportunistic fungi, i.e., with pathogens that colonize the intestinal tract of up to half of the human population and cause infections and symptoms only when the body’s defenses are weakened, when antibiotics have been administered, or due to other reasons that we do not know in detail.
With the exception of flucytosine, antimycotic agents inhibit cell membrane synthesis in yeasts by disturbing the metabolism of ergosterol, through inhibition of the enzyme cytochrome P450.
Protozoa
Protozoa are unicellular organisms of the animal kingdom. They possess a typical cell nucleus, and are therefore eukaryotes. They cause various infections, such as malaria, sleeping sickness, leishmaniasis, amebic dysentery, toxoplasmosis, pneumocystosis, and giardiasis.
Trichomoniasis plays the most important role in gynecology. However, other diseases caused by protozoa may become a problem during pregnancy, for example, toxoplasmosis.
In the wake of AIDS, pneumonia caused by Pneumocystis carinii has increased in frequency.
Normal Flora
Vagina 
Lactobacilli
In the vagina, only lactobacilli are regarded as a normal flora with high bacterial counts. Reproduction of lactobacilli and selective colonization of the vagina with these germs depends on estrogen levels. Lactobacilli are therefore found during the first weeks after childbirth and then again, when the ovaries regain activity, until menopause sets in. Even in old age, high concentrations of lactobacilli in the vagina can still be found in some women, e.g., in obese women who receive medications that have a certain estrogen effect.
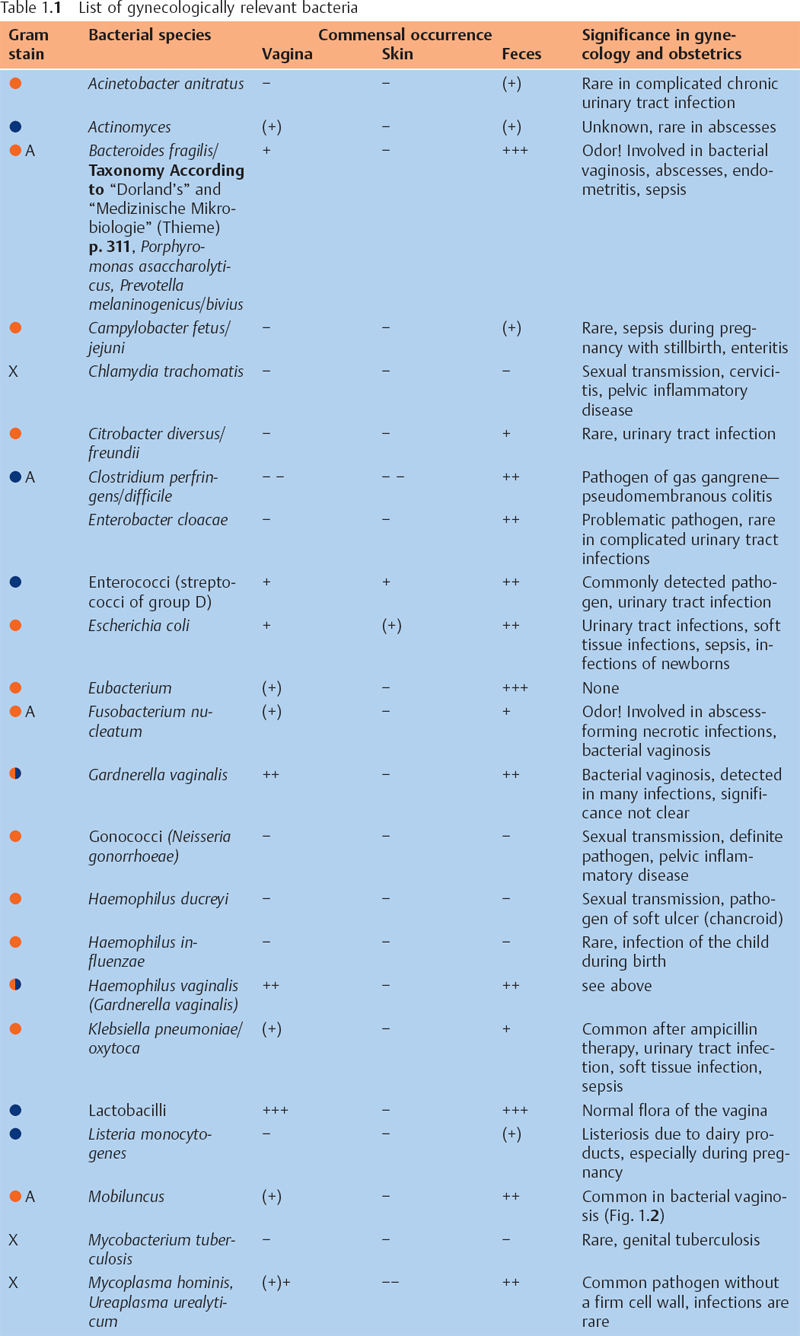
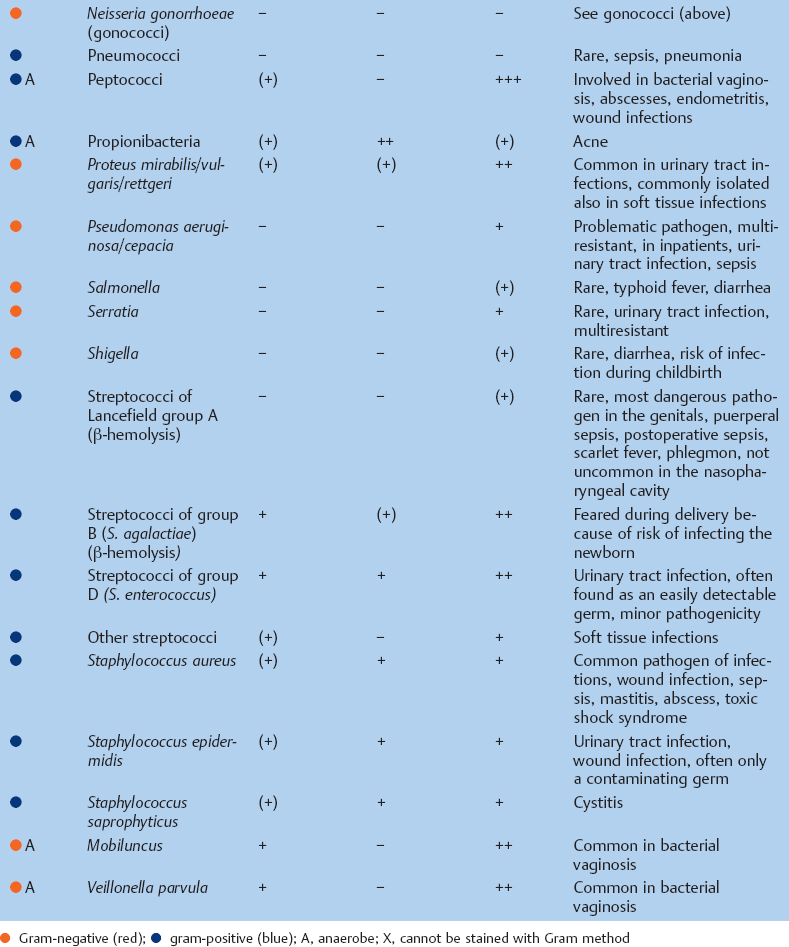
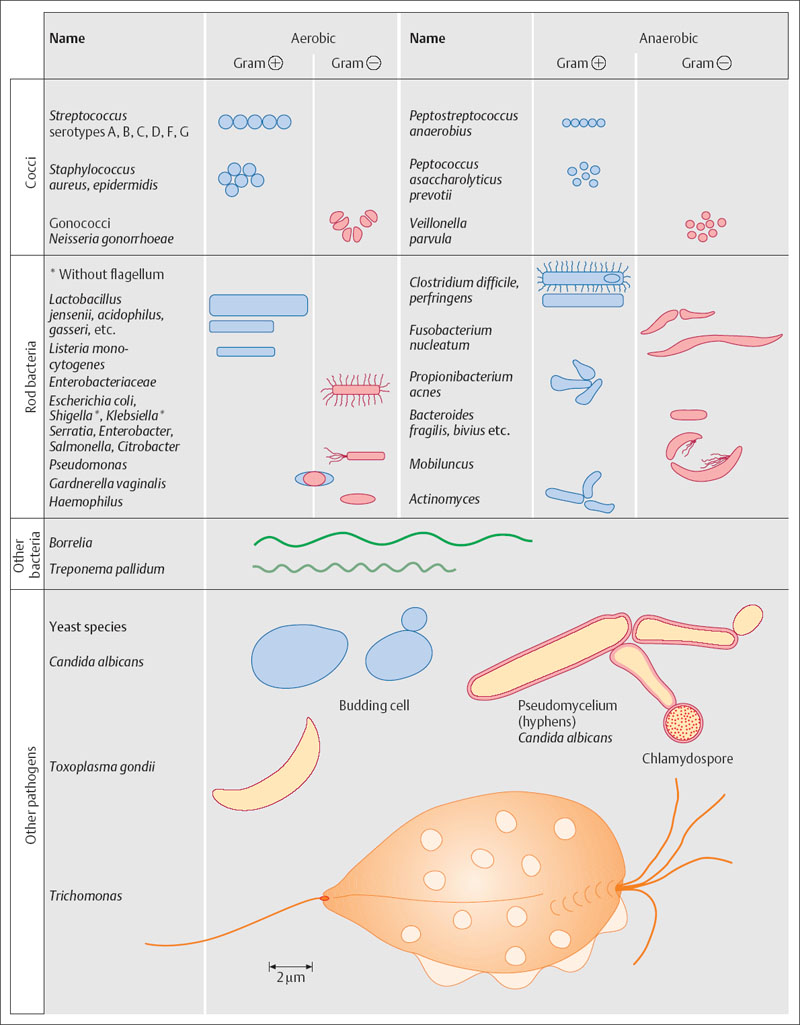
Fig. 1.2 Schematic illustration of various pathogens (bacterial species, fungi, and protozoa), comparing morphology and size. Even within some bacterial species, there may be considerable variation in morphology and size.
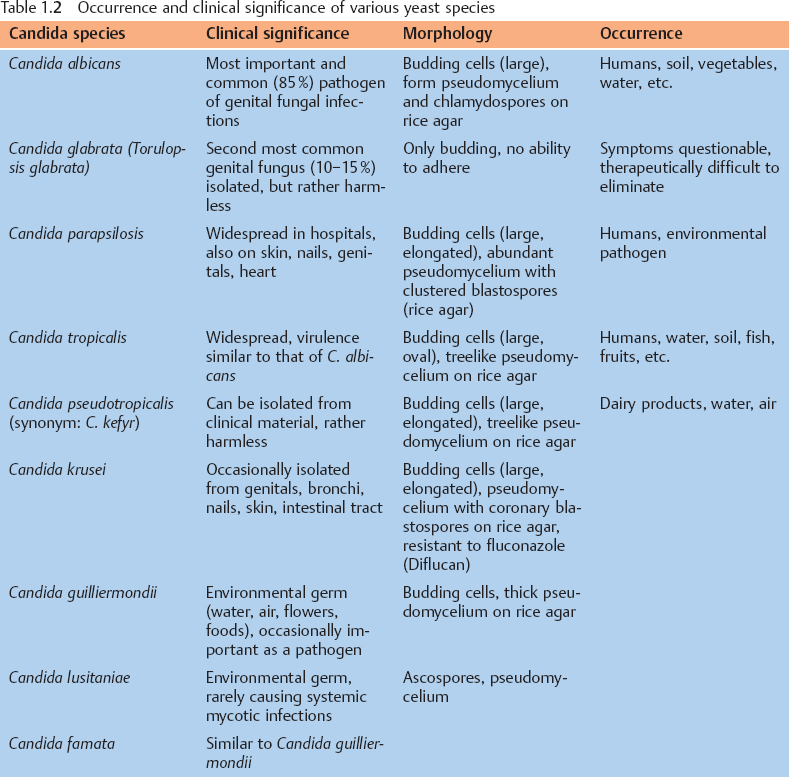
Table 1.3 Other fungal species, also for purposes of differential diagnosis
Fungal species | Characteristics |
|---|---|
Trichophyton rubrum | The most common dermatophyte, a hyphomycete, pathogen of infections on dry skin |
Saccharomyces cerevisiae | Brewer/baker yeast, nonpathogenic, only large, elongated budding cells |
Geotrichum candidum | Mold fungus, harmless, occurs in feces due to dairy products etc., forms true septate, large mycelium with arthrospores (hockey sticks) |
Rhodotorula rubra | Widespread in the environment, harmless, pink–red colonies, homogeneous budding cells, poorly developed pseudomycelium |
Trichosporon cutaneum | Hyphomycete, considered opportunistic, infests hairs |
Cryptococcus neoformans | Occurs in the soil, in AIDS patients: meningitis, lungs, abscesses |
Aspergillus fumigatus | Mold fungus, common air contaminant, aspergilloma in case of immunosuppression (Fig. 7.166, p. 167) |
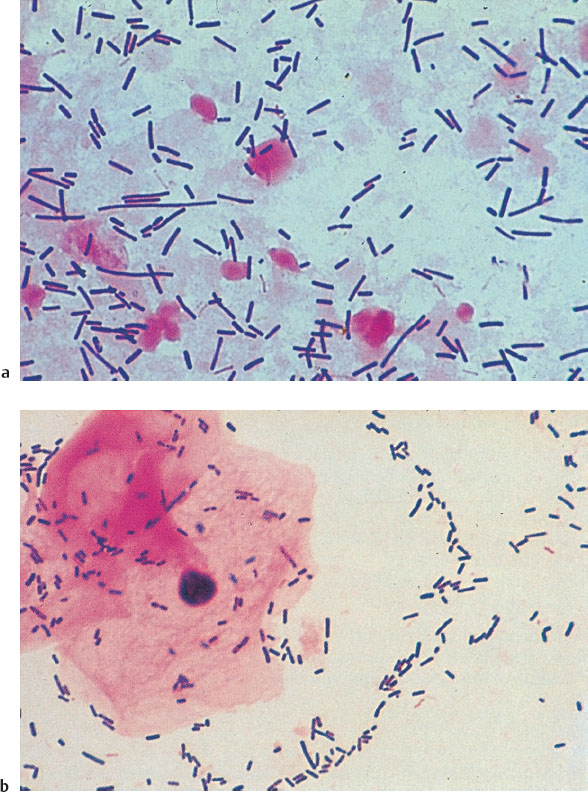
Fig. 1.3 Normal vaginal flora stained using Gram method, showing (a) large lactobacilli (Lactobacillus jensenii)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


