Chapter 391 Parenchymal Disease with Prominent Hypersensitivity, Eosinophilic Infiltration, or Toxin-Mediated Injury
391.1 Hypersensitivity to Inhaled Materials
Clinical Manifestations
Acute attacks usually occur 4-8 hr after an exposure. Symptoms include fever, chills, cough, dyspnea, myalgia, and malaise that can persist for up to 48 hr. Physical examination usually reveals an ill-appearing, dyspneic child with bibasilar crackles, wheezing, or a normal lung examination. Chest radiographs may also be normal or may demonstrate bilateral ground-glass haziness, often sparing the lung apices and bases, with fine nodulations (Fig. 391-1). These patients may progress to the subacute presentation if exposure continues or recurs. The cough worsens, dyspnea becomes more prominent, and anorexia and weight loss may occur. The chest radiograph at this stage has a more reticulonodular appearance. Long-term exposure can lead to the chronic presentation. Dyspnea and cough are severe; clubbing may be present, as are weight loss, weakness, and hypoxemia. These patients eventually develop chronic alveolitis and fibrosis that can lead to cor pulmonale. Chest radiographs show coarse reticulonodular infiltrates and bronchiectasis primarily in the upper- and mid-lung zones. High-resolution computed tomography (HRCT) scans may be more sensitive in demonstrating bronchiectasis.

Figure 391-1 Chest radiograph shows bilateral patchy alveolar infiltrate with peripheral consolidation.
(From Wubbel C, Fulmer D, Sherman J: Chronic eosinophilic pneumonia: a case report and national survey, Chest 123:1763–1766, 2003.)
Diagnosis
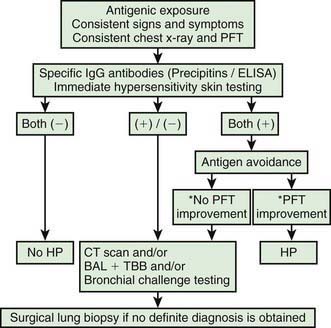
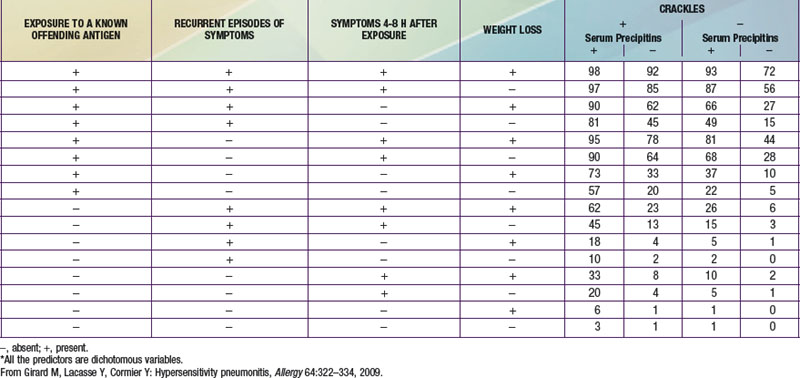
The diagnosis of HP is based primarily on the clinical presentation in association with a suspicious exposure. Because the clinical presentation is nonspecific, a high index of suspicion is crucial. Children with HP will meet most of the basic diagnostic criteria that have been proposed for adults. A variety of diagnostic criteria recommendations have been proposed. Major criteria include symptoms compatible with HP, evidence of exposure (antibody studies), compatible chest x-ray or HRCT findings, bronchoalveolar lavage (BAL) lymphocytosis, histologic changes compatible with HP, and a positive antigen provocation challenge. Minor criteria include bibasilar crackles, decreased diffusion capacity, and hypoxemia. The presence of 4 major and 2 minor criteria are very suggestive of HP, especially when other diseases with similar presentations have been excluded. A number of laboratory tests may also be helpful in confirming a strong clinical suspicion. HP patients often demonstrate a modest leukocytosis with neutrophilia with a left shift, and modest elevation of the erythrocyte sedimentation rate. Serum levels of immunoglobulins (IgG, IgM, and IgA) are often elevated. Skin testing to particular antigens lacks sensitivity and specificity, as do serum precipitins to specific antigens. Both these tests may indicate exposure but are often positive in individuals without the clinical disease. In adults, BAL fluid typically demonstrates a marked lymphocytosis (often up to 70%) particularly of the CD8+ suppressor T cells, although in children the CD4 : CD8 ratio is not increased. BAL fluid may also contain higher levels of immunoglobulins. Pulmonary function tests classically demonstrate a restrictive pattern with impaired gas exchange (diffusion capacity). The presence of a mild obstructive pattern during the acute stage is a poor prognostic indicator. Some have advocated an inhalational challenge either in the laboratory or by re-exposure to the environment. Challenge testing can be dangerous and therefore should be undertaken only in appropriately equipped diagnostic centers. A diagnostic algorithm is proposed in Figure 391-2. Table 391-1 provides criteria for estimating the probability of HP; an individual living on a farm presenting with recurrent episodes of respiratory symptoms, inspiratory crackles and testing positive for the corresponding precipitating antibodies, would have an 81% chance of having HP, while an individual with progressive dyspnea and inspiratory crackles only would have a probability of HP of less than 1%.