Chapter 251 Parainfluenza Viruses
Epidemiology
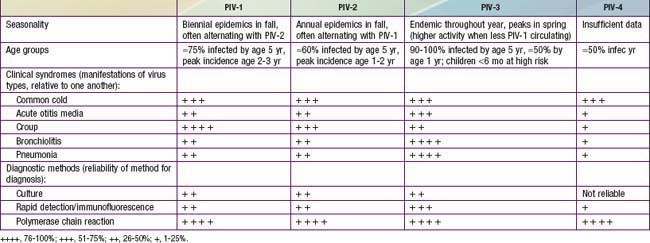
By 5 yr of age, most children have experienced primary infection with PIV types 1, 2, and 3 (Table 251-1). PIV-3 infections often occur in the first 6 mo of life, whereas PIV-1 and PIV-2 are more common after infancy. In the USA and temperate climates, PIV-1 and PIV-2 have biennial epidemics in the fall, usually alternating years in which their serotype is most prevalent. PIV-3 is endemic throughout the year but typically peaks in late spring. In years with less PIV-1 activity, the PIV-3 season may extend longer or have a second peak in the fall. The epidemiology of PIV-4 is less well defined, because it is difficult to grow in tissue culture and was often excluded from early studies.