Chapter 87 Overview of Mortality and Morbidity
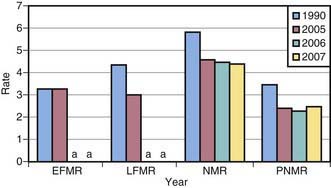
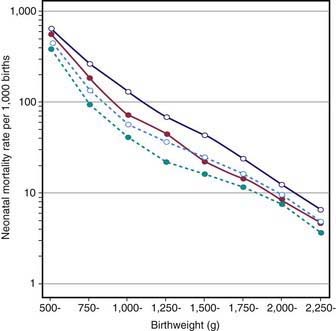
Perinatal mortality is influenced by prenatal, maternal, and fetal conditions and by circumstances surrounding delivery. Perinatal deaths are associated with intrauterine growth restriction (IUGR); conditions that predispose the fetus to asphyxia, such as placental insufficiency; severe congenital malformations; and overwhelming early-onset neonatal infections (Table 87-1). The major causes of neonatal mortality are prematurity/low birthweight (LBW) and congenital anomalies. Mortality is highest during the 1st 24 hr after birth. Neonatal mortality (4.27/1,000 in 2008) accounts for about two thirds of all infant deaths (deaths before 1yr of age). Neonatal and postneonatal mortality rates in the USA have declined or remained stable (Fig. 87-1). Factors related to the decline in mortality include improved obstetric and neonatal intensive care management with a significant reduction in birthweight-specific neonatal mortality (Fig. 87-2). Further reduction in neonatal mortality will depend on prevention of preterm delivery and LBW, prenatal diagnosis and early management of congenital anomalies, and effective diagnosis and treatment of diseases that result from adverse factors during pregnancy, labor, and/or delivery (see Table 87-1). In the USA each year, approximately 6 million pregnancies, 4 million live births, 19,000 neonatal deaths, and 28,000 infant deaths occur. Ten per cent of births are to teenage women between the ages of 15 and 19 yr, a proportion that has been decreasing for about 35 yr (Fig. 87-3). Births to girls 10-14 yr, very young mothers who are at great social and medical risk, declined substantially over this period. The proportion of deaths to unmarried women was 40.6% in 2008, the highest ever in U.S. history.
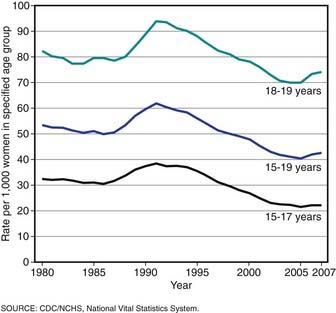
Figure 87-3 Birthrates for teenagers by age, USA, final for 1980-2006 and preliminary for 2007.
(From Hamilton BE, Martin JA, Ventura SJ: Births: preliminary data for 2007, Natl Vital Stat Rep 57:12:1–23, 2009.)
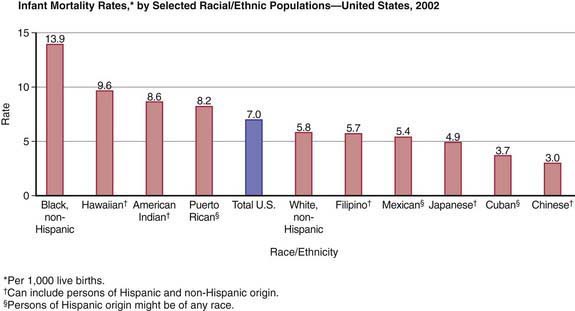
The LBW rate (infants weighing ≤ 2,500 g at birth each year) in the USA increased from 6.6% to 8.2% between 1981 and 2008, whereas the very low birthweight (VLBW) rate (infants weighing ≤1,500 g at birth) increased from 1.1% to 1.46% of all births. In the past decade, LBW has increased among white infants, mainly because of a rise in the number of multiple births (often associated with assisted reproduction) (Fig. 87-4). Nonetheless, LBW and VLBW rates remain highest among black infants. Reasons for the racial disparity in LBW remain unclear. Despite advances in prenatal and obstetric care, racial disparity in birthweight persists, thus suggesting the need for novel prevention programs. Furthermore, although preterm LBW survival is better among black neonates (see Fig. 87-2), overall neonatal and infant mortality rates remain highest among blacks (Fig. 87-5), even for infants born to extremely low-risk mothers (married, aged 20-34 yr, ≥13 yr of education, adequate prenatal care, no medical risk factors, no alcohol or tobacco use during pregnancy). A reduction in the racial disparity in mortality is an important public health issue reflected in Healthy People 2010, the U.S. national health objectives for the year 2010.
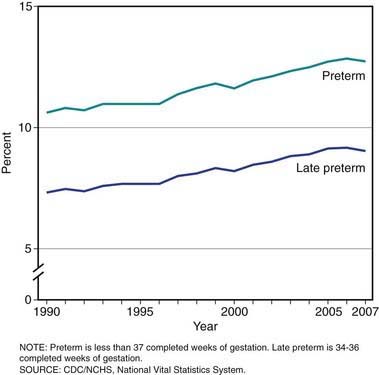
Figure 87-4 Preterm birthrates, USA, final for 1990-2006 and preliminary for 2007.
(From Hamilton BE, Martin JA, Ventura SJ: Births: preliminary data for 2007, Natl Vital Stat Rep 57:12:1–23, 2009.)