CHAPTER 13 Outcomes of treatment for neonatal brachial plexus palsy
Summary box
Introduction
The first description of brachial plexus palsy during the birth process can be traced back to the year 1768 by William Smellie.1 In 1872, Duchenne published his gross description of an upper nerve root lesion,2 followed by the classic description of upper brachial plexus palsy by Erb in the year 1874.3 Although Erb was not the first to describe this condition, he was the first to localize the lesion to the junction of the fifth and sixth nerve roots and to describe the effect of nerve stimulation at Erb’s point.3 In 1885, Augusta Klumpke described the lower brachial plexus palsy, and she experimentally localized the cause of the associated Horner’s syndrome to injury of the white rami communicantes of C8, and especially the T1 nerve root.4
Early treatment of brachial plexus palsy consisted of physical therapy while awaiting spontaneous recovery. The first descriptions of surgical reconstruction of the brachial plexus were published by Kennedy in 19035 and Taylor in 19076. These reports were followed by other reports that demonstrated limited results and significant morbidity, leading to a predominantly conservative approach until the 1980s.7–9 Interest in surgical treatment for neonatal brachial plexus palsy (NBPP) was revived after the publication of satisfactory outcomes by Gilbert in 1984.10
Outcome evaluation
The British Medical Research Council (MRC) scale is a 6-point (0–5) power scale commonly used for adults; however, infants cannot participate in testing that requires voluntary demonstration of full power. Therefore, some authors have developed measurement scales that depend on active range of motion for assessment of the paretic or paralyzed limb. Such is the case in the muscle grading system of Gilbert and Tassin, which considers the presence or absence of movement with and without the effect of gravity. The scale is simple, easy to apply, and widely recognized. However, since it must include a wide range of movements within only 4 possible grades (M0–M3), discriminatory capability is not one of its strengths. Furthermore, the scale has not yet been subjected to validation studies.7 The Mallet classification described in 197211 is commonly used to evaluate global function of the upper extremity. Although it has limited applicability in infants, this classification system does provide a reasonable assessment of upper limb function in older children.
In our practice, we use the Hospital for Sick Children Active Movement Scale (AMS) (Table 13.1), which has been subjected to validation studies and has demonstrated consistent intra-rater reproducibility and inter-rater reliability among physiotherapists having a wide range of experience.12 It is an 8-point scale that addresses range of motion for a specific joint in the presence and absence of gravity. It is designed to be highly discriminatory in detecting minor as well as major changes in movement. In using this scale, a full range of gravity-eliminated movements must be achieved (grade = 4) before the movement can be scored against gravity (grade 5 or above). Other advantages of this scale include its ability to grade movement within the entire upper extremity and that it does not require the child to perform specific tasks on command, allowing it to be used in early infancy.7
Table 13.1 The active movement scale
| Observation | Movement grade |
|---|---|
| Gravity Eliminated | |
| No contraction | 0 |
| Contraction, no motion | 1 |
Motion ≤  range range | 2 |
Motion >  range range | 3 |
| Full motion | 4 |
| Against Gravity | |
Motion ≤  range range | 5 |
Motion >  range range | 6 |
| Full motion | 7 |
From Clarke HM, Curtis CG. An approach to obstetrical brachial plexus injuries. Hand Clin 1995; 11:563-80.
Other reports exist that describe joint-specific outcome scales such as the Gilbert elbow paralysis scale13 (Table 13.2) which assign positive points for elbow flexion and extension and negative points for any extension deficit, giving an outcome described as poor, average, or good recovery. The Raimondi and Gilbert hand and wrist classification13 (Table 13.3) is a specific classification of hand recovery ranging from stage 0 indicating complete paralysis, to stage 5 with good wrist and finger flexion and extension and full pronation/supination.
Table 13.2 Gilbert elbow paralysis scale
| Evaluation | Points | |
|---|---|---|
| Flexion | Nil or some contraction | 0 |
| Incomplete flexion | 2 | |
| Complete flexion | 3 | |
| Extension | No extension | 0 |
| Weak extension | 1 | |
| Good extension | 2 | |
| Extension defect | 0 to 30° | 0 |
| 30° to 50° | −1 | |
| >50° | −2 |
0–1 point = poor recovery, 2–3 points = average recovery and 4–5 points = good recovery
Table 13.3 Raimondi/Gilbert hand and wrist classification
| Stage I | Complete paralysis or slight finger flexion of no use; useless thumb; no pinch; some or no sensation |
| Stage II | Limited active flexion of fingers; no extension of wrist of fingers; possibility of lateral thumb pinch |
| Stage II | Active extension of wrist with passive flexion of fingers (tenodesis); passive lateral pinch of thumb (pronation) |
| Stage III | Active complete flexion of wrist and fingers; mobile thumb with partial abduction & opposition; intrinsic balance; no active supination; good possibilities for palliative surgery |
| Stage IV | Active complete flexion of wrist and fingers; active wrist extension; weak or absent finger extension; good thumb opposition with active ulnar intrinsics; partial prosupination |
| Stage V | Hand IV with finger extension and almost complete prosupination |
Natural history
Many reports with various study designs and patient populations exist in the literature to describe the natural history of NBPP, some including a combination of spontaneously recovered patients and patients who underwent surgical reconstruction. Pondaag et al.14 presented a systematic review of the literature from 1966 to 2001 to clarify the natural history of untreated NBPP. They identified 4 inclusion criteria for good quality studies: (1) prospective study design; (2) study population should be constituted on a demographic basis, avoiding potential bias toward severe cases in reports based on referral to specialized centers; (3) sufficiently long and complete follow-up; (4) an accurate and reproducible assessment of final recovery with no surgical intervention. Only 7 articles met 2 inclusion criteria and 35 articles met 1 criteria; no article was found to meet 3 or 4 of the inclusion criteria. Therefore, these authors concluded that the often-cited excellent prognosis for NBPP cannot be considered to be based on scientifically sound evidence.
DiTaranto et al.15 reported on 91 infants born with NBPP at one institution in Argentina from 1994 to 2000. The only treatment offered was physical and occupational therapy, and early microsurgical reconstruction was unavailable to any of these children. All children were examined every 3–4 months and minimal follow-up was 2 years (range, 2–5 years). Documentation of muscle power using the MRC scale was done for critical marker muscles (deltoid, biceps, triceps, and wrist extensors). None of the patients with global palsy (N = 12) had greater than M1 deltoid or biceps strength at 6 months, and all had extensive limitation and minimal functional use of the limb at long-term follow-up. Infants with typical Erb’s palsy (N = 63) who had regained biceps and deltoid power of M4–M5 at 4–6 months resulted in having no significant limitation in hand and wrist function and only mild limitation in range of motion of the shoulder. The last group (N = 16) was infants with upper brachial plexus palsy who only had minimal recovery (M1–M2) of deltoid and biceps strength at 6 months of age, and at final evaluation, these children had persistent deformities and functional limitations.
The number of infants who recover from NBPP is variably reported to be from 69–95%.16 Some of these studies defined recovery as improvement to a good functional outcome that could not be improved further by surgical intervention, yet others defined recovery as normal neurological findings with no weakness in the affected limb. Evans-Jones et al.17 reported the incidence and documented the outcome at 6 months for infants with NBPP in the United Kingdom and Republic of Ireland. Out of 323 confirmed cases, 52% of infants had full neurological recovery; all of these infants had upper brachial plexus palsy (C5,6 +/-C7). Forty-six percent had partial recovery, and 2% had no recovery (all with complete brachial plexus palsy). Noetzel et al.16 prospectively followed 94 infants with monthly examinations, 7 patients were lost to follow-up and another 7 were excluded because of surgical intervention. Fifty-three infants (66%) had complete recovery, all of whom had antigravity movement of the biceps, triceps, and deltoid by 4.5 months with a normal examination at 15 months. Nine infants (11%) had only mild persistent weakness, all having antigravity movement in the same 3 muscles at 6 months. In the remaining 18 patients, 7 had moderate persistent weakness affecting mainly the deltoid muscle (MRC grade 2). All had antigravity biceps and triceps function, but no antigravity function was seen in the deltoid at 6 months of age. The other 11 patients with severe weakness in the deltoid and biceps or wrist and fingers had a maximum MRC grade 2 in deltoid, biceps, and triceps muscles at 6 months of age.
Michelow et al.9 reported that 92% of 66 infants recovered spontaneously to such a degree that surgery was not indicated; these authors determined that elbow flexion at 3 months incorrectly predicted recovery in 12.8% of cases. Combining the scores of elbow flexion with scores for elbow, wrist, finger, and thumb extension incorrectly predicted recovery in only 5.2%.
Waters18 reported on 66 infants with NBPP seen within the first 3 months of life with subsequent monthly examinations. All infants who recovered biceps function by the first month of life had no residual neurological deficit at final follow-up examination. He also documented the outcome of 39 patients who did not have recovery of biceps function by 3 months of life; in these patients, 18 had a grade 4 shoulder abduction on the Mallet scale, and 10 had grade 4 hand-to-mouth range of motion at time of final follow-up. On subgroup analysis, he concluded that the final outcome for patients who recovered biceps function at 4 months is comparable to the outcome of patients who underwent surgical repair for absent biceps function at 6 months of age. Similar findings documenting good outcome in selected patients who did not recover biceps function by 3 months have been published by other authors.19–21
Outcome of surgical treatment
Patients referred to the brachial plexus clinic at the Hospital for Sick Children are seen on presentation and a thorough clinical history and a detailed examination are obtained. Follow-up is provided every 3 months with repeated examinations. Our indications for surgical intervention at 3 months of age are a Test Score of 3.5 or less out of a possible 10, presence of Horner’s syndrome, or clinical evidence of T1 avulsion. The Test Score is calculated by converting the active movement scores for 5 specific joint motions (elbow flexion and elbow, wrist, finger, and thumb extension) to numeric scores using a standard formula (Table 13.4), and then summing these numeric scores to calculate the total Test Score. At 9 months, our indication for surgery is inability to pass the cookie test.7,12 In Erb’s palsy, we give priority to restoration of elbow flexion and shoulder movement. In total palsy, priority is given to restoring hand function by targeting the entire lower trunk with the best available donor.
Table 13.4 Active movement scale conversion for use in calculating test score
| Movement grade | Converted score |
|---|---|
| 0 | 0 |
| 1 | 0.3 |
| 2 | 0.3 |
| 3 | 0.6 |
| 4 | 0.6 |
| 5 | 0.6 |
| 6 | 1.3 |
| 7 | 2.0 |
From Clarke HM, Curtis CG. An approach to obstetrical brachial plexus injuries. Hand Clin 1995; 11:563–580.
Our approach since 1993 has been to resect all neuromas (regardless of whether or not the neuroma shows evidence of conduction by intraoperative electrodiagnostic studies), if no distinct fascicular pattern is seen on intraoperative exploration. We previously demonstrated that despite an initial decrease in overall movement at 6 weeks postoperatively, movement returns to baseline by 3 months postoperatively following neuroma resection,22 this demonstrated that the neuroma does not contribute significantly to overall function of the limb and can be discarded safely.
In 1996, we reported the short-term outcome for 16 patients with NBPP who had neurolysis as the complete treatment for conducting neuromas-in-continuity. At 1-year follow-up, neurolysis in Erb’s palsy improved both the muscle grade and the functional ability of patients. Neurolysis did not provide useful functional recovery in patients with total brachial plexus palsy.23
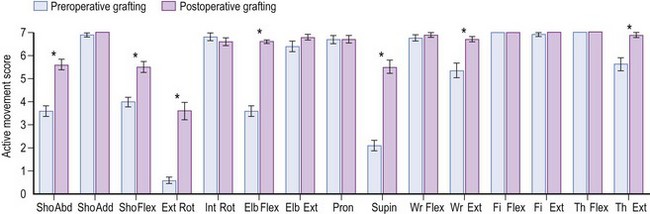
We recently reviewed our long-term outcome (minimum of 4 years follow-up) in patients having brachial plexus exploration from 1991 to 1999 at the Hospital for Sick Children.24 A total of 108 patients were reviewed; 16 underwent neurolysis of conducting neuromas-in-continuity (the same patients studied by Clarke et al.23), and 92 had neuroma resection and nerve grafting at a mean age of 7.9 months (48 with Erb’s palsy and 44 with total palsy). For the Erb’s palsy group undergoing neurolysis alone, a significant increase in active movement scores was seen only for supination, with no increase in the proportion of patients achieving functionally useful scores (6 or 7 on the active movement scale). In contrast, Erb’s palsy patients undergoing neuroma resection and nerve grafting demonstrated a statistically significant increase in active movement scores for 7 movements (Figure 13.1) and a significant increase in the proportion of patients with functionally useful movements for the same 7 movements (shoulder abduction, flexion, and external rotation, as well as elbow flexion, supination, wrist extension, and thumb extension) (Figure 13.2). For the total brachial plexus palsy patients undergoing neurolysis of neuroma-in-continuity, significant improvement in elbow flexion, supination, and extension of the fingers and thumb were noted but again, without a significant increase in the proportion of patients achieving a functionally useful movement. In comparison, the total brachial plexus patients undergoing neuroma resection and grafting showed significant improvement in 13 joint movements (Figure 13.3), with a significant improvement in the percentage of patients achieving functionally useful movement in the following 11 movements: shoulder abduction, adduction, flexion and external rotation, elbow flexion, supination, wrist flexion, wrist extension, finger flexion, finger extension, and thumb extension (Figure 13.4).
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree