Fig. 1
A Mckie splint is a prefabricated soft splint that helps to support the thumb in abduction for improved functional grasp
In some cases, a child may not tolerate the rigidity of a thermoplastic orthotic or the care team may desire for the child to have increased support at a joint without complete immobilization of the joint. In these instances, neoprene may also be the material of choice. For example, a child with substantial ligamentous laxity and chronic wrist pain who consistently has pain with writing and poor CMC joint stability may experience less pain when using a neoprene wrist and thumb spica orthotic. Benik® (Silverdale, WA) is a vendor that makes a wide selection of prefabricated and custom-sized neoprene orthotics in pediatric sizes. Other vendors make neoprene orthotics that are available in adult sizes that may fit children nearing skeletal maturity.
Types of Upper Extremity Orthotics and Casts
When considering what type of orthotic or cast to prescribe, it is helpful to consider what purpose the orthotic/cast will serve. If orthotics are needed to optimize function of the upper extremity, the role of the orthotic is typically either to provide increased stability or to assist with active range of motion. Orthotics to support the interphalangeal (IP) joints, metacarpophalangeal (MCP) joints, and thumb carpometacarpophalangeal (CMC) joint and/or wrist are the most common styles of orthotics used for the purpose of providing stability at a joint or multiple joints for improved function in cases where there is no neurologic involvement. Table 1 above outlines the most common styles of orthotics used for improving hand function by providing increased joint stability and the various material options for the orthotics. The specific styles of orthotics use for improving function by either providing joint stability or assisting active range of motion when nerve injury is presented are in Table 3.
Table 1
Orthotics for joint stability for improved function
Orthotic style | Structures immobilized | Material options |
|---|---|---|
Short opponens orthotic | First CMC joint and thumb MCP | Thermoplast, neoprene, neoprene with thermoplastic insert |
Wrist and thumb spica | Wrist and first CMC joint and thumb MCP | Thermoplast, neoprene, neoprene with thermoplastic insert or neoprene with metal stay |
Volar based | ||
Radial based | ||
Wrist immobilization orthotic (or wrist cock-up orthotic) | Wrist | Thermoplast, neoprene, neoprene with thermoplastic insert, or neoprene with metal stay |
Volar | ||
Dorsal | ||
Figure of eight orthotics | Distal interphalangeal (DIP) or proximal interphalangeal (PIP) joints | Oval-8, thermoplast, silver ring orthotics |
Pediatric occupational therapists may also use an orthotic, such as a resting hand orthotic, or a cast (Fig. 2) to constrain the unaffected upper extremity for the purpose of improving hand function in children with hemiplegia (Aarts et al. 2010). This is typically performed in cases where a child has sustained an injury to the peripheral nervous system resulting in upper extremity impairment, such as an obstetrical brachial plexus birth palsy (Abdel-Kafy et al. 2012), or when an insult to the central nervous system has resulted in unilateral upper extremity impairment such as cerebral palsy (Huang et al. 2009). With constraint-induced movement therapy, the therapist applies a cast or an orthotic to the unaffected upper extremity to facilitate increased use of the impaired upper extremity. A variety of protocols for constraint therapy exist ranging from application of a cast that is not removable to application of a constraint cast or orthotic for a specified amount of time or set of activities on a regular basis (Huang et al. 2009).


Fig. 2
A cast can be placed on the unaffected extremity to promote increased functional use of an affected upper extremity with a constraint-induced movement therapy protocol
Orthotics that are used for protection (Figs. 3 and 4) of the upper extremity after an injury or surgery must be designed to include the specific structures that should be immobilized for healing. Often these orthotics are fabricated out of thermoplastic materials so that they have the rigidity necessary to provide the degree of immobilization adequate to promote continued healing of the injured or surgically repaired structures. Similarly, orthotics that are being used to provide pain relief are constructed to immobilize or position the upper extremity to allow inflamed structures to rest. Table 2 below provides an overview of the most common orthotics used to promote healing.



Fig. 3
An ulnar gutter splint includes the ring finger and small finger in safe position and wrist in neutral to slight hyperextension

Fig. 4
A finger gutter splint serves to immobilize one digit. It can be donned with Velcro straps as shown or using tape
Table 2
Common orthotics used to promote healing
Orthotic style | Structures immobilized | Variations |
|---|---|---|
Ulnar gutter | Fourth and fifth digits with MCPs in 50–70° of flexion and IPs extended; wrist is in neutral to 15° of extension | Hand based: most proximal end is just distal to the wrist flexion crease |
Forearm based: wrist included in neutral to 15 degrees of extension | ||
Third finger included: referring provider may request that the orthotic is extended radially to include the third digit | ||
Finger gutter | Can include one or multiples the following joints of: DIP, PIP, MCP of one digit | Sometimes the clinician will extend a finger gutter splint to be hand based in children with small hands to facilitate the splint staying on |
Radial gutter | Second and third digits with MCPs in 50–70° of flexion and IPs extended; wrist is in neutral to 15° of extension | Hand based: most proximal end is just distal to the wrist flexion crease |
Forearm based: wrist included in neutral to 15 degrees of extension | ||
Resting hand | Wrist (neutral to 15–20° of extension) and digits (extension or 10–15° arc of digit flexion) and thumb (palmar abduction) | The thumb may be omitted if the nature of injury/surgery does not require immobilization of thumb |
Safe position: MCPs are positioned in 50-70 degrees of flexion and IPs are in full extension. Indicated when prolonged immobilization is desired so that collateral ligaments of MCPs do not tighten | ||
Thumb spica | Wrist in 0–15° of extension; thumb in palmar abduction with IP free | Hand based: the wrist is not included |
IP included: the IP joint of the thumb is immobilized | ||
Dorsal blocking orthotic | MCPs included in safe position (50–70° of flexion); IPs in neutral extension; wrist in neutral | This splint may be modified in several ways: |
• Hand based or forearm based | ||
• PIP extension may be blocked to prevent full PIP extension | ||
• Specific digits may be excluded from the splint (such as the index finger) to allow greater function if the precautions allow for this | ||
Wrist immobilization | Wrist in 0–15° of extension and neutral deviation | Volar based |
Dorsal based: allows palm of hand free for greater sensory input to the hand |
Orthotics may be used to limit deformity in cases of neurologic impairment (Langlois et al. 1989), either that of the central nervous system affecting the upper extremity or peripheral nerve impairment in the upper extremity. Table 3 outlines those orthotics most often used with peripheral nerve injury. In cases where there is an upper motor neuron injury causing abnormal muscle tone in the upper extremity, the most effective orthotic design to limit deformity is usually that which includes all structures contributing to the loss of range of motion (Figs. 5 and 6). The clinician must carefully assess the joint mobility to determine the presence of tendon tightness and/or joint tightness and assess which muscle/tendon groups should be placed on stretch with the orthotic design. Finally, in cases of severe tissue trauma, such as a burn (Feldmann et al. 2008) or Volkmann ischemic contracture, positioning in an orthotic may serve to limit contracture and deformity.



Fig. 5
This is a Benik elbow splint. It is made of neoprene with a moldable thermoplastic insert so that the splint may be positioned to match the child’s positioning need

Fig. 6
This is a Benik resting hand splint made from neoprene with a moldable thermoplastic insert. The splint may be molded by the therapist to achieve the desired position of support
Orthotics or casts may be used to improve joint range of motion in cases where tissue tightness limits range of motion (Bhat et al. 2010; Lucado and Li 2009). In cases where therapists apply orthotics to improve joint mobility, consultation with the referring provider is recommended to ensure that the range of movement is not limited by a bony block or joint incongruity. Therapists may employ one of several orthotic/cast interventions with the goal of improving joint range of motion:
1.
Serial static orthotics: When serial static orthotics are employed to improve joint mobility, a static splint, such as a finger gutter splint or elbow extension splint, is fabricated to position a stiff joint at its end range. The static splint is then serially remolded over a series of therapy sessions into increased joint range until the desired passive range of motion is achieved or a plateau occurs. Often static orthotics are worn at nighttime to allow the child movement during the daytime (Schultz-Johnson 2002). Serial static orthotics are a good option in cases where the child is returning for regular therapy visits since the splint must be adjusted by the therapist to achieve a greater stretch. Because they are simple in design and lack movable components, they do not pose considerable safety risks when used with children.
2.
Static progressive orthotics: “Static progressive splinting is the use of inelastic components – such as hook and loop tapes, static line, progressive hinges, turnbuckles, screws, and gears – to apply torque to a joint in order to statically position it as close to end range as possible and thus increase passive range of motion (Schultz-Johnson 2002). With a static progressive orthotic, the principal of tissue elongation through low load and prolonged stretching is applied to improve joint mobility (McClure et al. 1994). Therapists may custom fabricate static progressive orthotics (Fig. 7) or use either prefabricated orthotics (Fig. 8). Static progressive orthotics may be prescribed to be worn anywhere from three 30-min sessions per day (Doornberg et al. 2006) to as much as 23 h per day (Schultz-Johnson 2002).
3.
Dynamic orthotics: Dynamic splints (Fig. 9) employ elastic components, such as rubber bands or springs, to provide a passive assist to joint motion or mobilize a stiff joint (Schultz-Johnson 2002). Both prefabricated and custom fabricated styles of dynamic orthotics are options. When dynamic orthotics are being used for the purposes of increasing joint mobility, they are worn for a specified amount of time to achieve a sustained stretch. They can be removed between wearing periods to allow for range of motion exercises and/or functional use of the upper extremity.
4.
Serial casts: Serial casts (Fig. 10) may be applied to be worn without removal until the next therapy visit or they can be bivalved so that they may be removed and worn for a portion of each day or night. Serial casts may be used to decrease joint tightness that limits mobility after a trauma such as a stiff PIP joint lacking extension (McClure et al. 1994). They may also be used to reduce joint contractures in the upper extremity that have resulted from spasticity in conditions such as cerebral palsy (Pohl et al. 2002).
The decision as to which style of orthotic to use for increasing joint mobility is complex in nature. A variety of factors guide the therapist and care team in determining which orthotic design might be the best for a particular child. The therapist should obtain a thorough assessment of the child’s tolerance for orthotics, ability to wear an orthotic for the advised wearing schedule, caregiver support, skin integrity, and ability to follow directions for monitoring orthotics and performing necessary adjustments to orthotics to determine if any of the above orthotic options is appropriate for the child.
Therapy Evaluation for Orthotics
Occupational Profile
Gathering the appropriate information from the child and family is essential in choosing the appropriate orthotic (Hanna and Rodger 2002). It is important to realize that each child has unique needs that require thought and clinical judgment from the therapist. When the purpose of the orthotic is for function rather than protection, an occupational profile or a client/family interview is beneficial in determining the right orthotic for that child/family (DeGrace 2003). Some of the common questions to keep in mind while evaluating the patient are:
What is the goal of the orthotic (e.g., is it to limit deformity or improve function during a particular task)?
What are the occupations (e.g., student, athlete, musician, etc.) of the patient?
Is this a long-term or short-term option?
Will the child benefit more from a daytime wearing schedule or nighttime?
What is a realistic wearing schedule for the child, considering developmental stage and occupations?
The occupational profile will provide the therapist greater insight to the specific needs of each individual child, their goals, and the context in how the orthotic will be helpful in their lives.

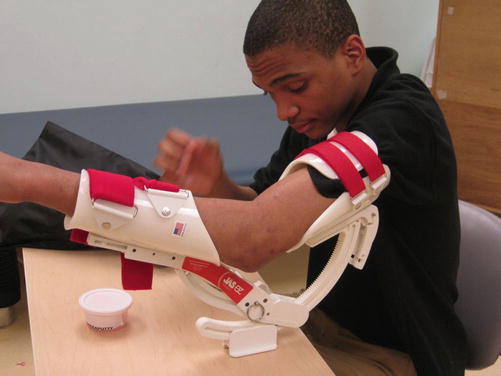



Fig. 7
This is a custom-molded static progressive PIP flexion splint for the middle finger. The turnbuckle on the volar surface of the splint allows the splint to be serially adjusted into increased PIP flexion as the child is able to tolerate an increased stretch
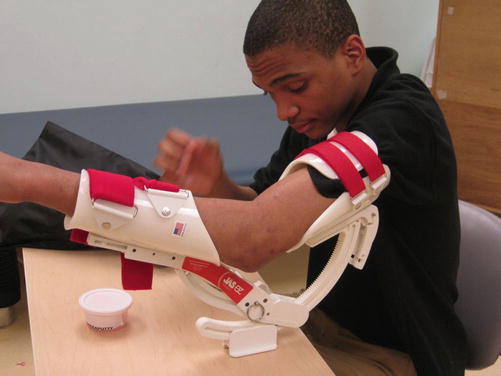
Fig. 8
The JAS elbow splint is a prefabricated static progressive elbow splint that may be used for improving elbow flexion or elbow extension

Fig. 9
Prefabricated dynamic splints may be used during the daytime to improve PIP extension

Fig. 10
Casts, such as this elbow extension cast, may be applied serially in an increased stretch to improve range of motion when a child has persistent joint tightness
Health Status
The child’s health status typically has a substantial impact on the appropriate orthotic style. The child’s health status informs the therapist of what precautions must be considered when choosing an orthotic and may also provide information as to how the child may be able to tolerate the orthotic. The child’s health status may include their diagnoses, previous surgeries, and current or previous therapies. Skin integrity is an important factor of a child’s health status. Newborn and younger children may have more sensitive skin than teenagers. It is not uncommon for a child to have sensitive skin that breaks into rash easily. A good question to ask the caregivers is whether the child sweats excessively or often. Too much moisture may lead to skin breakdown. Discomfort can lead to difficulty with tolerating the orthotic and poor compliance. The patient may have extensive regimental care that may affect the wearing schedule of the orthotic. These considerations will factor into the wearing schedule and the type of orthotic material that is chosen. In order for a patient and family to be compliant with orthotic wear, it must be tolerated by the child and fit into their daily routine (Callinan and Mathiowetz 1996).
Level of Function
It is important to assess the child’s current level of function. The child’s level of function will help you to determine if he or she will be donning/doffing the orthotic independently or if they will need assistance from a caregiver. Additionally, the child may be able to take off the orthotic and may attempt to do so rather than wearing it as prescribed. These factors may affect the overall design and wearing schedule of the orthotic (Ho et al. 2010).
When recommending an orthotic to improve function, it is beneficial to observe the child complete tasks while wearing the orthotic and without the orthotic (Goodman and Bazyk 1991). Sometimes this can be done with sample orthotics, taping, or with the patient’s previous orthotic. In other cases, it can only be done once the orthotic has been donned on the child. Often a patient’s positioning may be improved in an orthotic; however, function may be compromised. For example stabilizing a wrist may impede a tenodesis grasp. In some instances, several orthotics are trialed before deciding upon the optimal orthotic. Sometimes, the therapist determines it is best to not use an orthotic (Frohlich et al. 2012).
Goals/Outcome Measures
Many therapists find it beneficial to use a formal assessment tool to gather information about a child’s functional abilities and limitations. A frequently used tool is the Canadian Occupational Performance Measure (COPM) (Case-Smith 2003; Dedding et al. 2004). Other outcome measures may also be used (see chapter, “Outcome Measures”). Outcome measures are useful tools in determining how the patient’s function is affected by his or her diagnosis and whether an orthotic is indicated to help improve function. The COPM may also be helpful to determine the patient’s and family’s goals. Often a patient will come to the evaluation with the goal of having the same orthotic that he or she has always had. Sometimes after reviewing the outcome measure, it is discovered that a different orthotic may be more suitable. Outcome measures can be readministered at a later date to determine the effectiveness of the orthotic.
Orthotics for Specific Conditions
Congenital Differences
Children with congenital differences may benefit from upper extremity orthotics to improve function, limit deformity, or provide protection following surgical reconstruction of their upper extremity. The most common congenital differences for which orthotics are used include longitudinal differences, camptodactyly, thumb hypoplasia, and preaxial (radial) polydactyly. Orthotics are also used in the treatment of amniotic band syndrome with associated nerve compression and congenital clasped thumb. Less commonly, orthotics are used with syndactyly releases.
Longitudinal Deficiency: Radial and Ulnar
When children have a radial or ulnar longitudinal difference, a wrist immobilization orthotic may be used to prevent a fixed wrist radial or ulnar deviation contracture, respectively. The wearing schedule of a wrist immobilization orthotics for a child with an untreated longitudinal difference depends on whether or not the child is more functional when wearing a wrist orthotic that aligns their wrist in more neutral deviation. When children achieve greater function with their wrist positioned by an orthotic, then day wear of the orthotic is recommended. Kennedy (Kennedy 1996) found that children experienced increased functional use of their affected upper extremity when wearing a neoprene wrist support (Fig. 11). Furthermore, older children being treated with a neoprene wrist orthotic reported a preference for the neoprene orthotic over prior wrist orthotics fabricated from thermoplastic materials. When children will not tolerate wearing an orthotic during the day, night wear of the orthotic to provide a sustained stretch into neutral alignment is used to prevent a fixed deviation contracture. If a child has a wrist centralization procedure, a wrist immobilization orthotic for supporting the wrist in neutral alignment is employed once the child completes an adequate period of immobilization in a postsurgical cast. A circumferential (a.k.a. clam shell) style orthotic and an ulnar gutter with radial return (in the case of radial longitudinal deficiencies) are commonly used styles of orthotics to maintain neutral wrist alignment. Goldfarb et al. (2011) outlines a protocol of wearing the orthotic at all times except for AROM and light play until 6 months out from surgery and then transitioning to night wear until skeletally mature.


Fig. 11
Therapists may fabricate soft neoprene wrist supports such as the one depicted to support neutral wrist alignment
Camptodactyly
Conservative treatment of congenital camptodactyly is the standard of practice since “surgical results are uniformly disappointing (Goldfarb et al. 2011).” Resolution or reduction of the PIP flexion contracture maybe achieved through serial static extension orthotics (Benson et al. 1996; Bonhomme et al. 2013). Bonhomme et al. (2013) used night orthotics with serial adjustments for increased extension and found it took an average of 7 months for 62 % of subjects to achieve full PIP extension and 38 % to achieve PIP extension of −10° or better. In this study, an extension orthotic with the MCP and wrist held in neutral or slight extension was used.
Surgical intervention is reserved for only those cases which do not respond favorably to conservative intervention (Benson et al. 1996). When surgical reconstruction is performed, serial orthotics or casts prior to surgery may help to lessen the joint contracture and lengthen tight tissues prior to surgery (McFarlane et al. 1992). Once the pin is pulled after surgical reconstruction, an extension orthotic is worn continually for 2 weeks, and then transition to a night orthotic is suggested. Night orthotics are continued for 3–6 months following surgery (McFarlane et al. 1992). Alternatively, Goldfarb et al. (2011) use a protocol of wearing a hand-based or forearm-based orthotic at all times except for hygiene and ROM exercises from 2 to 6 weeks after surgery and then switching to night orthotic that is continued until 12 weeks out from surgery or longer if an extension lag persists. They also use a dynamic extension orthotic during the day beginning at 6 weeks post-op if a considerable lag in extension is present.
Thumb Hypoplasia
With thumb hypoplasia, Blauth type I and II, orthotics that support the thumb in palmar abduction can improve function for activities requiring gross grasp or palmar pinch grasp. Typically soft neoprene styles of orthotics are adequate to provide this level of improved function. A wrist and thumb spica orthotic is used in the postoperative rehabilitation of children who undergo surgical management of a hypoplastic thumb, either a pollicization or thumb reconstruction. While timing of transition from a postoperative cast to an orthotic can vary, it most often occurs 4–6 weeks following surgery. Continual orthotic wear aside from hygiene, AROM, and light functional activities/play is used for 2–4 weeks following surgical reconstruction, and a night orthotic is continued until 3 months out from surgery (Goldfarb et al. 2011).
Preaxial Polydactyl
When a child undergoes surgical reconstruction of their thumb for preaxial polydactyly , the child is transitioned from the postoperative cast to a thumb spica around 4 weeks following surgery. Initially, the orthotic is worn at all times except for hygiene, range of motion exercises, and supervised light functional use of the hand. Six weeks following surgery, the child can be transitioned to a night wearing schedule that is continued up to 3 months from surgery if the child is at risk of developing a first webspace contracture (Goldfarb et al. 2011).
Congenital Clasped Thumb
Orthotics have shown to be an effective intervention for resolving grade I congenital clasped thumbs without an associated soft tissue contracture (Lin et al. 1999; Tsuyuguchi et al. 1985). Lin et al. (1999) describes a protocol of using a short opponens orthotic that holds the thumb in MCP extension and radial abduction, while Tsuyuguchi et al. (1985) used a forearm-based orthotic with the thumb MCP and IP joints in neutral and the CMC in abduction. Both found that with full-time wear of the orthotic, it took 3–6 months for the child to achieve consistent active MCP extension of the thumb. They also both continued with night orthotics for an additional 1–3 months.
When surgical reconstruction of a clasped thumb is necessary, the child is placed into a forearm-based thumb spica orthotic after pins are pulled. Goldfarb et al. (2011) recommends the child wears the orthotic with the thumb supported in radial and palmar abduction at all times aside from hygiene, range of motion exercises, and light functional use or play until 2 months following surgery. Their protocol involves continuing with the orthotic at night until the child is 3 months from surgery. Tsuyuguchi et al. (1985) initiated nighttime orthotics only once pins are pulled and continued with night orthotics until the child was 6 months from surgery.
Amniotic Band Syndrome
Amniotic band syndrome may result in a child having motor loss from a band compressing a peripheral nerve (Kozin 2005). In such cases, upper extremity orthotics may be part of the treatment plan used to preserve joint mobility until active movement is restored. Because orthotics are employed when the child is newborn, a forearm-based resting hand orthotic is most effective. If the radial nerve is involved, the MCP joints and wrist are positioned in extension and thumb in radial deviation. If motor function of the ulnar and/or median nerve is affected, then the MCPs should be placed in 60–70° of flexion with the IPs extended to prevent a claw deformity.
Syndactyly
Orthotics are not typically necessary following a syndactyly reconstruction, unless the surgery involves the first webspace. When surgical revision occurs in the first webspace, a c-bar (Fig. 12) or thumb spica with a c-bar is used to maintain the first webspace once the postoperative dressing is removed (Coombs et al. 1994). Typically, a nighttime wearing schedule is adequate and is continued until 3–6 months out from surgery (Goldfarb et al. 2011). If the child is not actively moving the thumb into abduction and opposition regularly with functional use of the affected, then orthotics may be used during the day as well.


Fig. 12
A first webspace c-bar splint may be used when the depth of a webspace needs to be maintained
Therapists may use a resting-hand-style orthotic as the base of support for an elastomer scar pad that is worn at nighttime when a syndactyly reconstruction involves a webspace other than the first. Using a highly perforated orthotic material as a base for moldable elastomer products allows for a custom-formed elastomer scar pad to be securely affixed to an infant or toddler’s hand following surgery, decreasing the choking risk posed by a scar pad.
Customized Functional Orthotics for Children with Congenital Differences
Pediatric hand therapists may be called upon to design orthotics to allow a child with an upper extremity congenital difference to participate in specific activities. Figure 13 is an example of an orthotic designed to assist a child with symbrachydactyly in riding a bicycle. While children with congenital differences in their upper extremities are quite adept at achieving functional goals, anatomical differences, such as asymmetrical limb length or underdeveloped digits, may impede children in a few very specific activities. In such cases, therapists employ activity modifications, which may include uniquely designed orthotics to allow a child to use specific tools.


Fig. 13
Children with congenital impairment or other conditions that impact their ability to use an upper extremity for a particular activity may require a customized splint to facilitate participation in a desired activity. The above is a splint made so that a child with a congenital impairment could ride his bike
Peripheral Nerve Injury
When children experience trauma affecting a peripheral nerve, the pattern of motor loss is specific to the level of nerve injury and specific nerve(s) involved. Table 3 outlines the styles of orthotics employed in providing care to children recovering from a peripheral nerve injury. While these are the typical styles, therapists take into consideration the patient’s functional abilities and limitations, speed of recovery, and patient/family preferences and resources when determining the best option for each specific child.

Table 3
Orthotics for peripheral nerve palsies
Nerve involved | Pattern of motor impairment | Recommended orthotics |
|---|---|---|
Radial nerve | Absent or weakened: wrist extension, MCP extension, and thumb radial abduction | Benik® radial nerve orthotic; Robinson InRigger (adult sizes only); P-1 blocker immobilization orthotic with MCPs and wrist in extension wrist |
Median nerve (high lesion) | Absent or weak: pronation, wrist flexion, digit flexion of the PIPs and DIPs of the IF and MF, thumb palmar abduction and opposition, thumb flexion | Thumb spica with thumb in palmar abduction |
Median nerve (low lesion) | Absent or weak: thumb palmar abduction and opposition | Thumb spica with thumb in palmar abduction or short opponens orthotic |
Ulnar nerve | Absent or weak intrinsic muscles resulting in claw positioning of RF and SF | Anticlaw orthotic (Fig. 14) for SF and RF (note: if the child also has median nerve injury, the claw deformity will be present in the index, middle, ring, and small finger and the anticlaw orthotic should include all four digits) |

Fig. 14
Anticlaw splints position the MCPs in flexion and facilitate IP extension. They can be designed to include the ulnar two digits for an ulnar nerve palsy or all four digits in case of an ulnar nerve and median nerve palsy
If the nerve does not fully return, then the child may undergo tendon transfers to regain motor function lost from the nerve injury. A child must have good passive joint mobility prior to tendon transfers. If contractures are present, orthotics or serial casting may be used to achieve improved joint mobility prior to surgery. Following at tendon transfer, the child is typically casted for 4–6 weeks and then they may be transitioned to a protective orthotic. The design of the protective orthotic should be such that the joints are positioned to keep the all-transferred muscle groups in a shortened position to prevent overstretching the transfer (Skirven et al. 2011). Once the child has learned to activate the transfer independently to achieve the desired joint movement, then the orthotic may be transitioned to night wear only. This typically occurs around 2 months postoperatively. After the transfer is strengthened and the child is using the transfer regularly during functional tasks, the night orthotic may be discontinued.
Brachial Plexus Palsy
Children may have an obstetrical brachial plexus palsy or sustain a traumatic brachial plexus injury. The pattern of motor and sensory impairment with brachial plexus palsies follows the distribution of injured nerve roots or trunks. Often, in the initial period following a lesion to the brachial plexus, the child will require a resting hand orthotic to prevent contractures of the wrist, digits, and first webspace (Eng et al. 1996).
When recovery is incomplete, children may undergo surgical intervention, such as nerve or tendon transfers. In such cases, orthotics may be used in the postoperative rehabilitation plan to protect the extremity. The specific style of orthotic used depends on the type of procedure performed. The therapist and surgeon should collaborate to determine the best orthotic design to provide the necessary protection and support to the upper extremity during the postoperative recovery stage. When splints are necessary following surgery, they are typically implemented 4–6 weeks following surgery.
It is common for children who have sustained an obstetrical brachial plexus to develop an elbow flexion contracture during the recovery process. The use of botulinum toxin type A combined with a 4 week serial casting protocol has been found to be effective in improving elbow extension (Basciani and Intiso 2006).
Tetraplegia
Children with tetraplegia resulting from a spinal cord injury (SCI) may have orthotic needs that vary depending on where they are in the recovery process and the level of their spinal cord injury. In early phases of rehabilitation, orthotics may be necessary to limit joint contractures as the child is experiencing autonomic storming. Elbow extension orthotics and/or resting hand orthotics are the most common needs during this time. As the child’s acute stage of healing stabilizes, children may continue to benefit from orthotics to prevent deformity as well as orthotics to optimize function. However, because tenodesis grasp and/or lateral pinch are compensatory grasp patterns used by children with SCI, clinicians must carefully assess that the orthotic being considered to improve function does not actually impede functional grasp patterns. When the level of SCI is incomplete, recovery may occur for several months past the injury. Once motor and sensory return plateau, a child may be a candidate for reconstructive surgery to maximize their upper extremity function (Waters et al. 1996; Hamou et al. 2009).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


