Orthospinology: A Specific Upper Cervical Approach for Pediatric Care
Julie Mayer Hunt
The importance of the upper cervical spine in the pediatric patient cannot be overstated. Numerous publications, authored by chiropractic and medical doctors alike, document the impressive response to upper cervical adjustments for a myriad of conditions. Notable among them are common childhood disorders such as otitis media, colic, constipation, torticollis, nocturnal enuresis, attention deficit hyperactivity disorder, tonsillitis, and sinusitis. Other conditions such as seizures, skull deformities, breast-feeding difficulties, kinematic imbalance, and sleep disorders have also been established. In the medical literature, Gutmann (1) and Biedermann (2) document a high incidence among infants for upper cervical subluxations or “atlas blockage,” while Gottlieb (3) relates birth trauma to neurological dysfunction including cranial nerve deficits. Because the birthing process is a primary cause of upper cervical subluxations, and because subluxations induce such profound complications, all infants should be examined for upper cervical misalignments while neonates. For further study, The Upper Cervical Subluxation Complex by Dr. Kirk Eriksen (4) provides an exhaustive source for numerous abstracts regarding adult and pediatric upper cervical research.
Chiropractic Orthospinology is a specific approach to the successful management of the entire spine. Based on the work of John F. Grostic, D.C., the procedure incorporates three primary radiographs to determine a precise vector to facilitate the correction of the occipito-atlantal-axial subluxation complex. These three films are analyzed to quantify, in degrees, the malposition of C1 and C2 relative to the center of the skull, as well as the unique architecture of the patient’s upper cervical spine and any deviation of the lower cervical spine. These findings mathematically establish the adjustment vector, which is measured via a coordinate system with the thrust applied to the atlas transverse process with the patient in a side lying position. The Orthospinologist may then choose one of three adjusting methods to deliver the gentle force to the transverse process of the atlas vertebrae: the original hand adjustment using a pisiform contact setup on a Grostic adjusting table, a handheld adjusting instrument (currently, the model KH2), or a table-mounted adjusting instrument, called the Orthospecific. The light force adjustment is perfectly suited for the pediatric population, using under 1 lb of force, and the handheld adjusting instrument incorporates a variety of small styli ideal for the smaller pediatric neck. Orthospinology Procedures, An Eυidenced-Based Approach to Spinal Care, by Eriksen and Rochester (5) provides a complete step-by-step review of Orthospinology procedure protocols.
While the need to be as specific as possible is of great importance in an area of the spine with such significant neurological implications, producing quality radiographs of neonates and toddlers can be extremely difficult. However, given a thorough understanding of the anatomy and biomechanics of the pediatric spine, Orthospinology principles may be applied to facilitate the correction of the upper cervical spine when radiographs are not feasible, with positive outcomes. This chapter presents an overview of pediatric Orthospinology with emphasis on the unique anatomy and biomechanics of the pediatric spine, upper cervical subluxation patterns, and the clinical assessment of postural distortions. Straightforward and modified procedures regarding x-ray placement and adjusting methods are presented with supporting case studies.
ANATOMY AND BIOMECHANICS OF THE OCCIPITOCERVICAL JUNCTION IN A NEWBORN
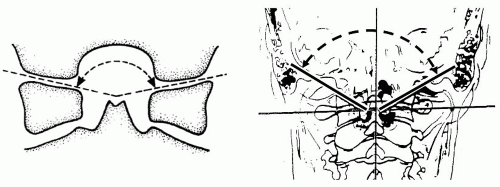
To accomplish upper cervical corrections in the pediatric patient, considerations must be given to the unique anatomy of the developing spine. The pediatric spine is differentiated from the adult spine in several significant ways. The angles of the pediatric spinal joints have articulating surfaces, depicted in Figure 32-1A, which are flatter and more horizontal when compared to the occipitoatlanto articulation of a mature child or adult as shown in Figure 32-1B. Note that the frontal angle of C0-C1 in children is not as easy to measure because the cartilaginous tissue is much thicker during the first years.
In a study by Biedermann (6), “more than 1,000 x-rays from the first year of life were reviewed and found to have an almost horizontal plane of the frontal angle of the occipito atlanto articulation.” As the child matures, these angles increase with age as do the facet angles of the lower cervical joints as depicted in Figure 32-2. Owing to the thickness of the cartilaginous beds in the young pediatric spine, the adjustment vectors calculated by standard Orthospinology protocols are not as varied. Subluxation patterns become increasingly complex as the joints ossify and become more angular especially related to Y-axis rotation.
Stability of the upper cervical region is achieved by soft tissue inclusive of the tectorial membrane, the alar, apical, and cruciate ligaments, as well as the anterior and posterior musculature. In the pediatric spine, the greatest degree of mobility occurs at C2-C3. The hypermobility is due in part to capsular and ligamentous laxity and increased elastic properties. The hypermobility is also complicated by the weight of the pediatric head and the underdeveloped musculature. The odontoid is separated from the C2 body and neural arches by a broad cartilaginous band that does not ossify until the child reaches 3 to 6 years of age. Furthermore, as in the adult population, the spinal segments
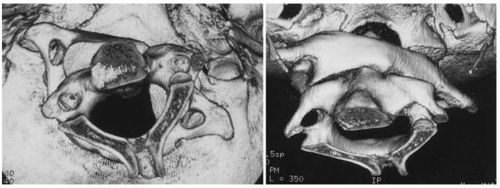
from C2-C3 to L5-S1 incorporate locking facet joints aided by the Joints of Luschka in the cervical spine and the mammillary processes in the lumbar spine. The occipito-atlantal-axial complex has articular beds without boney interlocking facets increasing the potential for biomechanical subluxations and/or dislocations resulting in compensating spinal fixations as the body maintains balance. Figure 32-3 depicts an example of the potential mobility of the upper cervical spine.
from C2-C3 to L5-S1 incorporate locking facet joints aided by the Joints of Luschka in the cervical spine and the mammillary processes in the lumbar spine. The occipito-atlantal-axial complex has articular beds without boney interlocking facets increasing the potential for biomechanical subluxations and/or dislocations resulting in compensating spinal fixations as the body maintains balance. Figure 32-3 depicts an example of the potential mobility of the upper cervical spine.
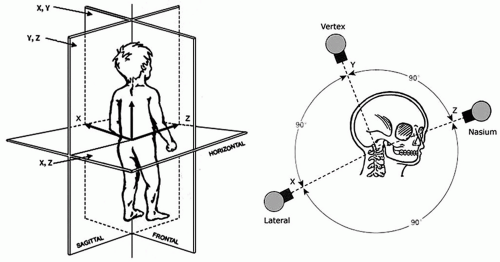
A thorough understanding of the biomechanical patterns of the upper cervical misalignment is paramount to establish consistent spinal corrections. As the pediatric spine ossifies, the specificity of the adjustment vector becomes increasingly complex. Therefore, as soon as x-rays in 3 dimensions can be obtained – the lateral, nasium, and vertex series – an accurate vectored adjustment can be performed. Figure 32-4 depicts the three angles utilized for the radiographs required for the Orthospinology analysis. The neutral lateral cervical
film is taken to assess the general structure and pathology of the cervical spine and to provide the angle necessary to expose the nasium film. The vertex view is taken perpendicular to the transverse plane of the atlas to measure C1 rotation, while the nasium view provides assessment of any lateral deviation of the central axis of the skull, the atlas, and the lower cervicals, as well as the rotation of C2 and the slope of the C0-C1 and C1-C2 articular surfaces. The analysis produces angular measurements to quantify, in degrees, the relative deviation from normal of the above components. These factors are computed to calculate the specific adjustment vector. A detailed explanation of these x-ray views and analysis is provided in the Orthospinology Procedures (5) textbook.
film is taken to assess the general structure and pathology of the cervical spine and to provide the angle necessary to expose the nasium film. The vertex view is taken perpendicular to the transverse plane of the atlas to measure C1 rotation, while the nasium view provides assessment of any lateral deviation of the central axis of the skull, the atlas, and the lower cervicals, as well as the rotation of C2 and the slope of the C0-C1 and C1-C2 articular surfaces. The analysis produces angular measurements to quantify, in degrees, the relative deviation from normal of the above components. These factors are computed to calculate the specific adjustment vector. A detailed explanation of these x-ray views and analysis is provided in the Orthospinology Procedures (5) textbook.
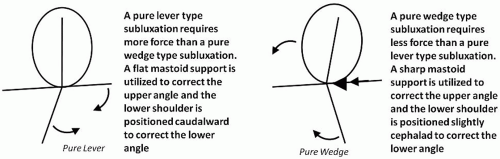
In a gravitational field, the weight of the head on the spinal column is an important biomechanical factor to be considered to understand upper cervical subluxation patterns. There are four basic patterns of cervical misalignment recognized in the orthogonal approach for the upper cervical region. The two primary patterns are the pure lever and pure wedge patterns (Fig. 32-5). Simply stated, the adjustment vector is unique to the type of correction required. If the head is to be moved on top of the C1 vertebra, a wedge-type adjustment (low line of correction) is utilized; if the C1 vertebra is to be moved under the skull, a lever-type adjustment (high line of correction) is required. The pediatric application of these biomechanical principles will be discussed.
SUPINE LEG LENGTH ASSESSMENT
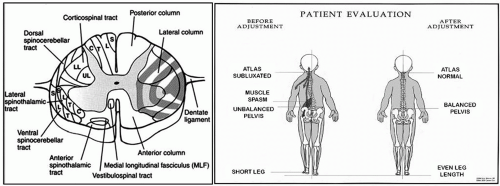
The supine leg length assessment is the primary examination observation used by orthogonally based upper cervical practitioners for more than 50 years. While most chiropractic procedures place the patient in a prone position, upper cervical practitioners examine pelvic imbalance with the patient supine on a firm surface. In the pediatric population, apparent leg length asymmetry is usually readily apparent for discrepancies of ¼ to ½ in. Greater discrepancies may indicate anatomical abnormalities or hip pathologies. Dr. Kirk Eriksen (4) notes the following regarding the apparent or functional short leg theory: “the spinocerebellar tracts are located along the lateral edge of the spinal cord and are located at the most probable site of maximal mechanical irritation via the dentate ligaments. The proprioceptive tracts are primary pathways for regulating muscle tone and joint position sense. The spinocerebellar tracts are arranged in a laminar fashion (although somewhat angulated) with the most lateral fibers innervating the most caudal structures (i.e., legs, sacral, lumbar, thoracic, cervical [very limited]). Irritation of these tracts could lead to muscle tone imbalance of the pelvic girdle resulting in a functional short leg.” Figure 32-6 (left) depicts the proximity of the dentate ligaments to the peripheral spinal cord tracts and how the dentate ligament tension may distort their form and function. This may represent a lateral and rotational upper cervical subluxation complex and has been demonstrated on upright MRI. The concept of leg length asymmetry is shown graphically in Figure 32-6 (right).
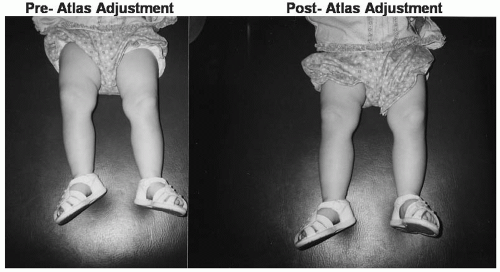
A supine leg length examination as shown in Figure 32-7 is an invaluable assessment especially when used in conjunction with palpation of the associated paraspinal erector spinae musculature. Indeed, in the absence of pelvic discrepancy, the upper cervical region is considered to be normal and no adjustment is given. When the supine leg check is performed, the entire lower extremity is observed. With early toddlers, observation of skin folds bilaterally as well as foot and ankle differences should be assessed. For infants younger than 6 months, leg length asymmetry may be difficult to determine; therefore, palpation of the erector spinae muscles is performed as a secondary evaluation method. Utilizing shoes will improve accuracy as they establish a straight line for better evaluation.
In infants 6 months or older (Fig. 32-8), it is helpful to stabilize the legs at the knee with the doctor’s thumb placed on the patella. Care must be taken to apply equal pressure to both knees especially if the infant or toddler is squirming on the table. Unequal skin folds above the knee (Fig. 32-9) may indicate unequal pressure and yield a false leg length assessment.
PEDIATRIC TABLE PLACEMENT
The Orthospinology adjustment is accomplished using a side posture patient placement on a specialized headpiece to facilitate a stable mastoid support with the adjustment side up. With infants, a thin receiving blanket can be used on the headpiece to minimize the child’s reaction to the adjusting surface. The patient is placed in a neutral position with the cervical spine level and thoracic and lumbar spine parallel to the adjusting table as shown in Figure 32-10.
The mastoid is placed 1/8 in. superior to the caudal edge of the specialized Orthospinology headpiece to provide the critical solid mastoid support. Care should be taken not to fold the ear lobe so as to alleviate possible pinching. The head should not be rotated and the infant’s parent can help aid stability by holding the
patient’s legs in a slightly flexed position while maintaining eye contact. Distracting the infant may be necessary utilizing a noisy toy or set of keys.
patient’s legs in a slightly flexed position while maintaining eye contact. Distracting the infant may be necessary utilizing a noisy toy or set of keys.
 FIGURE 32-9 Toddler Leg Check. Left: Correct leg stabilization. Right: Incorrect leg stabilization signified by unequal skin folds. |
THE KH2 ADJUSTING INSTRUMENT
Unique to all other upper cervical adjusting procedures, Orthospinology provides the chiropractor with a variety of adjusting methods:
The original hand adjustment using a pisiform contact
A handheld adjusting instrument, originally called the Laney instrument, now known as the KH2 instrument (Fig. 32-11)
A table-mounted Orthospecific adjusting instrument
For the pediatric population, the KH2 is ideal to adjust the small contact area and versatile enough to accommodate a toddler prone to move at any moment. The force of the instrument can be regulated to <1/2 lb of pressure and a variety of styli are available making this method perfectly suitable for the pediatric patient.
MODIFIED X-RAY PLACEMENT WITH A TODDLER
When necessary, the Orthospinology x-ray series can be obtained with assistance from a lead-shielded parent when an accurate adjustment vector is required. It is essential that each visit is a positive experience for the toddler to ensure consistent cooperation in subsequent visits. With a child under 2 years of age, multiple visits may be required with only one film taken during each visit. If the child reaches meltdown mode, a sticker, toy, or other positive reinforcement is used to regroup for the next visit. Autistic cases often require this type of repetitive reinforcement to achieve quality x-rays though at no time should the child’s behavior allow a poor-quality film to be exposed. Having an older child “pose” for a fake x-ray may also encourage cooperation from a wary toddler. Obtaining the lateral, vertex, and nasium views on a toddler with assistance from a shielded parent is illustrated in Figure 32-12. The parent may need to hold the child’s hands down and away from exposure during the exam. The vertex view is the most challenging and may require several visits to procure a quality film. Note the stuffed animal placed above the child and the mother holding down the hands. In the nasium setup, notice the mother has not changed position from the vertex view and is able to secure the child’s hands while the doll is used to encourage the child’s cooperation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree