Operative Delivery by Vacuum
The first recorded attempt at vacuum-assisted vaginal delivery occurred in 1694, by Dr. James Younge, a physician at Portsmouth Naval Hospital in Plymouth, England. His records demonstrate that he had been called to the bedside “to deliver…a woman four days in labor…and I could neither fasten a crochet nor draw it out by a copping-glass fixt to the scalp with an air pump.” The principle of cupping was regularly used in that epoch to elevate depressed skull fractures. Younge’s attempt at vacuum-assisted vaginal delivery was unsuccessful. A century later Saemann (1794) published a paper stating, “I saw in a dream an air pump wherewith one can seize the head of an infant without injury to mother or child. The pump was made of brass and had a covering of rubber with ventilators” (MacCahey, 1890). Unfortunately, no actual deliveries are described. In 1829, Neil Arnott advocated the use of a pneumatic tractor in his text Elements of Physics or Natural Philosophy. Interestingly, Arnott wrote that the tractor “seems peculiarly adapted to a purpose of obstetric surgery, viz., as a substitute for steel forceps in the hands of men who are deficient in manual dexterity, whether from inexperience or natural ineptitude.” Again, there were no actual deliveries recorded with such a device.
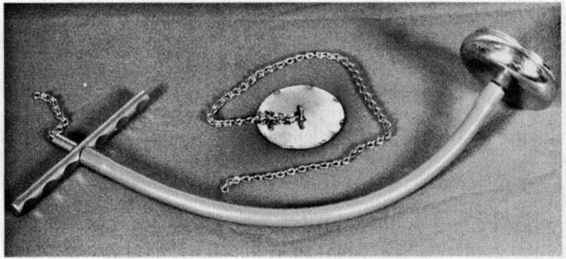
A leading innovator in obstetric history is credited with the first successful vacuum-assisted vaginal delivery. James Young Simpson of Edinburgh, Scotland, who popularized the use of chloroform for labor analgesia and who developed the forceps that bear his name, is credited with performing the first successful series of vacuum-assisted vaginal deliveries in the 1840s. In a manuscript entitled On a suction tractor; or New mechanical power, as a substitute for forceps in tedious labours, Simpson described a metallic vaginal speculum that was fitted with a piston with the broader trumpet-shaped end covered with leather and greased with lard. This end was applied to the fetal scalp and the piston was withdrawn so as to create a vacuum (Simpson 1849; Fig. 7-1). Writing in the London Medical Gazette (1849), Simpson stated, “I have now employed it repeatedly in cephalic and pelvic presentations, and both when the head was already high above the brim and already sunk into the pelvic cavity.” The London Journal of Medicine sounded a note of caution and, in an editorial, stated, “We much fear that this proposed substitute for the forceps may only lead to disappointment. We almost dread the infant’s scalp being torn off or a parietal bone dragged out. … We must wait to see it fully tested in practice.” For unknown reasons Simpson abandoned his air-tractor but continued to concentrate on his forceps (Chalmers 1963).
FIGURE 7-1. The “suction-tractor” as described by James Young Simpson. Vacuum was created by pulling back on the plunger. (Adapted from Laufe and Berkus, 1992, with permission.)
MacCahey described and patented two vacuum devices in 1890. The first of these was a cup constructed of soft rubber, which was attached to a rigid handle. This device was pushed against the fetal head, which created a vacuum when traction was applied, much in the same manner as a commode plunger. The second device consisted of a metallic cup, which was attached to a vacuum pump in a manner very similar to modern designs.
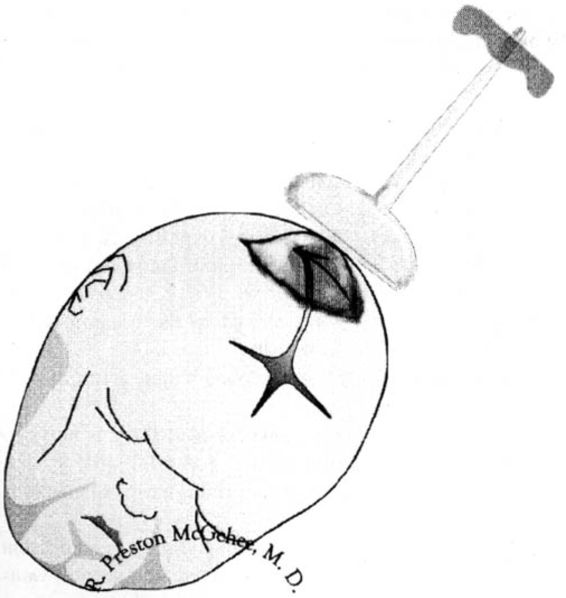
In 1954, Malmstrom introduced a metal cup, which he termed a “vacuum-extractor.” The original Malmstrom vacuum-extractor consisted of a mushroom-shaped stainless steel cup with a smooth inverted lip and an outside diameter of 60 mm (Fig. 7-2). The vacuum extractor was originally used not only for traction to assist delivery, but it was also attached to the fetal scalp before full cervical dilatation in an effort to overcome dystocia. Vacuum cups of smaller diameters were designed for use in the first stage of labor. The vacuum-extractor was considered to be a simpler instrument and to require less anesthesia than the obstetric forceps.
FIGURE 7-2. Photograph of the Malmstrom device showing the metal cup, handle, and chain. The metallic disk with the attached chain fits inside the metal cup and prevents the fetal scalp from being pulled into the vacuum port.
The Malmstrom vacuum extractor was also introduced in the United States but received mixed reviews. Earn (1967) reviewed the obstetric literature with regards to the Malmstrom vacuum device and forceps, and concluded that maternal morbidity and perinatal deaths were lower with vacuum delivery. There was, however, a higher incidence of scalp trauma with the vacuum extractor than with the forceps. Other reports of the Malmstrom vacuum extractor also noted favorable results (Tricomi, 1961; Kelly, 1962; McCullough, 1963; Pauly, 1963; Nyirgesy, 1963; Barth, 1965; and their many colleagues). Matheson and coworkers (1968) published a case series of 168 procedures without significant maternal complications, a 2 percent incidence of fetal cephalohematoma, and an overall perinatal mortality rate of 18/1000.
Vacuum-assisted vaginal delivery did not become popular in the United States, however, probably in part because of reports of fetal complications. The vacuum device was often associated with scalp abrasions, and the edematous area of the scalp raised by the device (the chignon) was cosmetically unpleasant (Fig. 7-3). Several groups (Aguero, 1962; Ahuja, 1969; Plauche, 1979; and their colleagues) reported life-threatening neonatal complications of vacuum extraction. Ott (1975) pointed out that the women in the report of Ahuja (1975) were poor candidates for the vacuum extraction procedure secondary to very prolonged labors.
FIGURE 7-3. The chignon is the area of edematous scalp that is raised by the vacuum extractor cup. Typically, it recedes a few hours after birth.
These reports of poor neonatal outcomes led to refinements in technique. Wider and associates (1967) limited the use of the vacuum extractor to the second stage of labor and suggested that the device should be used for no more than 15 minutes to minimize adverse perinatal impact. In a retrospective study, Greis and colleagues (1981), using the Bird modification of the Malmstrom device, demonstrated that neither perinatal mortality nor serious neonatal injury were more likely, as compared to forceps or cesarean section, when the procedure time was limited to 15 minutes and/or two sudden disengagements (“pop-offs”). Broekhuizen and colleagues (1987) noted that the vacuum extractor was often chosen over the forceps for difficult deliveries. In a retrospective study, this group noted that 60 percent of vacuum cases were initiated in the midpelvis compared to only 9 percent of forceps deliveries. Malposition of the fetal head (occiput posterior or transverse) was seen in 81 percent of vacuum cases as compared to only 9 percent of forceps cases (Broekhuizen and coworkers, 1987). In a retrospective study, Baerthlein and coworkers (1986) compared 512 mid-pelvic vacuum extractions with 592 midforceps procedures and documented a significant increase in maternal morbidity in the forceps group. There was no significant difference in neonatal morbidity other than “inconsequential cephalhematoma” in the vacuum group.
The utilization of the vacuum extractor for operative vaginal delivery has increased tremendously in the United States during the past decade. This is likely the result of training in vacuum-assisted delivery in a majority of residency training programs in the United States and Canada. A 1995 survey of residency training programs (Bofill and associates, 1996) revealed that nearly all of the responding programs (95 percent) purport to train their residents in vacuum delivery. This survey reported data from 210 residency training programs (72 percent response rate) and noted that about one-third of these institutions perform more vacuum than forceps procedures. Hankins and associates (1999) noted that residency program directors expected their residents to be proficient with forceps and vacuum for outlet and for low-pelvic deliveries (both with less than 45 degrees rotation and with greater than 45 degrees rotation). However, the expectation of proficiency with instruments for midpelvic delivery was divergent. Only 38 percent of directors of residency training programs expected their graduates to be proficient with midforceps procedures, while 69 percent expected proficiency with midpelvic vacuum extractions.
Until recently, obstetric forceps was considered the preferred instrument for operative vaginal delivery in the United States. In an international survey of operative vaginal delivery, Hillier and Johanson (1994) noted that the obstetric forceps were the most commonly used instrument in the United States and other “English-speaking countries.” Other data, however, suggest that the vacuum extractor has achieved parity or has exceeded the obstetric forceps even in the United States. In a random survey of 558 Fellows of the American College of Obstetricians and Gynecologists (Bofill and co-workers, 1996b), it was noted that only 51 percent of respondents used the obstetric forceps more often than the vacuum. When the time elapsed since residency was considered, these researchers reported that the more recently trained obstetricians were more likely to have been taught the use of the vacuum extractor and were more likely to use vacuum for operative vaginal deliveries initiated in the midpelvis, or for “deep transverse arrest.”
Meniru (1996) explored trends in operative vaginal delivery in Great Britain during a five-year period. From 1989 through 1993 the overall rates of operative vaginal delivery remained steady at about 10 percent but the percentage of vacuum procedures gradually changed from 14 percent in 1989 to 34 percent in 1993. There are similar trends in the United States. In the eight-year period from 1989 through 1996, the overall rate of operative vaginal delivery in the United States remained steady at approximately 9 percent (Ventura and colleagues, 1998). However, during this period of time there was a 42 percent decrease in forceps procedures while there was a concurrent 77 percent increase in vacuum deliveries.
Learman (1998) studied the regional and temporal trends in operative vaginal delivery using data from the National Center for Health Statistics and the National Hospital Discharge Survey from the years 1987 through 1994. He reported that use of the vacuum extractor surpassed that of the forceps in the western United States in 1988, in the Northeast in 1990, and in the Midwest in 1991. Forceps procedures continued to outpace vacuum procedure in the southern United States during the years of this study, but there was near parity regarding the use of these instruments in 1994 (Learman, 1998).
With the increase in vacuum use in the last decade, there has been an increase in the number of reported neonatal complications. On May 21, 1998, the United States Food and Drug Administration distributed a public health advisory (FDA, 1998), “Need for Caution When Using Vacuum-Assisted Delivery Devices.” The FDA reported 12 deaths and 9 serious injuries in the preceding 4 years (about 5 events per year) among newborns on whom vacuum-assisted delivery devices were used. It was the concern of the FDA that some health care professionals who were using these vacuum devices were unaware of the possibility of life-threatening neonatal complications such as subgaleal hematoma or intracranial hemorrhage. A subsequent Committee Opinion from the American College of Obstetricians and Gynecologists (1998) noted that there were an average of 228,354 vacuum deliveries per year in the period of time covered by the FDA advisory, which amounted to 1 adverse event for every 45,455 vacuum deliveries. It was concluded that clinicians using these devices should be familiar with the indications for the use of these devices and be properly educated in their use. This Committee strongly recommended the continued use of vacuum-assisted vaginal delivery devices in appropriate clinical settings.
PRINCIPLES OF VACUUM EXTRACTION
The praxis of vacuum-assisted vaginal delivery is straightforward and can be summarized for a soft-cup delivery as follows:
• An indication should exist for the procedure.
• There should be informed consent.
• The cervix should be fully dilated and the fetal head should be engaged.
• The position of the fetal head should be known.
• The vacuum set-up should be tested against the clinician’s gloved hand.
• The vacuum cup should be placed on the median flexing point of the fetal head.
• The vacuum pressure should be raised to 100 mm Hg, and the clinician should run a finger around the rim of the cup to make certain no maternal tissue is included under the cup.
• The procedure should be timed from the time of placement of the cup until the delivery is completed.
• The vacuum pressure should be brought to 600 mm Hg and traction should be initiated when a contraction ensues that is simultaneous with maternal expulsive efforts.
• Traction should be in the direction of the pelvic axis and perpendicular to the cup.
• Torsion should never be applied to the traction bar to effect rotation of the fetal head.
• The procedure should be abandoned if there are three pop-offs.
• The procedure should be abandoned if there is any evidence of fetal scalp trauma after a pop-off.
• The procedure should be abandoned if a time threshold is reached.
• The procedure should be abandoned if there is no descent with an appropriate application and traction (without waiting for three pop-offs or 20 minutes to elapse).
• After delivery the scalp should be inspected for trauma and position of the chignon.
• Nursery personnel should be alerted that the delivery was accomplished via vacuum.
• The procedure should be thoroughly documented.
The indications for vacuum-assisted delivery are nearly identical to those indications for use of the forceps. Well-known indications include a prolonged second stage of labor and nonreassuring fetal status. Other indications include maternal exhaustion and maternal illnesses in which pushing efforts should be limited (cardiac, pulmonary, or neurologic disease). Rarely does the medical record demonstrate that the instrument was used electively although this is often the case. Contraindications to the use of the vacuum include face, brow, or breech presentation. Although the vacuum extractor has been used to assist in the birth of preterm infants (Morales, 1995; Thomas, 1997; and their coworkers), forceps delivery is generally recommended if the estimated gestational age is less than 34 weeks.
Clinicians should discard the erroneous notion that the vacuum device should be used, instead of the forceps, when the position of the fetal head within the maternal pelvis is unknown. Important clinical information is derived from a careful assessment of the fetal head with regard to the size and position of the caput succedaneum and the amount of molding. Severe molding of the fetal head may be indicative of disproportion of the fetal head with respect to the maternal pelvis. Stewart (1980) devised a method to describe the amount of molding by examination of the parietal bones. If the parietal bones are clearly separated, then no molding is present; if the parietal bones touch, but do not overlap, then molding is slight; if the parietal bones overlap but can be reduced by the clinician’s digital pressure, then the molding is moderate; lastly, if the overlap of the parietal bones cannot be reduced, then the molding is considered to be severe (Fig. 7-4).
FIGURE 7-4. The estimation of the degree of molding as described by Stewart (1980). No molding is present (0) when the parietal bones do not touch; molding is considered mild (+) when the parietal bones touch in the midline; molding is considered moderate (++) when the parietal bones overlap in the midline but can be reduced with the clinician’s digital pressure; molding is considered severe (+ + +) when the parietal bones overlap and cannot be reduced. (Adapted from Vacca, 1990, with permission.)
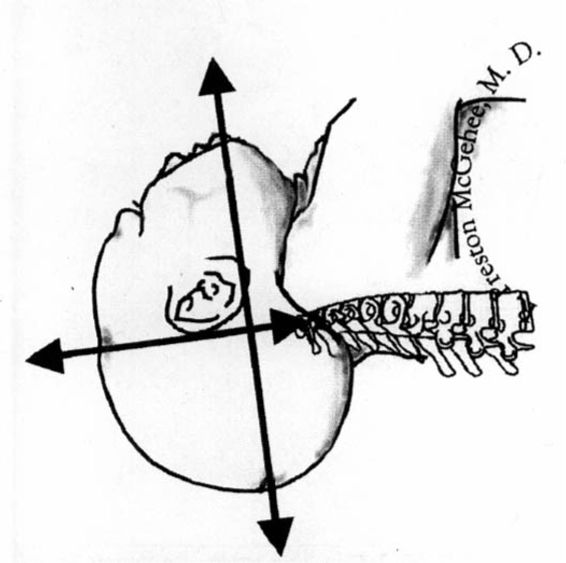
Safe and successful vacuum-assisted vaginal delivery is contingent upon an appropriate application of the cup onto the fetal head. The position of the fetal head should be known. It is of utmost importance that the cup be placed on the so-called “flexing point” (Vacca, 1990). The flexing point is located where the mentovertical diameter of the fetal head emerges which is about 3 cm anterior to the posterior fontanelle and in the midline (Fig. 7-5). The fetal head is considered to be completely flexed when the mentovertical diameter points in the direction of the pelvic axis. The center of the vacuum cup should be placed over the flexing point and symmetrically astride the sagittal suture. Placement of the vacuum cup over this landmark is important because subsequent traction in the direction of the pelvic axis will maintain flexion and correct or maintain synclitism. The pelvis will then be presented with the most favorable diameter of the fetal head. The ideal vacuum cup application is called the “median flexing” application. When the cup is placed over the median flexing point a small amount of vacuum pressure should be established and the clinician should make certain that no maternal tissues have been entrapped underneath the edge of the cup. Severe lacerations to the maternal genital tract, with possible bladder or bowel damage, may result from entrapped maternal tissue.
FIGURE 7-5. The mentovertical diameter emerges about 3 cm anterior to the posterior fontanelle; this is described as the median flexing point. The fetal head is considered well flexed when the mentovertical diameter points in the direction of the pelvic axis.
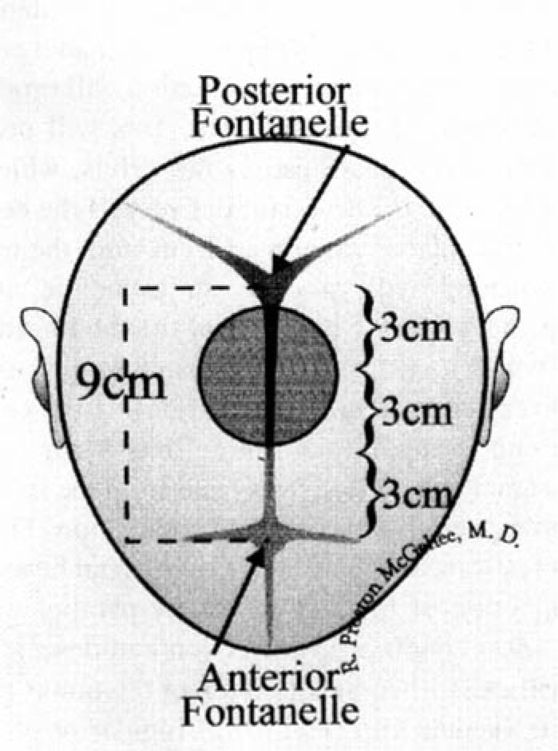
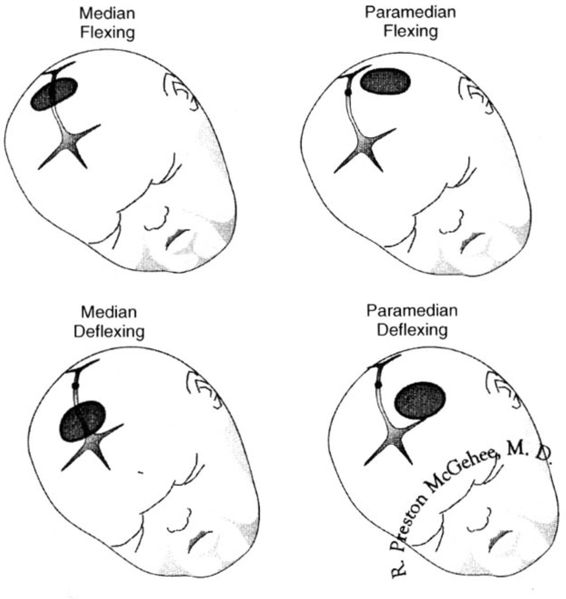
In a term fetus, the sagittal suture will measure about 9 cm (Fig. 7-6). If the center of a 60 mm cup is placed 3 cm from the posterior fontanelle, one edge of the cup will encroach on the posterior fontanelle while the opposite edge will be situated about 3 cm from the anterior fontanelle. If the center of the vacuum cup is placed more than 3 cm from the posterior fontanelle, subsequent traction will produce an attitude of deflexion of the fetal head. This will present a larger diameter of the fetal head to the pelvis, which may lead to pop-offs or an unsuccessful delivery. If the center of the vacuum cup is placed more than 1 cm from the midline, subsequent traction will produce an asynclitic attitude, which will present a larger diameter of the fetal head to the pelvis and which may lead to an unsuccessful vacuum-assisted delivery (paramedian application). If the center of the vacuum cup is applied both more than 3 cm from the posterior fontanelle and more than 1 cm from the midline, it is considered a paramedian deflexing application (Fig. 7-7).
FIGURE 7-6. This demonstrates the appropriate placement of a 60 mm vacuum cup. The distance from the anterior to the posterior fontanelles should be about 9 cm in the term infant. The vacuum cup should be positioned symmetrically astride the sagittal suture. One edge of the cup should encroach upon the posterior fontanelle, and the opposite edge should be situated about 3 cm from the anterior fontanelle (see text).
FIGURE 7-7. In these images, the median flexing point is identified by the black dot on the sagittal suture. The positions of the vacuum cup for the median flexing, median deflexing, paramedian flexing, and paramedian deflexing applications are demonstrated (see text).
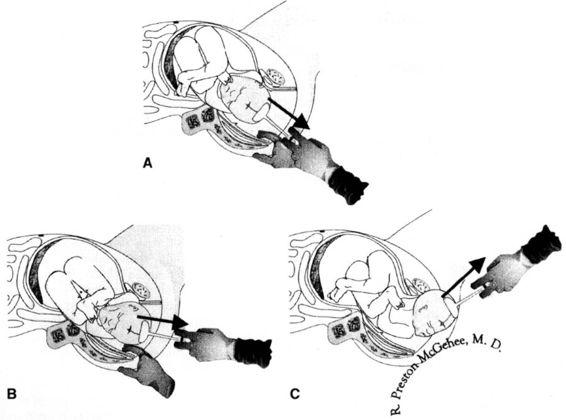
The least resistance to the passage of the fetal head occurs when the direction of traction is exactly parallel with the pelvic axis. Ideal conditions for traction and descent of the fetal head will exist when the direction of traction is perpendicular to the vacuum cup (Fig. 7-8). Angular or off-center traction tends to lift the far edge of the cup, which may lead to sudden disengagements. Most procedures initiated at the outlet or in the low pelvis can be easily accomplished without any angular traction because the fetal head will be well flexed and synclitic. Challenging vacuum procedures in which angular traction could be a problem will involve those cases initiated in the midpelvis or when there is significant deflexion or asynclitism of the fetal head. The clinician can sometimes compensate for this angular traction by using the thumb or index finger of the nontraction hand to apply counterpressure on the far side of the cup, which may detach.
FIGURE 7-8. It can be seen in these images that the traction stem is at a perpendicular angle to the plane of the vacuum cup. There is no angular traction. The black arrow demonstrates traction is directed parallel with the pelvic axis (see text).
Clinicians may be tempted to apply torsion to the vacuum cup when it is used to deliver an infant from an occiput posterior (OP) or occiput transverse (OT) presentation. Torsion applied to the vacuum cup may result in fetal injury. Straight vacuum traction often produces rotation to the anterior when the fetal head encounters resistance from the maternal levator musculature. This is termed “autorotation.” Vacca (1992) reviewed five studies that documented that 72 percent of infants delivered from OP or OT positions underwent autorotation and delivered as occiput anterior (OA).
It is important that vacuum extraction should be limited to a second-stage procedure and that it should not be attempted prior to full cervical dilatation except in the direst of circumstances. A prerequisite for vacuum applications should be fetopelvic engagement. The vacuum cup should not be applied at “high” stations. Hankins and coworkers (1999) documented that there is wide agreement that the 1988 ACOG forceps classification should be used when a vacuum procedure is performed. This classification divides the pelvis into outlet, low, and midpelvic stations and also categorizes the procedure by the amount of rotation required (less than or greater than 45 degrees of rotation). Other important principles of safe vacuum-assisted vaginal delivery include the requirement for adequate uterine contractions and maternal expulsive efforts. Typically, traction is applied only during those times when the patient is actually pushing.
As with a forceps delivery there should always be at least one experienced clinician in attendance. An important aspect of vacuum extraction is the willingness of the clinician to abandon the attempt if the delivery does not appear to be proceeding smoothly. The vacuum pressure should not exceed 600 mm Hg. Clearly, if fetal scalp trauma is identified the vacuum cup should be removed and the delivery completed in another manner. The length of time the vacuum cup is on the fetal head has been identified as a predictor of cosmetic scalp lesions (Teng and Sayre, 1997) and of cephalohematoma (Bofill and coworkers, 1997b). Authorities vary in their recommendations for the upper limit of time that the vacuum cup should be on the fetal scalp, and this time is quoted to be anywhere from 15 to 45 minutes (Greis and colleagues, 1981; Ross, 1994). In our own practice, we have limited the length of time that the cup may be on the fetal scalp to no more than 20 minutes. Most authorities also place a limit on the number of pop-offs that can be sustained prior to abandonment of the vacuum procedure. We allow only two reapplications of the cup. If the cup pops off three times, the attempt at vacuum delivery is abandoned. Cup detachment should not be considered as a safety mechanism of the vacuum extractor. Cup detachments may be indicative of a nonmedian flexing application, angular traction, or cephalopelvic disproportion. Importantly, if a proper application and adequate traction do not produce descent of the fetal head, the procedure should be considered to be an unsuccessful trial of vacuum without waiting for three pop-offs or for 20 minutes to elapse.
The fetal scalp should be inspected after delivery to assess the position of cup placement and to document any obvious trauma. If the nursery personnel are not present at delivery, they should be informed that the infant was delivered by vacuum so that attention may be focused on the fetal scalp in the hours after delivery. Lastly, a thorough note should be placed in the medical record that documents the procedure. The important points to document include the indication for the procedure, the instrument used, the station and position of the fetal head at the time the cup was applied, the number of pop-offs, and the amount of time the cup was on the fetal head. The amount of caput, molding, and asynclitism at the time of placement of the cup should be documented. Auto-rotation occurring during delivery should be recorded. The type of analgesia provided, episiotomy requirements, and whether any maternal or fetal trauma was sustained should also be documented.
THE UNSUCCESSFUL VACUUM DELIVERY
There are times when the criteria for abandonment of a vacuum-assisted vaginal delivery will be reached. There are three delivery options to consider at this point. Spontaneous delivery is possible if there are still good maternal expulsive efforts and the fetal head is on the pelvic floor. Cesarean delivery is an option, and may be preferable, especially if the fetal head is in the midpelvis. Lastly, the obstetric forceps may effect delivery after the attempt at vacuum delivery has been abandoned, especially if the fetal head is at or on the pelvic floor. The propriety of these sequential operative vaginal deliveries is controversial.
Revah and colleagues (1997) studied three cohorts of women; a group who had an unsuccessful trial of forceps, another group with an unsuccessful trial of vacuum, and a group of patients who had unsuccessful attempts at both vacuum and forceps. These researchers were able to demonstrate that an unsuccessful trial of instrumental delivery, either forceps or vacuum, was not associated with increased maternal or neonatal morbidity in a setting in which a cesarean delivery could be expeditiously performed.
Berkus and collaborators (1986) described 36 cases of Silastic cup procedures that were completed with the forceps, and 9 cases in which the unsuccessful vacuum procedures were completed by cesarean delivery. In this series, the authors noted that the vacuum extractor was able to convert what would have been a difficult midforceps procedure to an outlet forceps delivery. Neonatal morbidity was not significantly different between cases of successful and unsuccessful vacuum deliveries, except for an increased frequency of neonatal retinal hemorrhages in the unsuccessful vacuum group. Ezenagu and collaborators (1999) reviewed nine studies of operative vaginal delivery and reported that the sequential use of instruments to effect delivery varied from 4 to 27 percent (mean, 8 percent) of cases. In their own cohort study of 34 patients delivered by the sequential use of instruments, Ezenagu and coworkers were unable to document any increased maternal or neonatal risks. However, this group cautioned that the decision to use a second instrument after the first instrument failed to effect delivery requires individualization of care and should not be undertaken by inexperienced clinicians.
VACUUM OR FORCEPS?
Some authorities adamantly support the vacuum extractor as the preferred instrument for operative vaginal delivery (Chalmers and Chalmers, 1989), while others have been more circumspect in their recommendations (Ryden, 1986; Drife, 1996). It has been difficult to perform meta-analyses of studies of vacuum extraction and forceps for at least three reasons. First, the published investigations have demonstrated important methodologic differences that have made the pooling of data difficult. Second, these studies cover a 30-year period of time (Lasbrey, 1964; Bofill and colleagues, 1996a; and their colleagues). Third, these studies have used many different types of vacuum extractor cups, each of which probably has an inherently different rate of efficacy and complication.
The above limitations notwithstanding, Johanson and Menon (1999, 2000) performed a meta-analysis of trials of vacuum and forceps as part of the Cochrane database of systematic reviews. These researchers pooled the results from 10 prospective and randomized trials from the obstetric literature and presented some intriguing findings. First, the vacuum extractor is significantly less likely to achieve a successful vaginal delivery as compared to forceps. However, the women who randomized to the vacuum arms of these studies actually had a lower cesarean delivery rate because a vacuum failure was often followed by a forceps delivery, whereas failed forceps deliveries most often were completed as cesarean sections. Maternal genital tract injury was significantly higher in the forceps group. Women who randomized to the vacuum had significantly less pain at delivery and significantly less pain 24 hours postpartum, even with a lower rate of usage of regional and general anesthesia. The vacuum extractor was associated with a higher rate of neonatal cephalohematoma and retinal hemorrhages, but there was no significant difference in the numbers of babies who required phototherapy.
In a population-based historical cohort study involving 31,015 women delivered by vacuum and 18,727 delivered by forceps, Wen and colleagues (2001) concluded that vacuum was associated with less maternal trauma but “may increase the risk of cephalohematoma and certain types of intracranial hemorrhage (eg, subarachnoid hemorrhage).”
It should be acknowledged that, in modern practice, the clinician’s choice of vacuum or forceps usually depends on local tradition and the influence of the instruction he or she received during residency training. The choice of whether to use vacuum or forceps rarely hinges on the results of the published studies.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree