Inflammatory
Radicular cyst (Apical, lateral, and residual cyst)
Paradental cyst (Inflammatory collateral, mandibular infected buccal, or buccal bifurcation)
Developmental
Dentigerous (follicular) cyst
Eruption cyst
Gingival cysts of infants (newborn)
Calcifying odontogenic cyst
Odontogenic keratocyst (primordial cyst)→ Keratocystic odontogenic tumor (2008)
Lateral periodontal cyst
Glandular odontogenic cyst: sialo-odontogenic cyst
Nonodontogenic cysts
Nasopalatine duct (Incisive canal) cyst
Nasolabial (Nasoalveolar) cyst
Odontogenic Cysts
Inflammatory Cysts
Radicular Cysts
Introduction
The radicular cyst is an odontogenic cyst of inflammatory origin with a chronic periapical granuloma precursor that matures from the stimulation of cell rests of Malassez present in the periodontal membrane [3, 4]. Radicular cysts have different classifications by location:
Biology and Epidemiology
An inflammatory process stimulates proliferation of the rest of Malassez, and the center of the lesion degenerates and liquefies to form a cyst [1, 2, 5, 6]. The lesion forms a fairly well-defined periapical radiolucency which continues to enlarge via cell break down and hyperosmotic gradient resulting in transudation of the fluid into the lumen of the lesion [2, 5, 6].
Presentation
Differential Diagnosis
Odontogenic cyst: inflammatory (radicular cyst) vs. developmental (dentigerous cyst).
Odontogenic tumor: keratocyst odontogenic tumor, ameloblastoma.
Nonodontogenic bone lesions such as giant cell tumor.
Diagnosis and Evaluation
Physical examination:
Tooth is often nonvital.
Tenderness to palpation or percussion of affected teeth.
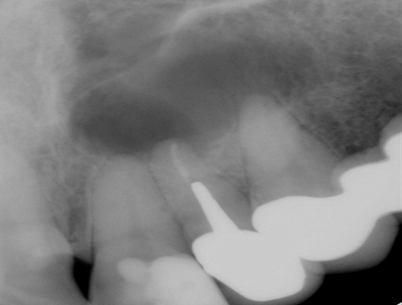
Imaging evaluation:
Pathology
Treatment
The offending tooth is often nonvital and requires root canal therapy to remove the pulpal tissue and eliminate bacterial load.
If the lesion is large, enucleation is required to eradicate the inflammatory cystic lesion and subsequent apicoectomy of the tooth with retrograde filling can be done.
If the offending tooth is nonrestorable, removal of the tooth is another method to eliminate the source of infection.
The residual cyst will require enucleation if it persists after extraction of the offending tooth.
Complications
Rare.
Buccal Bifurcation Cyst (BBC)
Introduction
The BBC, also previously known as the mandibular infected buccal cyst described by Stoneman and Worth in 1983, is a type of paradental cyst based on the WHO classification [9]. It is a rare inflammatory cyst of odontogenic origin. It is easily misdiagnosed as radicular cyst because radicular cysts are more common lesions and have a similar presentation [2, 9–11].
Lesions with similar characteristics have been called other names, such as “circumferential dentigerous cysts” by Thoma in 1964. Thoma described a cyst that involved the mandibular second molar with cystic development of the enamel organ around the neck of the tooth interfering with its eruption. The “inflammatory collateral dental cyst” was described by Main in 1970. It is histologically identical to the inflammatory radicular cyst and is associated with vital mandibular third molars that have chronic periocoronitis. In 1976, Craig called the cyst “juvenile paradental cyst.” He described the cyst around a vital third molar tooth and attachment to the buccal bifurcation [11].
Biology and Epidemiology
The BBC is inflammatory rather than developmental in origin. It also has distinct clinical and radiographic features which distinguish it from other inflammatory paradental cysts [2, 10].
The BBC develops on the buccal aspect of vital mandibular first molars and occasionally involves the second molars [9–11].
Etiology: unknown but many speculate that the inflammatory response in the dental follicle during eruption may be the inciting factor. As the mesiobuccal cusp of the first molar penetrates through the oral epithelium, it induces an inflammatory reaction in the connective tissue, causing epithelial proliferation and cyst formation [2, 7–11]. Alternatively, it is also believed that the inflammatory response from pericoronitis may stimulate cyst formation [9–11].
The BBC may be a variant of lateral periodontal cyst, and the cystic epithelium is derived from the cell rests of Serres, the cell rests of Malassez, the cells of the dental lamina, or the reduced enamel epithelium [9].
Age distribution: seen in children with a range of 4–14 years.
Presentation
Differential Diagnosis
Odontogenic cysts (BBC, radicular cyst, or dentigerous cyst).
Benign odontogenic tumors (ameloblastoma or keratocyst odontogenic tumor).
Nonodontogenic tumors (giant cell tumor, myxoma, or vascular malformation).
Diagnosis and Evaluation
Primarily based on the clinical and radiographic features.
Physical Examination
Imaging Evaluation
Panoramic or periapical radiograph supplemented by occlusal view radiograph are sufficient for diagnosis. The lesion appears as a U-shaped radiolucent lesion on the buccal aspect of the tooth covering the roots (Fig. 32.2). The periodontal ligament space (lamina dura) is intact and the cyst is unlikely to extend to the inferior border of the mandible. The buccal tilting of the tooth pushes the apices of the roots toward the lingual plate, and a buccal periosteal reaction is often evident. The lesion can be 1 cm in size [2, 9–13].
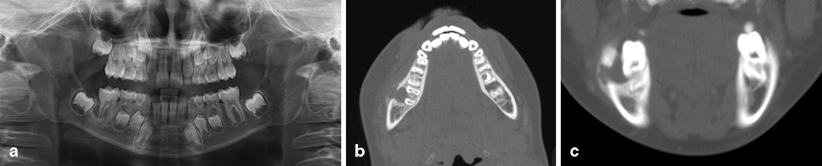
Fig. 32.2
a Panoramic radiograph demonstrating U-shaped radiolucency around the root of the lower, right first molar. Axial (b) and coronal (c) CT cuts show cortical perforation with a well-circumscribed lesion located on the buccal surface of the involved tooth
Computerized tomography (CT) scan: In today’s modern health care system, a CT scan is often used to better delineate the lesion (Fig. 32.2).
Pathology
Histopathologic examination (Fig. 32.3) shows the cyst wall lined by nonkeratinizing, stratified, squamous epithelium and a fibrous stroma with chronic inflammation [9–11]. These findings are nonspecific, and are similar to those found in a radicular cyst. As a result, diagnosis cannot be made from the histopathologic features alone [9].
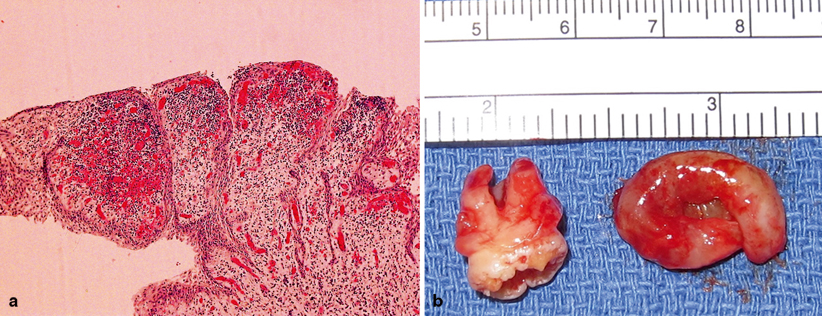
Fig. 32.3
a Histologic examination showing nonkeratinizing, stratified, squamous epithelium with spongiosis overlying chronically inflamed fibrous connective tissue. The specimen (b) shows the U-shaped lesion
Treatment
Surgical treatment is successful with low recurrence.
Treatment options: curretage, marsupialization, enucleation, removal of the tooth.
Nonsurgical approaches: periodontal probing or daily irrigation of the buccal periodontal pocket with saline have been reported [9].
Developmental Cysts
Dentigerous (Follicular) Cyst