Fig. 1
Young child reaching for a toy to encourage active reach during an assessment
Younger children are often more cooperative if the assessment is presented as a game or challenge, such as “Simon says” or reaching for a target. Allowing the child to touch the goniometer and “measure” a parent or doll can decrease anxiety and improve participation. For children with motor planning difficulty, demonstrate the desired motion. Using mirror movements of both arms can also help the child elicit the desired motion. Hand AROM in this age group is often assessed with observation. PROM in larger joints can be obtained. Using distraction techniques, such as music, toys, or videos, may allow the patient to relax for a more accurate measurement without co-contraction or resistance to being moved (Ashworth and Kozin 2011).
Older children and adolescents are better able to participate in formal goniometric measurements. For younger school-aged children, a playful approach may provide better rapport and performance. The older children can better follow directions. This age group can tolerate blocked and composite motions to differentiate tight structures for thorough examination.
These techniques to obtain ROM assessment are also utilized for treatment. Games, toys, and crafts can elicit desired ROM with creative positioning of the activity or child. To facilitate shoulder external rotation and overhead reach, a poster board can be taped to a vertical surface for a painting project (Fig. 2). A child working on opposition can be directed to pick up dice between thumb and each finger, progressing to the ulnar side with each turn. Many children have difficulty with stretching. Using distractions such as songs, bubbles, or a favorite TV show can help the child tolerate the intervention. Incorporating exercises into daily life can be difficult for busy families. Try to focus on the most important exercises and educate the family on positioning and activities that will incorporate the desired range of motion into activities they are already completing.


Fig. 2
Young boy eliciting external rotation by painting on a vertical surface
Strength
Strength is a dynamic element in pediatrics due to variations in childhood development. It differs greatly between sexes and age groups and does not follow a linear pattern, as there are large increases in strength at various ages in addition to relative differences between genders (Stam and Hovius 2010). Strength can be a determining factor in a child’s ability to acquire new skills; therefore, it is imperative to focus on strength during the assessment and intervention of a pediatric patient.
Strength, being the body’s ability to generate force for a short duration, is highly dependent upon effort. Getting maximal effort out of a child relies on the assessors’ ability to ensure the child feels comfortable, comprehends the directions, and is compliant with testing protocol. These factors are necessary to capture valid and reliable data. Simple strategies such as allowing the patient to hold, touch, or examine the testing equipment; demonstrating the test on their parents, siblings, etc.; or allowing them to administer it to a family member are all good way to increase their comfort level with the equipment and testing methods. Decorating testing equipment with funny faces, stickers, pictures, etc., can make the device less threatening. Next, the communication of expectations needs to be multimodal and appropriately worded. Verbal instructions should be combined with visual modeling and hands on demonstration, as children differ in their ability to comprehend auditory, visual, and tactile input. Language should be child appropriate and avoid medical jargon. Instead of using the joint or muscle to describe what you want the patient to do, ask them to touch their nose and keep their finger there for biceps testing, or ask them to try and poke you to assess triceps strength. Prior to testing, the patient should be positioned with proper support for stability in order to isolate the targeted muscle group. Supine is good for testing the elbow joint, and seated with foot support for shoulder, wrist, and hand. Finally, have them explain what they are going to do and complete a practice trial. With proper instructions, demonstration, and review, valid and reliable strength testing can be performed on children as young as 3 years old.
Assessment of strength is an essential part of the upper extremity evaluation and progress monitoring and a key factor in guiding clinical decisions. Strength testing can help identify the need to develop antagonist muscle strength to counteract spasticity for improved range of motion in children with spasticity, help determine what may be causing functional limitations in patients with neuromuscular disease, be performed preoperatively as a means to assist in selection of muscles for tendon transfer, and provide essential baseline data needed to appropriately develop an intervention plan and set measurable goals.
As a progress monitoring tool, evaluation of strength allows the clinician to upgrade, downgrade, or modify provision of therapy based on patient performance. It can measure the deficit remaining and indicate need for continued intervention, provide a means to measure compliance with home programs, and document the patient’s return to premorbid status.
Finally, strength assessments can be used to evaluate the effectiveness of clinical, surgical, and pharmacological interventions as part of clinical practice, clinical research, and natural history studies to learn more about the disease process.
For an assessment protocol to be useful in the clinical setting, it is important that it is specific to the clinical characteristics of the disease and is sufficiently sensitive to detect change in muscle performance using serial measurements. In addition, it is essential to target muscles that are relevant to upper extremity functional performance. If unfamiliar with a diagnosis, a literature review should be completed by the clinician to determine which muscle groups and joints are affected. There are various methods to assess strength, each having their own advantages as well as limiting factors. In order to select the appropriate method, a clinician has to consider the patient population, purpose for testing as previously discussed, and any limiting patient or environmental factors. Strength can be accessed via observation, hands on testing, and with the use of standardized equipment or assessments.
Observation
In the case of the fragile infant or a noncompliant patient due to age/cognitive/behavioral limitations, one needs to be creative in their assessment. Observation-based strength measurements can include prone skills (Fig. 3), supine reach, transitional movements, play abilities (Fig. 4), etc. For example, wheelbarrow walking is a great way to evaluate proximal shoulder girdle, pectoral, and triceps strength as well as distal hand strength in toddlers. While the child is having fun doing the wheelbarrow, the clinician can observe for any indication of weakness (collapsing at the elbow, fisting of the hands, turning of the hands in or out, sliding or shuffling of the hands to avoid single arm weight bearing, etc.). An infant’s ability to reach and sustain movement against gravity, push up into prone or quadruped, and pull to sit also offer valuable observations of strength. Observation-based measures are advantageous because they can be quick and easy, do not require any specialty training or expensive equipment, and can be suited to meet the needs of various patient populations as described above. However, observations are limited due to their subjective nature and limited measurability.



Fig. 3
Prone strength assessment during play

Fig. 4
Strengthening the flexors on a vertical swing
Manual Muscle Testing (MMT)
The most common method of evaluating the strength of separate muscle groups is the Medical Research Council (MRC) scale (Medical Research Council 1976), which is used for Manual Muscle Testing (MMT). The scale covers a range of strength from 0 (no contraction of the muscle) to 5 (normal strength) in which the ability to move against gravity and through the full range of motion are important elements. The scale is a simple, quick, cost effective, and standardized towards measuring strength in children who are able to follow basic instructions – such as “try to touch your shoulder as hard as you can” for elbow flexion and “try to reach the sky as hard as you can” for elbow extension. However, the scale is not sufficiently sensitive to assess strength in very weak muscles, when movement is possible only in the gravity eliminated plane and in patients with contracture, as full range is not possible. MMT is best used as a quick screen to identify muscle groups that require further testing with more objective means of measurement.
Myometry
Similar to MMT, myometry is quick and easy to administer and provides an objective, highly measurable method of evaluating specific force produced at a joint.
Myometry has proven to be a highly reliable and valid method of assessing strength in children with neuromuscular conditions (Escolar et al. 2001) and for specific muscle groups has shown reliability as young as 2 years old (Rose et al. 2008) . Myometry also helps to differentiate strength within a MMT grade. For example, Van der Ploeg et al. compared the nonparametric MRC scale with parametric handheld dynamometry and concluded that an MRC grade 4 covers a wide range of forces ranging from 10 to 250 N (Van der Ploeg et al. 1984). Myometry is also a good tool for evaluating patients with decreased range of motion or contractures that do not allow for typical MMT. In this case, a set position should be chosen and documented to ensure serial testing is accurate. This is especially helpful in evaluating children during the recovery process in diagnosis such as obstetric brachial plexus injury, peripheral nerve injury, stroke, etc. There are many handheld myometers on the market with a variety of options and accessories. They can be mounted or handheld (Fig. 5), provide comparison of left/right limbs with % difference, offer change variance scores within each extremity, and offer storage options for an entire assessment to eliminate the need to manually record data after each individual test. Measurement can be done using the “make” or “break” method. For a “make” test, the examiner holds the myometer stable, and the subject exerts a maximal force against the myometer for a period of 3–5 s. For a “break” test, the subject exerts a maximal force against the myometer, and the examiner applies sufficient force to break the hold. In children, it is especially important to ensure that a maximal effort was given and the data collected is valid and repeatable. If at least two of the three repetitions recorded are not within approximately 10 % of each other, the trial should be repeated (Phillips et al. 2000). The myometer is a very effective tool in measuring strength and has few limitations; however, the financial cost of the device may be a limiting factor for small private practices or individual practitioners.


Fig. 5
Hand held myometry for evaluating elbow flexion strength
Functional Strength Measurements
Functional scales should also be considered when evaluating strength. They combine the functional movement/task performance aspect of the observation-based assessments with the measurable properties of MMT and myometry. Both MMT and myometry focus on specific isolated muscle strength, but do not allow for compensatory movement strategies that children utilize to perform ADLs. Assessments such as the Spinal Muscle Atrophy (SMA) Upper Limb Module (Mazzone et al. 2011) and Jebsen-Test of Hand Function do capture range of motion and endurance to some extent but also assess functional strength of the upper extremity that is important. Test items are generally specific to ADLs or closely related and allow clinicians to interpret how performance-based components such as range of motion, dexterity, strength, and sensory function impact task performance. Finally, evaluation of specific tasks such as opening a sealed water bottle and medicine bottle with child proof caps, tearing open a bag of chips or a yogurt lid, removing caps from markers, and pulling apart toys offers good functional strength outcomes for goal writing.
Intervention for Strength
Resistance training in children and adolescents has proven to be effective and safe and provides an effective way for enhancing motor performance (Behringer et al. 2011). Unlike adults, children often require creative approaches to strengthening programs as traditional rote exercises tend to be boring and often require focus that may not be possible for younger children or those with cognitive impairments/developmental delays. Although the therapeutic approach may have to be different, the same principle apply in terms of using progressive resistance exercises, except in the case of muscular dystrophies or other diagnoses where strengthening is contraindicated. The key is to identify the muscles/muscle groups that need to be addressed and then create play-based activities that utilize those muscles in a controlled, gradable, and measurable fashion. Prone-based play on physioballs (Fig. 6), swings, wedges, and other prone positions is a great way to target the chest, anterior deltoid, triceps, and distal hands. The activity can easily be graded by varying the level of support and angle of the body and by adding additional resistance via resistive bands/weights/etc., to the patient. Resistive pulling activities (tug of war, climbing, rowing, swings, and scooter play) are fun ways to target the latissimus, rhomboids, biceps, and distal hands as well. Younger children can participate by imitating animal walks, yoga poses, and playing gaming systems such as Wii and Xbox Kinect with simultaneous resistance applied to the desired movement. The Wii Remote controller can be secured with Fabrifoam® to the forearm to enhance shoulder and elbow movement (Fig. 7).



Fig. 6
Prone weight bearing over ball for upper extremity strengthening

Fig. 7
Child with hemiplegia has a Wii Remote controller secured with Fabrifoam® on the forearm to encourage shoulder and elbow range of motion while playing a game (Courtesy of the Children’s Hospital of Philadelphia)
Consideration of baseline strength and motor control is necessary to develop the most effective treatment plan. The ability to actively move a limb is dependent on many factors that should be carefully assessed to determine the appropriate interventions. Motor control can be impacted due to traumatic brain injury (TBI), spasticity, pediatric stroke, etc., which may limit the ability to activate and recruit appropriate muscles for movement or relax the antagonist group. In this situation, coupling strengthening activities with biofeedback is a good way to improve motor control for more successful strengthening. In the case of peripheral nerve injury, brachial plexus injury, SMA, and other neuromuscular disorders, baseline strength can be substantially impaired to the point where gravity alone is a barrier to movement. In these cases, gravity eliminated or reduced movement planes are ideal for initiating strengthening. Aquatic sessions can be extremely beneficial, as the buoyancy of the water reduces the impact of gravity making it easier to move the limb, and the water can also be used to create assistance or resistance to movement as needed. Devices that decrease workload and/or accentuate movement (Wilmington Robotic Exoskeleton, counterbalance arm slings, Saebo mobile arm support) allow for initial strengthening to occur where it would otherwise be impossible. Computer-based software like the Biometrics E-Link Evaluation and Exercise System can be used to target strength in small muscles for cases like finger fractures where isolated strengthening may be limited with traditional equipment. Additionally, the Biometrics offers a surface EMG sensor that can provide feedback for isolated muscle activation (Fig. 8).


Fig. 8
Child positioned at Biometrics work station, moving a knob that is linked to a game on the monitor for desired wrist range of motion (Courtesy of the Children’s Hospital of Philadelphia)
For athletes and patients able to complete higher-level strengthening, progressive resistance exercises (PREs) can be performed with dumbbells, resistance bands, and other traditional strengthening tools. The use of body weight training with suspension systems like TRX (total body resistance exercise) (Fig. 9) can provide an excellent opportunity to work on joint stability, flexibility, and strength with very little space and equipment required. Resistance training programs for youth should follow a training model with a progressive and systematic variation in exercise selection, intensity, volume, frequency, and repetition velocity to enhance training adaptations, reduce boredom, and decrease the risk of overuse injuries (Plisk and Stone 2003). In addition, programs need to be tailored to the individual based on their past exercise experience, motor control, and physical limitations. Specific exercise volume (sets and repetitions) and resistance levels (based off % of 1 rep max) can be found in the Position statement on youth resistance training: the 2014 International Consensus. Finally, strength goals should be linked to specific functional impairments and discussed with patients in order to illustrate the benefit and importance of completion of exercises to restore independence or maximize athletic performance. Motivational tools such as charts, graphs, apps, etc., can help to motivate patients as well as provide a way to monitor progress and response to adaptations to the training program.


Fig. 9
TRX suspension push-up
Muscle Tone
Children who have the diagnoses of cerebral palsy, traumatic brain injury, high spinal cord injuries, pediatric stroke, or an unexplained hypoxic ischemic event may exhibit spasticity in one to four extremities. Tone is assessed by a quick range of motion stretch to a joint and can be measured using the Modified Ashworth Scale (MAS). It is a six-point scale with numbers ranging from 0 to 4 and may be useful in guiding outcomes posttreatment (Table 1). The use of the MAS becomes increasingly important for surgical options, and it is very useful to determine effects of pharmacological therapies such as Botulinum toxin or baclofen pump placement. Therapists play a crucial role in providing information on muscle tone to the physicians, as the child may be nervous in the physician appointment resulting in increased spasticity compared to baseline. Also, the surgeon may only briefly test AROM of the joint one or two times versus the therapist who challenges the child by making them exercise the extremity repeatedly causing fatigue and more spasticity over time. The child may also exhibit fair wrist extension with thumb extension with request from a physician but when that child is challenged to hold a 4 diameter jar for opening may exhibit dynamic tone while trying to complete the task. It is important for the therapist to document these differences and relay the findings to the physician for the most comprehensive plan for the child. Finally, video can be an extremely helpful tool to document quality of movement and progress in therapy and to provide the physician with a clinical picture of the patient prior to their appointment.
Table 1
Modified Ashworth Scale (MAS) for grading spasticity
Grade | Description |
|---|---|
0 | No increase in muscle tone |
1 | Slight increase in muscle tone, manifested by a catch and release or by minimal resistance at the end of the range of motion when the affected part(s) is moved in flexion or extension |
1+ | Slight increase in muscle tone, manifested by a catch, followed by minimal resistance throughout the remainder (less than half) of the ROM |
2 | More marked increase in muscle tone through most of the ROM but affected part(s) easily moved |
3 | Considerable increase in muscle tone, passive movement difficult |
4 | Affected part(s) rigid in flexion or extension |
Pain
A pain assessment is important, as it allows the clinician to monitor how the child feels at rest, with movement, during and after stretching, and during activities of daily living. Pain can hinder participation, as children are inherently fearful when they anticipate pain, and this anxiety can start before getting to the hospital. Cognition and developmental levels of the child are considered when assessing the child for pain. There are numerous pain scales that are uniform across a healthcare facility to ensure consistency of grading. It is important for the clinician to document the timing of the pain, such as before the activity begins, during the activity, and/or after the activity. If a heat modality is used prior to an activity, the therapist should document pain scores pre and post the modality application. Documenting pain is also useful in formulating functional goals for progressing the child in therapy.
Evaluation of Sensation
Evaluation of sensory function is important as our bodies require a collaborative effort between our sensory receptors to provide information on pressure, joint position, pain, and temperature to the brain. Subsequently, the motor neurons respond accordingly in carrying out the appropriate reaction. The two work synergistically to ensure smooth coordinated movements of the hand and upper extremity. A disturbance in sensory function will impact fine motor skills regardless of intact motor function. Individuals with impaired somatosensory feedback have difficulty grading fingertip forces used to grasp and lift objects, resulting in insufficient finger opening, object grasp at incorrect contact points, slips at object contact, temporal delays, and the use of excessive fingertip forces during fine motor tasks. This is crucial in pediatrics, as young children are continually developing their sensorimotor feedback system, and altered sensibility will impact skill acquisition. Sensation can be very difficult to describe; therefore, the use of keywords (hot/cold, sharp/dull, rough/smooth, etc.) or comparisons to tangible objects (soft like a teddy bear, sharp like a needle, cold like ice cube, etc.) can be helpful in establishing terminology for children during the sensory evaluation. Similar to the assessment of strength, it is necessary to develop trust with the child and comfort with the testing tools, especially when using sharp instruments (paper clip, discriminating disk, etc.). Finally, it is necessary to pay close attention to be sure the child is not using their vision to compensate during the assessment. A blindfold, parent’s hand, or piece of paper in front of the face may be necessary to ensure testing is valid.
Purpose
Sensory function requires a thorough evaluation. Specific sensory impairments should be identified along with their functional implications. For example, can the child feel the opening of the shirt to button, maintain grasp on a zipper, and provide ample force to hold a cup without dropping it?
Method
Sensory assessment should be methodical and comprehensive. Both large and small fiber nerves need to be tested in a quantitative way, and descriptions should include location, distribution, and extent of sensory impairment. Passive sensibility can be tested using the Semmes-Weinstein monofilaments or the WEST for touch pressure and the Discriminator® for static and moving two-point discrimination. Active sensibility can be tested using the Moberg picking-up test or general tests of tactile gnosis or stereognosis. Positional sense can be completed by placing the limb in space and asking the child to mimic the posture with the opposing limb or moving a finger in space and asking them whether it is up or down. Dexterity measures such as the Functional Dexterity Test (FDT) (Fig. 10) and 9-Hole Peg Test (Fig. 11) can also measure impact on hand function due to poor sensibility. The O’Riain’s Wrinkle Test is an easy way to check for denervation following a peripheral nerve injury. The therapist places the child’s hand in warm water (104 °F) for 30 min. The hand is checked for wrinkling or pruning consistent with intact sensibility. The absence of wrinkling infers the absence of nerve supply.

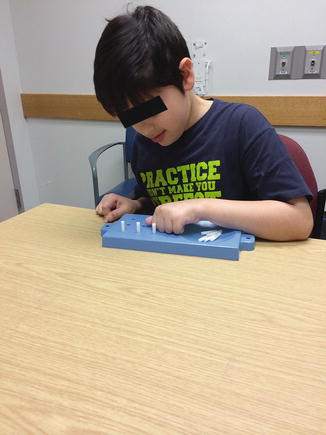

Fig. 10
Functional Dexterity Test
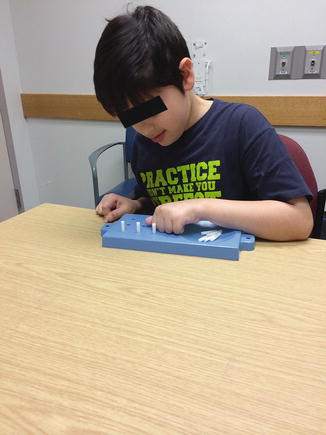
Fig. 11
Nine-Hole Peg Test
To ensure children comprehend testing procedure, it is advantageous to perform exaggerated trials at first. For example, during two-point discrimination testing, you should start with the points extremely far apart, or for light touch, a thicker monofilament should be used with a slow progression over time to a finer one. During positional sense, use large quick movements progressing to very slow subtle ones. Also, making it fun is a good way to keep the child’s interest. Telling them you are playing detective and they have to solve the mystery and pretending you are checking them for superpowers to see if they can figure out what things are without using their eyes (stereognosis testing) are useful tactics.
Sensibility
Due to their age/immaturity, children may provide several challenges during treatment, as therapeutic interventions for sensory impairment require a high degree of focus and patience. Children often disregard their insensate part. Therefore, it is imperative to use multimodal interventions to encourage usage. A child may not want to focus on their “loss” of a particular skill, but shifting the focus to an area of strength can be an empowering approach to therapy. For example, allowing the child to use their visual sense to accommodate for peripheral sensory impairments during tasks allows them to gain a degree of control over their rehabilitation and helps reinforce the therapeutic plan while working to improve performance.
Intervention
Intervention for sensory impairments varies greatly depending on the clinical presentation and stage of recovery. The intervention may be solely for protection (to prevent further injury in the case of a severe denervation injury or progressive neuropathy, spinal cord injury, etc.) or can be an active process utilizing a multisensory approach to foster hand function as reinnervation occurs. Regardless of the purpose, it is essential to imbed play in all sensory interventions to make them fun and to maintain the child’s interest and ultimately compliance with the sensory program.
Safety Awareness
In general, children have a decreased level of safety awareness, and impaired sensibility poses a further risk for accident/injury. A review of the child’s daily activities and tasks is performed to identify potential safety concerns. For example, a child with peripheral neuropathy may be at risk for burning or cutting the hand during meal preparation or injure the hand during constructive tasks, such as wood/metal work. Also, proper clothing (mittens, gloves, etc.) should be recommended to prevent injury from the cold weather. Role-playing can be beneficial to reinforce safety awareness, as it gives the therapist an opportunity to simulate unsafe situations themselves or with dolls/figurines and the child can correct the therapist by demonstrating proper safety. Finally, objects can be adapted by providing texture (Dycem, double-sided tape, rubber grips, etc.) to provide increased sensory input to prevent slippage or can be built up (with foam/rubber handle, adapted utensils, etc.) to increase the surface area for better holding.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


