Obstructive Sleep Apnea
Lane F. Donnelly, MD
DIFFERENTIAL DIAGNOSIS
Common
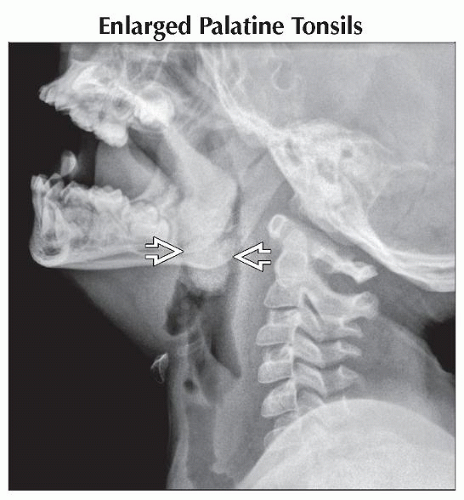
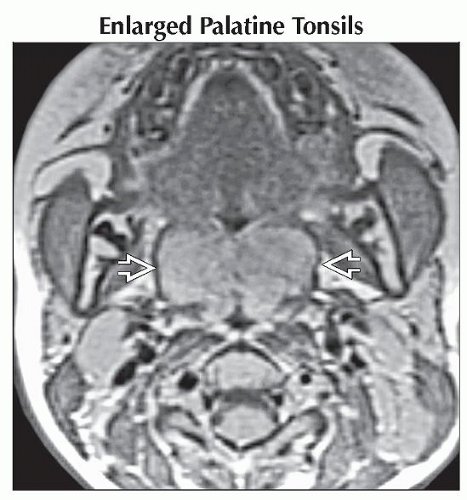
Enlarged Palatine Tonsils
Enlarged Adenoid Tonsils
Recurrent and Enlarged Adenoid Tonsils
Enlarged Lingual Tonsils
Glossoptosis
Hypopharyngeal Collapse
Less Common
Enlarged Soft Palate
Macroglossia
Rare but Important
Tongue-based Masses
Thyroglossal Duct Cyst
Artificial Airway (Mimic)
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
MR sleep studies: Combination of T1WI (static) and T2WI (static and dynamic cine)
Depict both anatomic and dynamic motion abnormalities in children with obstructive sleep apnea (OSA)
Most often performed in children who have persistent OSA despite previous surgery
e.g., previous palatine tonsillectomy and adenoidectomy
When interpreting, it is important to identify both anatomic causes (enlarged tonsils) &/or collapse patterns (glossoptosis or hypopharyngeal collapse)
2 key anatomic areas for most causes of OSA
Posterior nasopharynx
Airway bordered by soft palate anteriorly, nasal turbinates anteriorly and superiorly, adenoids posteriorly
Inferior border defined by inferior tip of uvula
Retroglossal airway
a.k.a. hypopharynx
Aerated space bordered by posterior aspect of tongue anteriorly, posterior pharyngeal wall posteriorly, and inferior aspect of soft palate anteriorly
Inferior border is inferior extent (or base) of tongue
Helpful Clues for Common Diagnoses
Enlarged Palatine Tonsils
Diagnosis made on physical inspection, not usually imaging diagnosis
Most patients referred for MR sleep studies already have had palatine tonsils removed
No published data on upper limits of normal measurement at imaging
Round, well-defined, high T2 signal masses within palatine tonsillar fossa
If appear prominent and “bob” centrally with respiration and obstruct airway → enlarged
Unlike adenoid tonsils, palatine tonsils do not recur after palatine tonsillectomy
Enlarged Adenoid Tonsils
Natural history
Adenoid tonsils are absent at birth
Reach maximum size by 2-10 years
Shrink during 2nd decade of life
Upper limit of normal size is 12 mm
Recurrent and Enlarged Adenoid Tonsils
Adenoids not encapsulated tonsil, so small amounts of lateral tonsillar tissue always left after surgery
Recurrence of adenoid 1 of more common causes of recurrent OSA
Postoperative appearance: Central wedge triangular defect in central portion of tonsil
> 12 mm in size and associated with intermittent collapse of posterior nasopharynx on cine images
Can be associated with secondary hypopharyngeal collapse secondary to negative pressure generated at obstruction of posterior nasopharynx
Enlarged Lingual Tonsils
Previously thought to be rare cause of OSA, increasingly recognized as more common
Surgically treatable; important to identify
Not always easily appreciated on physical examination
In most normal children, lingual tonsils range from nonperceptible to several mm
In patients with previous palatine tonsillectomy and adenoidectomy, lingual tonsils can grow large
High propensity in patients with Down syndrome, obesity
Appear as large, bilateral, high T2 signal masses at base of tongue
Can grow into 1 large dumbbell-shaped mass
Can grow superiorly into palatine fossa
Potentially confused with palatine tonsils if history of palatine tonsillectomy not known
Glossoptosis
Defined as posterior motion of tongue during sleep
Tongue is posteriorly positioned, and posterior wall of tongue abuts posterior pharyngeal wall, obstructing retroglossal airway
Tongue may also displace soft palate posteriorly and obstruct nasopharynx
Occurs in children with macroglossia (large tongue), micrognathia (small mandible), or decreased muscular tone
e.g., Down syndrome, Pierre-Robin sequence, cerebral palsy
Axial cine images show posterior motion of tongue but no change in left-to-right transverse diameter of retroglossal airway
Important to differentiate glossoptosis from hypopharyngeal collapse as there are more and better surgical options for glossoptosis
Hypopharyngeal Collapse
Primarily related to decreased muscular tone
Secondary to negative pressure, secondary to more superior obstruction (e.g., enlarged adenoids)
Axial cine images show dynamic and cylindrical narrowing of hypopharynx
All walls (left, right, anterior, posterior) collapse to center of retroglossal airway
Helpful Clues for Less Common Diagnoses
Enlarged Soft Palate
Thickened and long soft palate possible cause of OSA
No established quantitative imaging criteria for when soft palate too long or thick
If soft palate draped over tongue and associated with collapse of airway on cine images → enlarged
Edema from snoring can occur
Appears as increased T2 signal in soft palate centrally
Soft palate normally same signal intensity of tongue musculature, dark on T2
Helpful Clues for Rare Diagnoses
Artificial Airway (Mimic)
Obscures and distorts anatomic structures being evaluated
May simulate pathology
Try to avoid artificial airway when acquiring MR sleep studies
Image Gallery
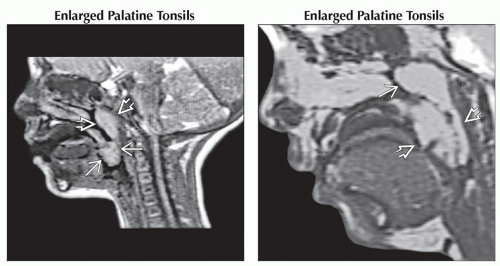 (Left) Sagittal T2WI FSE MR shows several high signal masses, which are enlarged adenoid
 and palatine tonsils and palatine tonsils  . (Right) Sagittal GRE MR shows enlargement of the palatine . (Right) Sagittal GRE MR shows enlargement of the palatine  and adenoid and adenoid  tonsils. tonsils.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|