Background
Noninvasive prenatal screening has become an increasingly prevalent choice for women who desire aneuploidy screening. Although the test characteristics are impressive, some women are at increased risk for noninvasive prenatal screen failure. The risk of test failure increases with maternal weight; thus, obese women may be at elevated risk for failure. This risk of failure may be mitigated by the addition of a paternal cheek swab and screening at a later gestational age.
Objective
The purpose of this study was to evaluate the association among obesity, gestational age, and paternal cheek swab in the prevention of screening failure.
Study Design
A retrospective cohort study was performed for women who were ≥35 years old at delivery who underwent screening at NorthShore University HealthSystem, Evanston, IL. Maternal weight, body mass index, gestational age, and a paternal cheek swab were evaluated in univariate and multivariable logistic regression analyses to assess the association with failed screening.
Results
Five hundred sixty-five women met inclusion criteria for our study. The mean body mass index was 25.9 ± 5.1 kg/m 2 ; 111 women (20%) were obese (body mass index, ≥30 kg/m 2 ). Forty-four women (7.8%) had a failed screen. Obese women had a failure rate of 24.3% compared with 3.8% in nonobese women ( P < .01). Gestational age was not associated with failure rate (mean ± standard deviation, 13 ± 3 weeks for both screen failure and nonfailure; P = .76). The addition of a paternal cheek swab reduced the failure rate from 10.2% in women with no swab to 3.8% in women with a swab ( P < .01). In multivariable analysis, obesity and lack of a paternal cheek swab were independent predictors of screen failure (odds ratio, 9.75; 95% confidence interval, 4.85–19.61; P < .01; and odds ratio, 3.61; 95% confidence interval, 1.56–8.33; P < .01, respectively).
Conclusion
The addition of a paternal cheek swab significantly improved noninvasive prenatal screen success rates in obese women. However, delaying testing to a later gestational age did not.
Noninvasive prenatal screening (NIPS) is a recently developed technology that uses fetal cell-free DNA (cfDNA) that is detected in maternal serum to screen for fetal aneuploidy. According to a recent metaanalysis, NIPS has demonstrated a high sensitivity of 99.2% for trisomy 21, 96.3% for trisomy 18, 91.0% for trisomy 13, 90.3% for monosomy X, and 93.0% for other sex chromosome aneuploidies. However, despite these compelling test characteristics, the test is limited by the potential for test failure.
Test failures commonly occur as a result of a low cfDNA fraction, with a reported failure rate as high as 6.1%. Typically, fetal DNA comprises 10–15% of the total cfDNA in the maternal circulation during the late first and early second trimesters, when prenatal screening is usually performed. This proportion increases throughout gestation at a rate of 0.10% weekly from 10-21 weeks and then increases sharply to a rate of 1% weekly after 21 weeks of gestation.
When the fetal fraction is <4%, there is insufficient fetal cfDNA for most methods to produce a reliable result. The relationship between maternal weight and fetal fraction has been well-documented: as maternal weight increases, fetal fraction decreases. For women who weigh >250 lb, the likelihood of failure increases to ≥10%. Conversely, the use of paternal DNA that is obtained via a cheek swab has been reported to improve the likelihood of obtaining a result when implemented with the Panorama Next Generation Aneuploidy Test Using SNPs algorithm (NATUS; Natera Inc, San Carlos, CA), particularly when the fetal fraction approaches the lower limit of 4%. Panorama has the lowest false-negative rate (0.7%) in published clinical trials. They measure fetal fraction and adjust their algorithm accordingly to improve sensitivity, even at low fetal fractions. Panorama also has a higher fail rate (approximately 5%), compared with reported rates that use other platforms, that further underscores the importance of understanding factors that contribute to failure and potential approaches to mitigate the risk of failure.
In our study, we sought to determine how to optimize our screening approach for women ≥35 years old without additional risks of aneuploidy to minimize the risk of NIPS test failure. We aimed to evaluate the association between gestational age, obesity, and the addition of a paternal cheek swab in the prevention of NIPS failure. We hypothesize that the NIPS failure rate will decrease with the addition of a paternal cheek swab and when screening is pursued later in pregnancy because of the anticipated higher fetal fraction.
Materials and Methods
A retrospective cohort study was performed for all women who were ≥35 years old at delivery and who underwent NIPS at NorthShore University HealthSystem. The following exclusion criteria were used: <10 weeks gestational age at screening, a first-trimester pregnancy loss, and additional high-risk factors, such as an abnormal ultrasound scan results or abnormal multiple marker serum screening. Maternal weight at initial screening was used, and obesity was defined as a body mass index (BMI) of ≥30 kg/m 2 . A paternal cheek swab was submitted with the maternal blood sample when available. Of note, women were not asked specifically to bring their partners to their visit, because a paternal cheek swab was not used routinely during this time.
All screens in this study were performed via Panorama screen, which uses a method of NIPS that specifically amplifies and sequences single-nucleotide polymorphisms (SNPs), and thus can differentiate between maternal and fetal haplotypes. Panorama’s proprietary, patented algorithm is called NATUS. Each specimen that is submitted must pass a series of quality control metrics to ensure that the DNA is sufficient to obtain a result. The laboratory requests an additional blood sample when certain metrics are not met, such as low quantity of DNA or poor quality of DNA because of contamination. There are other circumstances when a redraw is not indicated because it would not change the laboratory’s ability to obtain a result, such as an internal maternal characteristics. Patients who had test failures that were attributed to intrinsic maternal characteristic were not included in this analysis. Failures because of intrinsic maternal characteristics could be secondary to the presence of regions of loss of heterozygosity in maternal DNA that exceeded 25% of the chromosome. Therefore, a redraw would not be helpful. This characteristic is specific to the Panorama screen, because Natera Inc is the only company that uses SNP-based sequencing.
NorthShore University HealthSystem Research Institute’s Institutional Review Board approved this study. BMI and gestational age were evaluated as continuous variables and as categoric variables. Patient characteristics were compared between those whose NIPS testing was successful vs those with a test failure. Categoric variables were compared with the use of chi-square test or Fisher’s exact test (for small cell size). Continuous variables were compared with the use of the Student t test or Mann-Whitney U test for nonparametric distributions. Pearson or Spearman correlation coefficients evaluated the correlations between failure, weight (at initial screening), BMI (at initial screening), gestational age (at initial screening), availability of a paternal swab, and fetal fraction. Logistic regression models were constructed to evaluate predictors of NIPS failure. Variables from the univariate analysis with a probability value of <.10 were entered into a multivariable model with manual backwards selection. Gestational age as a categoric variable (less or greater than or equal to 20 completed weeks of gestation) was forced into the final model determined a priori for clinical importance. Weight in pounds, BMI, and the presence of obesity were evaluated in separate multivariable regression models. The model with the highest c-statistic and best-fit statistics was chosen as the final multivariable model. All interaction effects were evaluated. Statistical analyses were conducted with SAS software (version 9.3; SAS Inc, Cary, NC).
Results
There were 686 subjects who had NIPS at NorthShore University HealthSystem in the time period January 13, 2013, through April 3, 2014. Of those, 567 women (82.7%) were considered high-risk based on maternal age (≥35 years old) at delivery alone. Two subjects had test failures because of intrinsic maternal characteristics and were excluded from the analysis. The remaining 565 patients comprised our study population. The mean maternal age was 37.7 ± 2.4 years, and the mean gestational age at initial screening was 12.7 ± 2.7 weeks ( Table 1 ). Most patients in our study self-identified as white (67.1%) and underwent NIPS from 10-12 weeks of gestation (65.3%; Table 1 ). The mean BMI was 25.9 ± 5.1 kg/m 2 , with an obesity prevalence of 19.9% ( Table 1 ).
| Characteristic | Total | Success | Failure | P value |
|---|---|---|---|---|
| Total no. of women, n (%) | 565 | 521 (92.2) | 44 (7.8) | |
| Maternal age, y ± SD | 37.7 ± 2.4 | 37.7 ± 2.4 | 38.2 ± 2.9 | .27 |
| Race, n (%) | .20 | |||
| White | 379 (67.1) | 354 (68.0) | 25 (56.8) | |
| Black | 13 (2.3) | 11 (2.1) | 2 (4.5) | |
| Asian | 81 (14.3) | 73 (14.0) | 8 (18.2) | |
| Hispanic | 54 (9.6) | 51 (9.8) | 3 (6.8) | |
| Other | 38 (6.7) | 32 (6.1) | 6 (13.6) | |
| Nulliparous, n (%) | 113 (20.1) | 106 (20.4) | 7 (15.9) | .47 |
| Gestational age, wk ± SD | 12.7 ± 2.7 | 12.7 ± 2.7 | 12.5 ± 3.3 | .76 |
| Gestational age bracket, n (%) | .68 | |||
| 10–12 Wk | 369 (65.3) | 338 (64.9) | 31 (70.5) | |
| 13–15 Wk | 129 (22.8) | 120 (23.0) | 9 (20.5) | |
| 16–20 Wk | 49 (8.7) | 47 (9.0) | 2 (4.5) | |
| >20 Wk | 18 (3.2) | 16 (3.1) | 2 (4.5) | |
| Maternal weight, lb ± SD | 154.3 ± 31.5 | 151.4 ± 27.8 | 187.9 ± 48.7 | <.01 |
| Body mass index, kg/m 2 ± SD | 25.9 ± 5.1 | 25.5 ± 4.6 | 31.2 ± 7.7 | <.01 |
| Obese, n (%) | 111 (19.9) | 84 (16.4) | 27 (61.4) | <.01 |
| Fetal fraction, % ± SD | 10.2 ± 4.3 | 10.8 ± 4.0 | 3.4 ± 1.9 | <.01 |
| Noninvasive prenatal screening, n (%) | ||||
| High risk | 11 (2.0) | 11 (2.1) | 0 | .99 |
| Low risk | 511 (90.4) | 510 (97.9) | 1 (2.3) | <.01 |
| Paternal swab, n (%) | 211 (37.4) | 203 (39.0) | 8 (18.2) | <.01 |
Of the 565 subjects, 521 subjects (92.2%) had successful results; the remaining 44 subjects (7.8%) had test failures ( Table 1 ). Of the 521 results, 11 results (2.1%) returned as high risk for aneuploidy. Of these 11, 6 results were at high risk for trisomy 21. Three of these patients declined prenatal diagnostic testing and were lost to follow up; the remaining 3 patients had the diagnosis of fetal trisomy 21 confirmed by chorionic villus sampling or amniocentesis. Five patients were at high risk for trisomy 18. One of these patients underwent a chorionic villus sampling with a normal fetal 46 XX karyotype without any abnormalities noted at birth. One patient was found to have multiple fetal anomalies with a term intrauterine fetal demise. Karyotypic analysis was not obtained. The remaining 3 patients had confirmed fetal trisomy 18 by chorionic villus sampling or amniocentesis. Of the 44 test failures, 24 (55%) underwent repeat testing; the remainder declined. Of these 24 redraws, 18 results (75%) returned as low-risk; 5 results (21%) failed to return a result, and 1 result (4%) returned as high-risk for trisomy 21. Of the 5 redraws that again failed to yield a result, 1 patient had an amniocentesis that confirmed trisomy 18; 3 patients declined prenatal diagnostic testing, and all 3 had healthy-appearing infants. One patient moved to another state, and the outcome results were not available. The 1 patient who had high risk for trisomy 21 declined prenatal diagnostic testing and was lost to follow up.
We compared maternal and test characteristics of those with an initial failed test result with those with successful test results ( Table 1 ); of note, we did not include the redraw samples in the statistical analyses. Maternal age, race, ethnicity, and gestational age at the time of screening were comparable between those women who had successful tests and those who had test failures. As expected, the mean fetal fraction for those with a failed result was significantly lower (3.4 ± 1.9%) than those with a successful result (10.8 ± 4.0%; P < .01). In addition, the average weight of women with a failed result was significantly higher than those women with a successful test (188 ± 49 lb vs 151 ± 28 lb, respectively; P < .01). Similarly, the prevalence of obesity was higher among women with a failed test result as compared with those with a successful test result (61.4% vs 16.4%, respectively), with a failure rate of 24.3% (27/111 women) among obese women compared with 3.7% (17/454 women) in nonobese women ( P < .01). The failure rate increased dramatically as BMI increased, with a failure rate of 7.1% at a BMI of 28–29.9 kg/m 2 increasing to 50.0% at a BMI of ≥40 kg/m 2 ( P < .01; Figure 1 ).
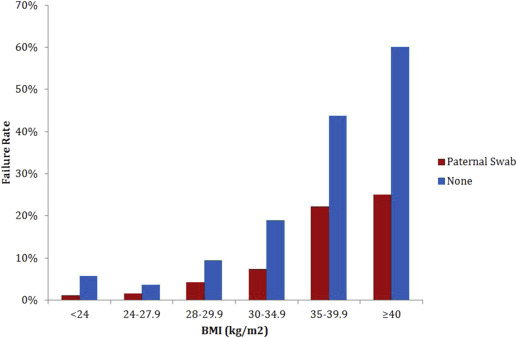
We also evaluated the impact of the addition of paternal cheek swab on test failure. The use of a paternal cheek swab was more frequent in successful tests than in those tests that failed (39.0% as compared with 18.2%, respectively; P < .01). When a paternal cheek swab was performed, the failure rate was 8 of 211 tests (3.8%) as compared with 36 of 353 tests (10.2%) when a cheek swab was not performed ( P < .01). The addition of a paternal swab decreased the failure rate among obese women from 22 of 67 (32.8%) to 5 of 43 (11.6%; P = .01). Although the addition of a paternal cheek swab improved test performance across all BMI groups, the impact was greatest among obese women ( Figure 1 ). In nonobese women, the addition of a paternal cheek swab decreased the failure rate from 14 of 279 (5.0%) to 3 of 167 (1.8%), which did not reach statistical significance ( P = .09).
In univariate analysis, greater fetal fraction, lower maternal weight, nonobese status, and use of paternal cheek swab significantly decreased the likelihood of a screen failure ( Table 2 ). Fetal fraction was correlated positively with gestational age (Spearman correlation coefficient: r = 0.13; P < .01) and negatively correlated with BMI ( r = –0.42; P < .01).



