10 Nutrition and Gastroenterology
Nutrition
Normal Infant Nutrition and Growth
The first year of life is marked by unprecedented growth when compared with any other period of life. Within the first 6 months birth weight generally doubles and by 1 year triples, with length close to doubling. As such, the normal caloric and protein requirements for growth are accordingly higher (Table 10-1). The fuel for this growth is human breast milk or formulas that have been derived to simulate the major components of breast milk. Beyond convenience and cost, there has been a growing consensus and acceptance that breast milk offers advantages that formulas to date cannot emulate (Table 10-2). Although generally considered nutritionally replete, breast milk lacks substantial amounts of vitamin D and fluoride, requiring supplementation from a multivitamin. Low amounts of vitamin K stores at birth and in breast milk have led to a standard practice of intramuscular vitamin K injection at birth. Breast milk also contains a lower amount of iron, albeit in a bioavailable form, requiring additional supplementation via a multivitamin or solid food as an infant uses the iron stores obtained in utero and reaches a physiologic nadir in the second half of the first year of life. Standard infant formulas do contain sufficient iron, vitamin K, and vitamin D and when diluted in fluoridated water are nutritionally replete. There has been a virtual explosion of the varieties of formulas available for infant feeding. Many of the “niche” formulas are designed for specific gastrointestinal illnesses and therefore are not necessary for standard infant feeding. Table 10-3 categorizes the elements of the most common variants of infant formulas used today. Although whole cow’s milk and other forms of mammalian milk have features similar to human breast milk, they include a higher protein concentration and thus higher renal solute load; the American Academy of Pediatrics recommends that their use be delayed until an infant is 12 months of age.
Table 10-1 Nutritional Requirements
| Age | Calories (kcal/kg/d) | Protein (g/kg/d) |
|---|---|---|
| 0-6 mo | 100-120 | 2.5-3.0 |
| 6-12 mo | 90-100 | 2.0-2.5 |
| 1-7 yr | 75-90 | 1.5-2.0 |
| 7-12 yr | 60-75 | 1.5-2.0 |
| 12+ yr | 30-60 | 1.0-1.5 |
Table 10-2 Advantages of Breast-feeding
Table 10-3 Considerations in Choosing a Formula
| Carbohydrate Source |
| Protein Source |
| Fat Source |
| Additives |
| Other Considerations |
ARA, arachidonic acid; DHA, docosahexaenoic acid; LCT:MCT ratio, long-chain to medium-chain triglyceride ratio.
Normal Childhood/Adolescent Nutrition and Growth
As an infant reaches 12 months of age, the caloric requirements necessary for growth continue to diminish as the rate of growth decreases (see Table 10-1). Solid foods, typically introduced around the fourth month of life, take on the role as a major source of calories and nutrients and formula is typically replaced by whole cow’s milk. Psychological and behavioral aspects of feeding from both the toddler’s and caregiver’s perspective take on new roles and are a common topic of discussion during health care visits. Variations of feeding patterns that do not affect growth but may lead to gastrointestinal symptoms are often recognized during this time period. Careful nutritional assessment, including dietary monitoring and simple anthropometric monitoring, continues to be essential as a marker of general health to recognize tendencies in undernutrition, overnutrition, and the recognition of both acute and chronic disease. Monitoring of nutrition continues to be important throughout childhood and adolescence as dietary habits are established, to promote overall healthy choices that remain well beyond childhood and into adult life.
Basic Monitoring of Growth and Nutrition
Growth assessment has been and continues to be commonplace in pediatric practice as both a surrogate for nutritional adequacy and general health status. Growth charts are the means by which to monitor simple anthropometric data to achieve this goal. Nationally standardized growth charts, in use since 1977, were updated in 2000 (see Chapter 9, Fig. 9-1), using data from the National Health and Nutrition Examination Survey III (NHANES III) as well as previous versions of the survey and other primary sources to obtain a percentage-based distribution of growth over a large cross-sectional population. The updated version continues to use weight for age, length/height for age, and occipital–frontal circumference for age, and has added normative data for body mass index for age after 2 years of age. The inclusion of body mass index [weight (kg)/height (m)2] is in response to the growing epidemic of overnutrition as a measure of obesity. Other reasons for the updated changes include additional data that were previously lacking in the infant age range. As a distribution based on percentages, it should always be recognized that by definition, there will always be a population that is over the greatest isopleth (>97th percentile) and under the lowest isopleth (<3rd percentile). Despite this, the characteristics of growth of a child over time can be an invaluable comparative measure of what would be considered normal growth to actual growth. Growth charts have been developed for specialized populations such as infants with trisomy 21 and premature infants. Care must be taken when using these growth charts, as the numbers of patients in the sample section are less than in the standard growth charts.
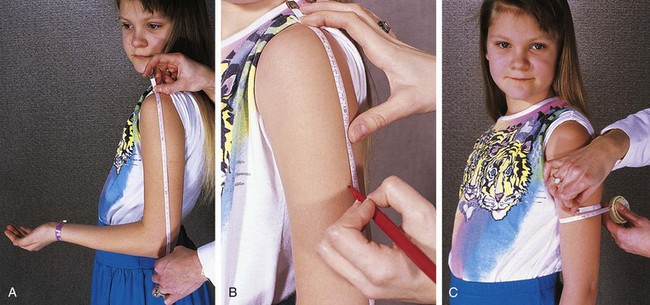
Other measurements, such as triceps skinfold thickness (Fig. 10-1) and midarm circumference (Fig. 10-2), when done by a well-trained, experienced examiner can be useful when growth charts are insufficient. Examples of this would include infants with end-stage liver disease and marked ascites or vascular malformations/hypertrophy of an organ or appendage, which falsely elevates true body weight. For the great majority of infants and children, growth charts are usually sufficient to assess overall growth.
Malnutrition States
Malnutrition results from an imbalance between the intake and/or absorption of calories and the consumption of calories required for growth. Obesity is the result of overnutrition and has grown to epidemic proportions in the United States and other developed nations. Obesity, in the context of both overnutrition and hormonal imbalance, is discussed in Chapter 9. Undernutrition results from inadequate intake, absorption, or digestion of nutrients, or insufficient intake for increased metabolic needs. Careful plotting of height, weight, and body mass index as a function of time on a standard growth chart greatly aids in the diagnosis of malnutrition. The Waterlow criteria assess undernutrition by plotting weight for height, as a measure of current nutritional status, and height for age, which reflects the chronicity of the malnutrition.
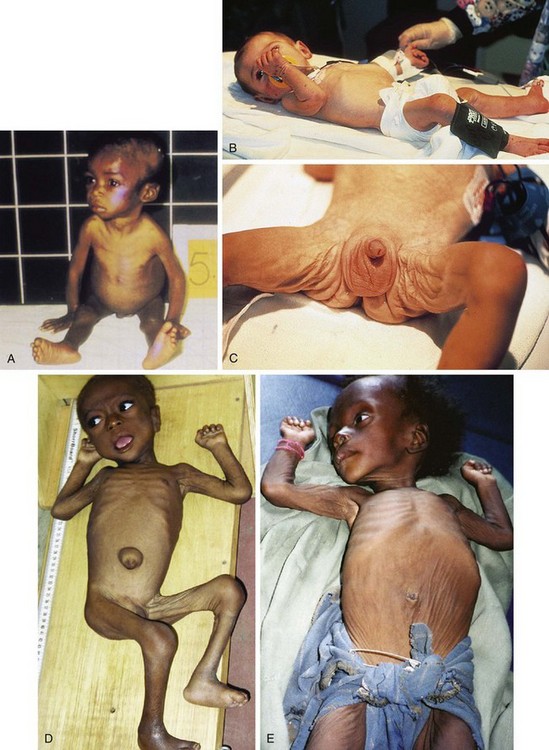
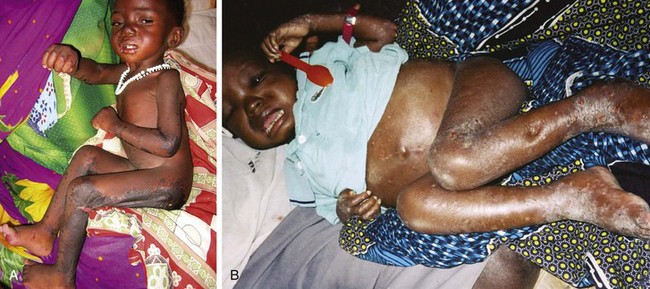
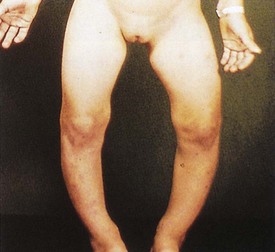
A traditional classification of extreme protein energy malnutrition includes marasmus, kwashiorkor, and marasmic kwashiorkor. Marasmus, defined as predominantly caloric/energy deficiency, is characterized by marked emaciation; loss of subcutaneous fat and muscle; brittle, sparse hair; and poor nail growth (Fig. 10-3). Diarrhea is common as intestinal cell turnover is blunted due to lack of energy (Fig. 10-4). Secondary effects of marasmus, such as hypothermia and bradycardia, occur late in the clinical course. Marasmus is usually seen within the first year of life at the time of weaning, during famine, or at any time when there is a consistent and extreme deprivation of calories. It is the consequence of poor caloric, protein, vitamin, and mineral intake. Kwashiorkor, on the other hand, results from a diet rich in calories but lacking protein. The initial “moon face” of kwashiorkor is often mistaken for proper nutrition. The child is often edematous, which becomes strikingly apparent after nutritional repletion (Fig. 10-5). Hepatomegaly and mental status changes are common. Skin changes in patients with kwashiorkor include hyper- or hypopigmentation with a scaly, weeping dermatitis that may ulcerate and desquamate (Fig. 10-6). The rash is often more prominent in areas that are chronically irritated (e.g., the infant’s groin and areas of peripheral edema) (Fig. 10-7). In marasmic kwashiorkor, both patterns of malnutrition may develop together, resulting in a combination of clinical features.
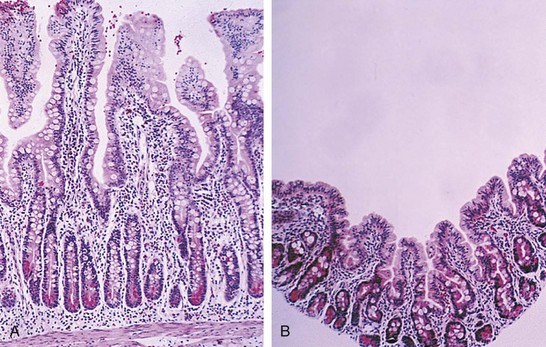
Figure 10-4 Gastrointestinal tract injury associated with malnutrition. A, Normal jejunal mucosa with tall villi and deep crypts. B, Blunted villi lead to chronic diarrhea and malnutrition. Note the lack of increase in crypt depth and lymphocytic infiltrate seen in celiac disease (see Fig. 10-28) and other diseases with active cell turnover.
Failure to Thrive
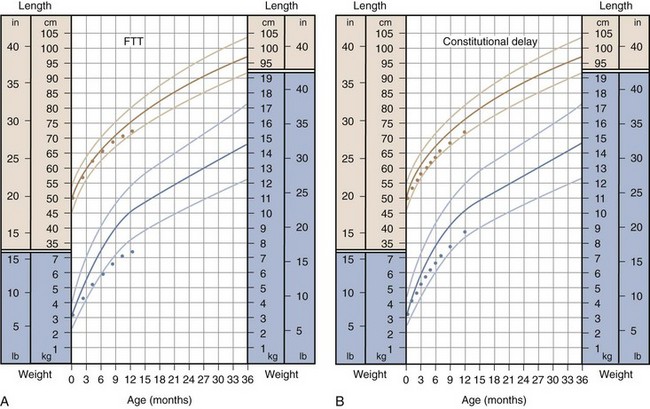
The term failure to thrive is a descriptive term used to depict inadequate weight gain over time, often used when weight for age crosses two percentile isopleths or when weight for age falls below the 3rd percentile for age. As previously stated, caution must be used when weight gain consistently tracks below the 3rd percentile, as this may reflect a normal growth pattern based on standard weight distribution patterns (Fig. 10-8). Most failure to thrive, by Waterlow criteria, is marked by decreased weight for height, with initial sparing of height for age and head circumference for age, with gradual loss in height and head circumference for age as the undernourished state continues. A more accurate description of this abnormal pattern of growth can be classified as inadequate intake, maldigestion, malabsorption, ineffective use of calories, or increased metabolic demand. Table 10-4 lists some of the more common diagnoses associated with failure to thrive. At times, the etiology can be mixed as an underlying diagnosis may be compounded by inadequate intake secondary to its presenting symptoms.
Table 10-4 Common Etiologies of Failure to Thrive
| Inadequate Intake | Inadequate Absorption | Increased Caloric Needs |
|---|---|---|
| Caloric deprivation Behavioral feeding disorders Disorders of swallowing | Celiac disease Intestinal inflammation Fat malabsorption (cystic fibrosis) | Congenital heart disease |
| Chronic pulmonary disease | ||
| Malignancy | ||
| Vomiting/reflux | Chronic diarrhea | Renal disease |
| Anorexia/poor appetite | Genetic disease |
Therapy for malnutrition is twofold. All attempts should be made to treat the underlying cause of the symptoms. As important, nutritional rehabilitation through the provision of sufficient calories for growth should be implemented once malnutrition is recognized. Care must be undertaken when providing nutritional rehabilitation, as one consequence of aggressive therapy is the refeeding syndrome (Table 10-5).
Table 10-5 Considerations in the Refeeding Syndrome
| Physiologic |
| Electrolyte Abnormalities |
| Monitoring |
Specific Nutrient Deficiencies
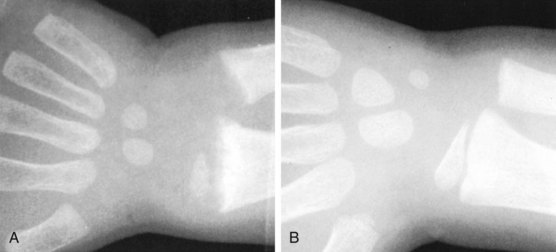
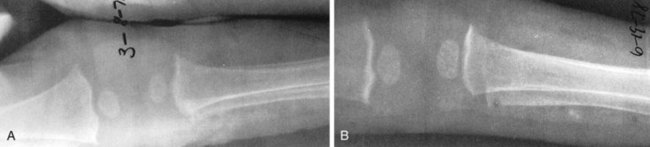
In addition to more general malnutrition states, either excess or deficiencies of specific nutrients, vitamins, and minerals can be seen in isolation or as complicating factors of chronic disease (Table 10-6). For example, fat-soluble vitamin deficiency (vitamins A, D, E, and K) can be found with fat malabsorption or in isolation due to inadequate intake. Vitamin D is essential for normal calcium, phosphorus, and magnesium homeostasis. Vitamin D deficiency may lead to rickets, the inadequate mineralization of growing bones, and osteomalacia. There is growing evidence that it also plays a role in various physiologic functions including immune function, and deficiency has been associated with risk for osteoporosis, heart disease, various cancers, type 1 diabetes, and multiple sclerosis later in life. Classic vitamin D deficiency presents at weight-bearing age and results in poor growth, curvature of weight-bearing bones (Fig. 10-9), widening of epiphyses, and costochondral “rachitic rosary” beading (Fig. 10-10). Craniotabes, or softening of the skull, may be seen in infants. With appropriate vitamin and mineral supplementation, resolution occurs followed by bone remodeling (Fig. 10-11). Common laboratory findings are summarized in Table 9-5. Vitamin D deficiency is especially prevalent in breast-fed infants, infants with darker skin, and infants and children with decreased sun exposure. Poor absorption in children with cholestasis, Crohn disease, cystic fibrosis, and celiac disease and abnormal hydroxylation in end-stage renal disease place these populations at risk as well. In fact, the preponderance of vitamin D deficiency without rickets places otherwise healthy children and adolescents at risk if they are not consuming the recommended daily allowance in dairy and other vitamin D–fortified foods. Whereas the recommended daily intake was 200 IU/day, the American Academy of Pediatrics has now recommended intake of 400 IU/day to prevent complications of vitamin D deficiency. Other fat-soluble vitamin deficiencies are seen in patients with fat malabsorption such as cholestatic liver disease and cystic fibrosis. Vitamin K deficiency results in prolongation of the prothrombin time and international normalized ratio (INR). PIVKA (elevations of proteins induced by vitamin K absence) may detect subclinical vitamin K deficiency, but are not done on a routine basis. Supplementation of vitamin K either orally, or, in some cases, intramuscularly is indicated in vitamin K deficiency. Vitamin A deficiency can lead to night blindness, xerophthalmia, follicular hyperkeratosis, or Bitot spots. Vitamin E deficiency is marked by absence of deep tendon reflexes and subsequent ataxia. It has also been linked to hemolysis and possible retinopathy of prematurity. Isolated deficiencies of vitamins A and E are rare and are generally found in the context of fat-soluble vitamin malabsorption. Water-soluble vitamin deficiencies are also uncommon unless unintentionally excluded in the diet. For example, an infant fed goat’s milk, instead of breast milk or a cow’s milk–based formula, is at risk for folate deficiency. One notable exception is vitamin B12, which requires active uptake in the terminal ileum. Patients with terminal ileum disease or resection are at particular risk of vitamin B12 deficiency, which results in a macrocytic anemia (see Chapter 11, Fig. 11-9), hypersegmented neutrophils (see Chapter 11, Fig. 11-10), and/or neurologic findings due to poor myelination of nerve fibers. Neurologic findings when detected early can be reversible. Supplementation is either intramuscular or (more recently) through intranasal mucosal absorption; the latter is generally reserved for adolescents and adults.
Table 10-6 Nutritional Deficiencies with Characteristic Physical Signs
| Vitamin/Mineral | Sign/Symptom |
|---|---|
| Calcium, phosphorus, vitamin D | Rickets/osteomalacia |
| Vitamin A | Night blindness, xerophthalmia, Bitot spots, follicular hyperkeratosis |
| Vitamin C | Scurvy: bone lesions, bleeding |
| Vitamin E | Hemolytic anemia, peripheral neuropathy |
| Vitamin K | Petechiae, ecchymoses |
| Thiamine (vitamin B1) | Beriberi: heart failure, increased intracranial pressure |
| Niacin | Pellagra: dermatitis (sun-exposed areas) |
| Riboflavin (vitamin B2) | Angular stomatitis, cheilosis |
| Vitamin B6 | Anemia, dermatitis, neuropathy |
| Vitamin B12 | Anemia, neuropathy |
| Folate | Anemia |
| Iron | Anemia, koilonychia |
| Biotin | Rash, hair loss |
| Essential fatty acids | Rash, coagulopathy |
| Zinc | Rash (acrodermatitis), growth failure, delayed sexual development, ageusia |
| Copper | Bone changes, hypopigmentation, anemia, neutropenia |
| Selenium | Cardiomyopathy (Keshan disease) |
Other specific nutritional deficiencies can sporadically occur in the pediatric population, especially when receiving nontraditional diets. Patients on extremely low-fat diets or who are receiving exclusive parenteral nutrition, in which standard fat emulsions have been limited/omitted because of concern about cholestasis, can present with essential fatty acid deficiency. α-Linolenic acid (ω-3) and linoleic acid (ω-6) are the essential fatty acids, whereas several others may be considered conditionally essential. Symptoms include a scaly dermatitis and dull, brittle hair and nails. Diagnosis can be suggested on the basis of triene:tetraene ratios. Zinc deficiency encountered in diarrheal diseases and in burns can result in alopecia, diarrhea, and acrodermatitis. Copper, which is often reduced in the diets of patients with chronic liver disease, can present as irritability, bone pain, decreased hair pigmentation, anemia, and neutropenia (Fig. 10-12). Copper deficiency can be diagnosed by serum copper levels and depressed ceruloplasmin. A weeping dermatitis in the perioral, perianal, and eyelid area along with lethargy and malaise has been described in patients with a suspected deficiency in biotin (Fig. 10-13), a conditionally essential amino acid. Further signs and symptoms of specific nutrient deficiencies can be found in Table 10-6.
Gastroenterology
Reflux
GER associated with one or more concurrent morbidities is often termed gastroesophageal reflux disease (GERD). The symptoms often associated with GERD include irritability/fussiness, heartburn, poor weight gain, upper respiratory symptoms, and wheezing (Table 10-7). Apnea and bradycardia have been associated with reflux in the preterm infant, although these episodes usually resolve as an infant reaches term. Sandifer syndrome is described as abnormal posturing and back arching in response to GER and is an uncommon manifestation. Rumination, not typically considered reflux, is the voluntary contraction of abdominal musculature that leads to episodes that manifest similar to reflux. It is generally regarded as a self-stimulating disorder and is more common in adolescence and in various behavioral disorders.
Table 10-7 Presentations of Gastroesophageal Reflux
| Regurgitation |
| Esophagitis |
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|