Nonalcoholic fatty liver disease (NAFLD) is considered the hepatic manifestation of metabolic syndrome and has become the most common form of chronic liver disease in children and adolescents. The histologic spectrum of NAFLD is broad ranging, from the relatively benign form of simple steatosis to the aggressive form of nonalcoholic steatohepatitis, eventually leading to fibrosis and cirrhosis. NAFLD has also been recognized as an independent risk factor for extrahepatic complications, such as cardiovascular disease, type 2 diabetes mellitus, sleep disorders, and osteoporosis. In this review, we discuss both the hepatic and extrahepatic complications of NAFLD in children.
Key points
- •
Nonalcoholic fatty liver disease (NAFLD) includes a broad spectrum of liver diseases ranging from simple steatosis to nonalcoholic steatohepatitis with further progression to fibrosis or cirrhosis.
- •
Liver biopsy still remains the gold standard for the diagnosis of NAFLD.
- •
Noninvasive diagnostic methods, such as serum markers or imaging, are still not well established or validated for children with NAFLD.
- •
NAFLD is associated with multiple extrahepatic complications, such as cardiovascular disease, type 2 diabetes, sleep disorders, and osteoporosis.
- •
Clinicians should be aware of these extrahepatic complications to ensure prompt screening and treatment.
Introduction
With the increasing trend in obesity, nonalcoholic fatty liver disease (NAFLD) has now become the most common cause of chronic liver disease in children and adolescents, with a prevalence of 3% to 10% in the general pediatric population increasing to up to 70% in obese children. NAFLD is a clinicopathologic entity that encompasses a broad spectrum of liver injury ranging from accumulation of fat in the liver (simple steatosis) to the potentially progressive form of nonalcoholic steatohepatitis (NASH) characterized by hepatocyte ballooning and inflammation, and is often associated with fibrosis. NAFLD can cause decompensated cirrhosis requiring liver transplantation and hepatocellular carcinoma even in children.
Although NAFLD increases the risk of liver-related mortality and morbidity, the most common causes of death among patients with NAFLD are cardiovascular disease (CVD) and extrahepatic malignancy. This has led to an increasing awareness of extrahepatic complications associated with NAFLD. NAFLD is often considered a hepatic manifestation of metabolic syndrome (MetS); however, emerging data indicate that NAFLD can be a risk factor for the development of MetS, type 2 diabetes mellitus (DM), and CVD. Similarly, NAFLD is shown to be associated with other extrahepatic complications, such as chronic kidney disease, hypothyroidism, polycystic ovarian syndrome, obstructive sleep apnea (OSA), osteoporosis, and colorectal cancer in adults. In children, recent evidence suggests that pediatric NAFLD is associated with individual extrahepatic complications, such as CVD, type 2 DM, retinopathy, vitamin D deficiency, and low bone mineral density.
Introduction
With the increasing trend in obesity, nonalcoholic fatty liver disease (NAFLD) has now become the most common cause of chronic liver disease in children and adolescents, with a prevalence of 3% to 10% in the general pediatric population increasing to up to 70% in obese children. NAFLD is a clinicopathologic entity that encompasses a broad spectrum of liver injury ranging from accumulation of fat in the liver (simple steatosis) to the potentially progressive form of nonalcoholic steatohepatitis (NASH) characterized by hepatocyte ballooning and inflammation, and is often associated with fibrosis. NAFLD can cause decompensated cirrhosis requiring liver transplantation and hepatocellular carcinoma even in children.
Although NAFLD increases the risk of liver-related mortality and morbidity, the most common causes of death among patients with NAFLD are cardiovascular disease (CVD) and extrahepatic malignancy. This has led to an increasing awareness of extrahepatic complications associated with NAFLD. NAFLD is often considered a hepatic manifestation of metabolic syndrome (MetS); however, emerging data indicate that NAFLD can be a risk factor for the development of MetS, type 2 diabetes mellitus (DM), and CVD. Similarly, NAFLD is shown to be associated with other extrahepatic complications, such as chronic kidney disease, hypothyroidism, polycystic ovarian syndrome, obstructive sleep apnea (OSA), osteoporosis, and colorectal cancer in adults. In children, recent evidence suggests that pediatric NAFLD is associated with individual extrahepatic complications, such as CVD, type 2 DM, retinopathy, vitamin D deficiency, and low bone mineral density.
Hepatic complications
Clinical Manifestations
Children with NAFLD are usually diagnosed because of incidental elevation in liver enzymes or evidence of steatosis on ultrasound done either as a part of routine screening test in obese children or for evaluation of other diseases. Children remain asymptomatic and present clinically once the liver disease has progressed or with concurrent extrahepatic manifestations of MetS. The mean age of diagnosis of NAFLD in children is reported to be between 11 and 13 years. Clinical manifestations of NAFLD include nonspecific right upper quadrant abdominal pain from stretching of liver capsule (approximately 42%–59% of the patients), fatigue, and irritability. Physical examination may reveal acanthosis nigricans from insulin resistance (IR); hepatomegaly in up to 50% of the patients, which might be difficult to assess because of abdominal obesity; and, rarely, splenomegaly.
Diagnostic Methods
Liver enzymes
In spite of the high prevalence of NAFLD in children, screening and diagnostic approaches in pediatric NAFLD are not well defined. The American Academy of Pediatrics recommends biannual screening of children 10 years of age or older who are overweight with other risk factors for NAFLD or obese even without risk factors with alanine aminotransferase (ALT) and aspartate aminotransferase (AST) levels and further referral to pediatric hepatologist if ALT or AST levels are 2 times the upper limit of normal levels. However, the European Society for Pediatric Gastroenterology Hepatology and Nutrition recommends screening in obese children 3 years of age or older with both liver enzymes and ultrasound. Analysis of data from the National Health and Nutrition Examination Survey between 1999 and 2006 in the SAFETY study showed that the 95th percentiles for ALT in healthy weight, metabolically normal, and liver disease–free children were 26 U/L in boys and 22 U/L in girls in comparison with the median upper limit of normal of 53 U/L (range 30–90 U/L) used at different children’s hospitals in the United States. Hence, lower cutoff of ALT to screen for NAFLD should be used to improve its sensitivity.
Imaging
Ultrasound is a widely used screening tool for hepatic steatosis with a sensitivity of approximately 80% and specificity of approximately 50% to 60%. However, ultrasound has decreased sensitivity in patients with mild steatosis. Moreover, ultrasound cannot accurately distinguish between simple steatosis and NASH or fibrosis. Newer imaging techniques, such as controlled attenuation parameter and MRI with proton density fat fraction, are shown to be more accurate in assessing hepatic steatosis. Imaging techniques that measure liver stiffness using elastography to assess hepatic fibrosis have been developed recently. Although these recent imaging techniques are more accurate than conventional ultrasound, their use is currently limited because of cost and the lack of validated cutoff values in children.
Liver biopsy
Liver biopsy remains the gold standard in the evaluation of steatosis, NASH, and NAFLD-related liver fibrosis. Simple steatosis is defined as macrovesicular steatosis in ≥5% of the hepatocytes after excluding other causes of hepatic steatosis, such as viral hepatitis, Wilson disease, or autoimmune hepatitis. NASH is characterized by hepatocyte injury (ballooning) and neutrophilic infiltration of the liver (lobular and portal inflammation). In a retrospective analysis of children with biopsy-proven NAFLD, 2 distinctive patterns of histology were identified. Steatosis, ballooning degeneration, lobular inflammation, and perisinusoidal fibrosis were categorized as type 1 (adult type) NASH, whereas steatosis, portal inflammation, and portal fibrosis were categorized as type 2 (pediatric type) NASH. Type 2 NASH was found to be the most common histologic pattern seen in younger children with NAFLD.
Progression of Liver Disease
Limited data exist on pediatric NAFLD progression from simple steatosis to NASH, to fibrosis and cirrhosis. The presence of advanced liver fibrosis is shown to be a predictor of overall and liver-related mortality irrespective of other histologic features. The prevalence of advanced liver fibrosis in children with NAFLD is variable. In a study by Alkhouri and colleagues, only 15% of 67 children with biopsy-proven NAFLD were found to have significant fibrosis (stage 2–3). In a retrospective review of liver histology from 742 children who had autopsy for sudden expected death, NASH was observed in approximately 23% of the children with fatty liver of which only 9% of them had bridging fibrosis or cirrhosis. In a multicenter retrospective cohort study including 108 children with biopsy-proven NAFLD, stage 3 fibrosis was observed in approximately 20% of the children at the time of presentation. In another multicenter study involving 92 children with biopsy-proven NAFLD, approximately 24% of them had stage 3 fibrosis. Therefore, approximately 10% to 25% of children diagnosed with NAFLD can progress to advanced fibrosis.
Long-term follow-up studies to assess liver and overall outcomes in children with NAFLD are lacking. A retrospective longitudinal follow-up of 66 children with NAFLD over 20 years demonstrated a standardized mortality ratio of 13.6 of whom 3% of them needed liver transplantation (LT). The observed LT-free survival was significantly lower than expected survival of the US population of same age and gender. In a data analysis from United Network for Organ Sharing database of 330 children and young adults who underwent LT for NASH cirrhosis between 1987 and 2012, 14 patients had LT when younger than 18 years, 20 had LT between 18 and 25 years of age, and 13 needed re-transplantation due to NASH recurrence. Therefore, it is very clear that pediatric NAFLD can progress to end-stage liver disease requiring LT in childhood and young adults.
Multiple adult studies have shown that NAFLD is a risk factor for the development of hepatocellular carcinoma (HCC) even in the absence of cirrhosis. One of the follow-up studies involving adults with cirrhosis showed that the yearly cumulative incidence of HCC in patients with NASH cirrhosis was 2.6%. HCC has been reported in a pediatric patient in the setting of obesity and steatosis without evidence of fibrosis or cirrhosis. Pediatric NAFLD might lead to increased risk of HCC in adulthood, but this association has not been studied. Development of HCC in the absence of cirrhosis or fibrosis might indicate the potential role of other factors, such as metabolic syndrome, obesity, IR, or oxidative stress in the pathogenesis of HCC in patients with NAFLD.
Extrahepatic complications
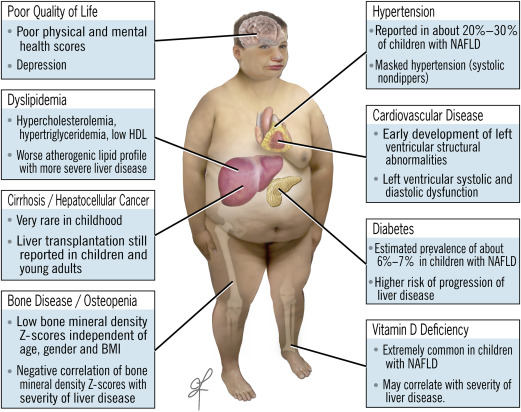
Mechanisms involved in the development of extrahepatic complications in children with NAFLD are not completely understood. It is hypothesized to be caused by an interplay of many factors such as proinflammatory mediators, oxidative stress, IR, and lipotoxicity. Different studies evaluating different extrahepatic complications ( Fig. 1 ) of pediatric NAFLD are outlined in Table 1 .
| References | Study Population | Diagnosis of NAFLD | Variable of Interest | Results |
|---|---|---|---|---|
| Cardiovascular diseases | ||||
| Schwimmer et al, 2008 | Obese children with (n = 150) and without NAFLD (n = 150) | Liver biopsy | Dyslipidemia Impaired fasting glucose Hypertension | Children with NAFLD had significantly higher TC, LDL-C, TG, fasting glucose and blood pressures than those without NAFLD. |
| Nobili et al, 2010 | Children with NAFLD (n = 18) | Liver biopsy | Atherogenic lipid profile | NAFLD activity and fibrosis scores had a significant positive correlation with TG/HDL-C, TC/HDL-C, and LDL-C/HDL-C ratios even after the adjustment for BMI, insulin resistance, impaired glucose intolerance and MetS. |
| Corey et al, 2015 | Children with NAFLD in TONIC trial (n = 173). Children with and without histologic improvement are compared | Liver biopsy | Dyslipidemia | Children with histologic improvement had significant decreases in TC, LDL-C and non-HDL-C compared with children with no histologic improvement. |
| Pacifico et al, 2008 | Obese children with (n = 29) and without NAFLD (n = 33) and lean subjects (n = 30) | Liver ultrasound | CIMT | CIMT was significantly higher in obese children with NAFLD compared to age-matched and sex-matched obese children without NAFLD and healthy controls. There was also a significant association between higher CIMT and severity of hepatic steatosis. |
| Demircioğlu et al, 2008 |
| Liver ultrasound | CIMT | CIMT was significantly higher in obese children with NAFLD and correlated with grades of steatosis. |
| Manco et al, 2010 |
| Liver biopsy | CIMT | There was no significant association between CIMT and NAFLD or grades of steatosis. |
| Schwimmer et al, 2014 | Children with NAFLD (n = 484) from NASH CRN Children assessed both at enrollment and 48 wk afterward | Liver biopsy | Hypertension | Prevalence of hypertension was approximately 36% at baseline and 21% at 48-wk follow-up. Children with hypertension had more severe grades of steatosis than children without hypertension. Girls with NAFLD had higher risk of having persistent hypertension at 48-wk follow-up. |
| Giordanno et al, 2014 | Children with NAFLD (n = 101) | Liver biopsy | Systolic and diastolic dipping by ambulatory blood pressure monitoring | Systolic nondippers had significantly impaired oral glucose tolerance and higher insulin resistance compared with systolic dippers. |
| Sert et al, 2012 | Obese adolescents with and without NAFLD (n = 80) Lean subjects (n = 37) | Liver ultrasound and ALT | Left ventricular mass | Significantly higher left ventricular mass with impaired diastolic function in obese children with NAFLD compared with obese children with no NAFLD and lean subjects. |
| Pacifico et al, 2014 | Obese children with (n = 54) and without (n = 54) NAFLD. Lean healthy subjects (n = 18) | MRI | Left ventricular function | Obese children with NASH had more severe left ventricular systolic and diastolic dysfunction compared with obese children with simple steatosis and obese children with no NAFLD. |
| Fintini et al, 2014 | Children with NAFLD (n = 50) | Liver biopsy | Cardiac function and geometry | Left ventricular hypertrophy, concentric remodeling and left atrial dilatation were seen in 50 children with biopsy-proven NAFLD. Significantly lower cardiac alterations in children with simple steatosis compared with those with NASH. |
| Type 2 DM and abnormal glucose metabolism | ||||
| Manco et al, 2008 | Children with NAFLD (n = 120) | Liver biopsy | MetS | Prevalence of type 2 DM was approximately 2% in children with NAFLD. Significant association was found between histologic severity and component of MetS. |
| Schwimmer et al, 2003 | Children with NAFLD (n = 43) | Liver biopsy | Insulin resistance Type 2 DM | Insulin resistance was present in 95% of subjects and prevalence of type 2 DM was found to be 14%. |
| Carter-Kent et al, 2009 | Children with NAFLD (n = 130) | Liver biopsy | Type 2 DM | Prevalence of type 2 DM was approximately 7% in children with NAFLD. |
| Xanthakos et al, 2015 | Adolescents undergoing bariatric surgery (n = 148) | Liver biopsy | Type 2 DM | Prevalence of type 2 DM was found to be approximately 14% and diabetes was found to be the only significant predictor of presence of liver fibrosis. |
| Newton et al, 2016 | Children with NAFLD (n = 675) | Liver biopsy | Prediabetes Type 2 DM | Prevalence of prediabetes and diabetes were 23.4% and 6.5%, respectively. Girls with NAFLD had higher risk of developing prediabetes and type 2 DM than boys with NAFLD. Children with prediabetes and diabetes had significantly higher odds for developing NASH. |
| Vitamin D deficiency | ||||
| Nobili et al, 2014 | Children with NAFLD (n = 73) | Liver biopsy | Vitamin D deficiency | Children with NASH had significantly lower vitamin D levels than those without NASH. Low vitamin D levels also correlated with the severity of liver fibrosis. |
| Hourigan et al, 2015 | Children with NAFLD (n = 102) | Liver biopsy | Vitamin D deficiency | Prevalence of vitamin D deficiency and insufficiency was high in patients with NAFLD. There was no relationship between vitamin D levels and histologic severity of NAFLD. |
| Osteopenia and osteoporosis | ||||
| Pirgon et al, 2011 | Obese children with or without NAFLD (n = 82) Lean controls (n = 30) | Liver ultrasound | BMD | Children with hepatic steatosis on ultrasound had lower spine BMD Z-scores compared with children with no hepatic steatosis. |
| Pardee et al, 2012 | Obese children with (n = 38) and without (n = 38) NAFLD Age, gender, weight, and height matched | Liver biopsy | BMD | BMD Z-scores are significantly lower in obese children with NAFLD compared with those without NAFLD. Children with NASH had lower BMD Z-scores than those without NASH. |
| Pacifico et al, 2013 | Obese children with (n = 44) and without (n = 44) NAFLD Age, gender, pubertal stage and BMI matched | MRI Liver biopsy in a subset of NAFLD patients | BMD | Obese children with NAFLD had lower BMD Z-scores than those without NAFLD. Children with NASH had lower BMD than those without NASH. |
| OSA | ||||
| Sundaram et al, 2014 | Obese children with NAFLD (n = 25) | Liver biopsy | OSA | Prevalence of OSA was approximately 60%. OSA is associated with severe hepatic fibrosis. |
| Nobili et al, 2014 | Obese children with NAFLD (n = 65) | Liver biopsy | OSA | Approximately 60% of the children with NAFLD had OSA. OSA was associated with presence of NASH and fibrosis. |
| QOL | ||||
| Kistler et al, 2010 | Obese children with NAFLD (n = 240) Healthy controls (n = 5480) | Liver biopsy | QOL | 39% of children with biopsy-proven NAFLD had impaired QOL scores. Children with NAFLD had worse total, physical, and psychosocial scores compared with healthy children. |
| Kerkar et al, 2013 | Children with NAFLD (n = 48) Obese controls without NAFLD (n = 40) | At least 3 of the following: BMI >97th percentile ALT >50 IU/L, positive liver ultrasound Liver biopsy | QOL | Children with NAFLD had higher levels of depression compared with obese controls without NAFLD. |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


