Fig. 1
27 Month female seen acutely for fracture of her right humerus after a reported fall to the ground. Because of a suspicious injury mechanism and social situation a skeletal survey was performed. There was evidence of healing scapula fracture indicating previous non accidental trauma
Appendicular skeleton |
Humeri (AP) |
Forearms (AP) |
Hands (PA) |
Femurs (AP) |
Lower legs (AP) |
Feet (AP) |
Axial Skelton |
Thorax (AP, lateral, right and left obliques), to include ribs, thoracic and upper lumbar spine |
Pelvis (AP), to include the mid lumbar spine |
Lumbosacral spine (lateral) |
Cervical spine (lateral) |
Skull (frontal and lateral) |
Follow-Up Survey and Other Studies
A follow-up skeletal survey at 2 weeks increases the yield, with 21.5 % of subjects having new information noted on the follow-up skeletal survey (Fig. 2). Therefore, follow-up skeletal surveys have become customary in child abuse protocols (Harper et al. 2013). A 15-view limited follow-up survey found new information in 38 % of studies, with less radiation and without missing clinically significant new fractures (Harlan et al. 2009). Because of the high morbidity and mortality risk of missing child abuse, the follow-up skeletal survey should be routinely performed (Singh et al. 2012). Obtaining skeletal surveys on siblings of abused children has also been suggested. Although radiation exposure is a risk associated with obtaining a skeletal survey, there are no studies that specifically describe the actual risks from radiation exposure to children receiving a skeletal survey (Karmazyn et al. 2011). Radionuclide bone scans, which cost 6 times more than a skeletal survey, have been used more as a supplement to the radiographic skeletal survey, rather than as the primary imaging modality (Mandelstam et al. 2003). Magnetic resonance imaging (MRI) or ultrasound examinations may be used to supplement the skeletal survey in cases of suspected physeal or soft tissue injury. CT scans are used to evaluate for abdominal injury or abusive head trauma. MRI provides full assessment of the intracranial pathology in child abuse in order to detect asymptomatic, nonacute parenchymal brain lesions. Diffusion- and susceptibility-weighted imaging is very reliable for diagnosing hypoxic-ischemic brain injury and parenchymal hemorrhage (Parizel et al. 2003). MRI can also detect related spinal cord pathology in the child with AHT, such as ligamentous injury and intraspinal injuries such as spinal cord injury without radiographic abnormality or proximal brachial plexus injuries, especially at the root level.
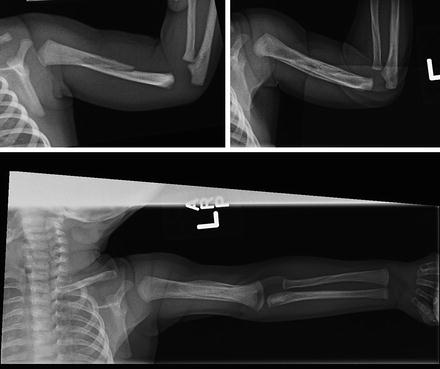
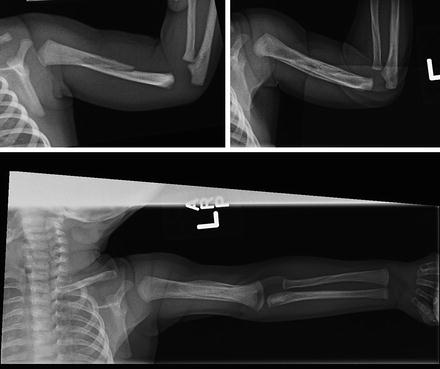
Fig. 2
Two month infant not using left upper extremity. No specific injury mechanism could be elicited from parents. Initial AP radiograph of the left humerus did not show a fracture (figure 1a). A skeletal survey was completed and the lateral image showed a left humerus midshaft fracture (figure 1b). A repeat skeletal survey two weeks later showed the healing fracture (figures 2c,d). Eye exam and head CT were normal
Variations in Skeletal Survey Screening
A skeletal survey is useful to screen for occult fractures in children suspected to be at high risk for abuse. However, there are marked variations in the use of the survey across children’s hospitals. The controversy is in the interpretation of the AAP guidelines, what the physician determines to be a “suspected” case, the physician experience level, the standard of care for the institution, and the availability of child abuse specialists and programs. In a survey of 40 children’s hospitals, screening was performed for 83 % of children under the age of 2 years who were diagnosed with physical abuse (Wood et al. 2012). The likelihood of screening varied from 55 % to 93 % and was higher for those hospitals with a child abuse program. In particular, the use of a skeletal survey for children with traumatic brain injury varied from 38 % to 88 % (mean 68 %) and for infants with a femur fracture from 41 % to 94 % (mean 77 %). This variation in the interpretation and use of the skeletal survey has led to a multidiscipline expert panel RAND/UCLA appropriateness method development of recommendations for obtaining a skeletal survey in young children less than 2 years of age, presenting with fractures (Wood et al. 2014).
Usefulness of the Skeletal Survey
A skeletal survey is very useful for detecting occult fractures in infants less than 6 months of age (Duffy and Squires 2011). Children with abusive head trauma had a higher chance of an occult fracture compared to other types of abuse injuries (Day et al. 2006; Duffy and Squires 2011). For children with isolated skull fractures but no abusive head trauma, the skeletal survey found additional fractures in only 6 %, typically in premobile infants under 6 months of age (Laskey et al. 2013). The older child with a simple linear skull fracture is less likely to have a positive skeletal survey. Laskey et al. found that the majority of long falls had only a simple skull fracture with a negative skeletal survey (Laskey et al. 2013).
Summary of Recommendations for Skeletal Survey
The skeletal survey should be thought of as a supplement to the history and physical examination in the infant and young child under the age of 2 years who cannot otherwise give a history or cooperate in a physical examination. A skeletal survey is recommended for all infants under 1 year of age with a fracture, unless the fracture is clearly in a mobile infant who is cruising and could accidentally sustain a fracture such as a distal radius and ulna fracture or a toddler tibia or fibula fracture and a simple skull fracture in an infant older than 6 months of age from a plausible mechanism or a plausible birth fracture such as the clavicle. For children 12–24 months of age, a skeletal survey is necessary if there is a history of abuse or domestic violence, there is a delay in seeking care for a painful injury, the history is not consistent or plausible for the fracture, the fracture was reportedly from a non-plausible mechanism such as being hit by a toy, or there are suspicious soft tissue injuries. For any child under the age of 2 years, all rib fractures, classic metaphyseal lesions, complex skull fractures, humeral fractures with physeal separation, or femoral diaphyseal fracture should receive a skeletal survey as part of their evaluation (Wood et al. 2014).
Dating Fractures
New periosteal bone is a classic finding of a healing fracture on a skeletal survey (Table 2). The follow-up skeletal survey at 2 weeks can give more precise information about dating of the fracture (Section on Radiology AAP 2009). Dating of a fracture remains an imprecise endeavor. A recent review of 82 accidental long bone fractures in 63 children younger than 72 months of age showed that the fracture could be dated as acute if less than 1 week from the fracture, recent if 8–35 days, or old if >36 days (Prosser et al. 2012). Soft tissue swelling, periosteal reaction, soft callus, hard callus, bridging, and remodeling were six key features that allowed dating (Table 2).
Peak times of appearance of radiographic features | Days |
|---|---|
Resolution of soft tissue change | 4–10 |
Earliest appearance of periosteal new bone formation | 10–14 |
Loss of fracture line definition | 14–21 |
Soft callus | 14–21 |
Hard callus | 21–42 |
Remodeling | 1 year |
Fractures in Abuse
Although any aged child can sustain an injury from abuse, it is the child under age 2 years without the verbal skills to tell their story, who is the most vulnerable to repeat abusive episodes. Up to 9,000 infants and children under 2 years of age are hospitalized in the USA with a fracture (Leventhal and Martin 2010). Approximately 20 % of these fracture cases are caused by abuse, although the numbers are likely much higher due to underrecognition and underreporting (Ravichandiran et al. 2010).
Hobbs described six important patterns of fracture from physical abuse (Table 3) (Hobbs 1989). However, no fracture pattern or location is pathognomonic of child abuse. Several fractures such as metaphyseal corner fractures (classic metaphyseal lesion) (Fig. 3), posterior rib fractures, and fractures in various healing stages are so commonly seen in non-accidental trauma that a high suspicion for abuse is always warranted for these fracture patterns (Baldwin and Scherl 2013). Prediction of abuse is often compounded by methodology, small retrospective series, a wide variation in ages of children, inclusion of all types of fractures, and when the mechanism of motor vehicle accident (MVA) is included in the analysis. Although there may be an association with abuse for a certain type of fracture, that association does not prove that the injury was caused by abuse. For most studies that show this association for a particular fracture type, the association is usually less than 50 %. For fractures in general, features such as young age, Medicaid insurance, nonwhite race, male sex, and presence of additional injuries such as traumatic brain injury had associations with abuse (Leventhal and Thomas 1993; Leventhal and Martin 2010; Lane and Rubin 2002; Skellern and Wood 2000). For an active child who is capable of rough housing on furniture, the rate of suspected abuse was only 5.5 % (Hennrikus and Shaw 2003).

A single fracture with multiple bruises |
Multiple fractures in different stages of healing, possibly with no bruises or soft tissue injuries |
Metaphyseal-epiphyseal injuries |
Rib fractures |
New periosteal bone |
Skull fracture in association with intracranial injury |

Fig. 3
Three month old female infant seen in emergency department with a midshaft femur fracture. A routine skeletal survey showed multiple fractures including a classic metaphyseal lesion of the distal radius (block arrow). This is also termed “corner fracture”
Age seems to be one of the strongest predictors of abusive fractures. For children under age 3 years who present with any type of fracture from any mechanism, the probability of abuse ranges from 10.8 % to 22.4 % (Leventhal et al. 2007, 2008; Leventhal and Martin 2010). For isolated long bone fractures in children less than 3 years of age, only 1 % of these fractures were diagnosed by the treating physician to be from child abuse (Taitz and Moran 2004). For younger-aged children, the probability for abuse dramatically increases. In infants (<1 year of age) with any type of fracture, 26.3 % were reported to child protective services (CPS), with abuse being confirmed in 15.2 % of the total study group (Skellern and Wood 2000). Leventhal found an even higher risk (37.5 %) of abuse in infants (Leventhal and Thomas 1993). Other studies have found age <4 months (Skellern and Wood 2000) and age <24 months (Leventhal et al. 2008; Leventhal and Martin 2010) to be associated with an increased risk of abuse. As a general principle, because of the higher association of abuse with age under 1 year and the difficulty in performing a reliable physical examination on an infant in pain, one cannot be faulted for obtaining a skeletal survey on an infant who presents with a fracture even if the suspicion for child abuse is low. Although fractures in infants are highly associated with abuse, this association is typically less than 50 %. While important to be mindful and even suspicious about abuse in an infant, it is equally important to not be judgmental.
Rib Fractures
Rib fractures are rarely from accidental trauma. They can be very difficult to detect, despite often being multiple. They occur posteriorly by a mechanism of anterior compression on the thoracic cage that levers the posterior aspect of the rib against the transverse process of the spine (Hobbs 1989). First rib fractures that have been reported in case series and case reports in infants have almost always been attributed to abuse (Melville et al. 2012). Lower rib fractures are typically posterior at the costovertebral articulation and are caused by lateral gripping of the infant with anterior posterior chest compression (Tsai et al. 2012). Rib fractures can be very difficult to visualize on routine chest radiographs and are detected by careful radiographic study and skeletal survey (Hobbs 1989). Cardiopulmonary resuscitation does not typically cause rib fracture in the young child. Since rib fractures are so rare in accidental trauma under 2 years of age, all rib fractures in this age group should receive a full skeletal survey with follow-up survey. Kleinman reported sternum fractures to be specific for abuse (Kleinman 1998).
Classic Metaphyseal Lesion
Metaphyseal fractures adjacent to the physis are classic for physical abuse in the young child (Fig. 3) (Hobbs 1989). The classic corner fracture, termed the classic metaphysical lesion (CML), is a result of acceleration and deceleration of the infant with resulting torsion and distraction to the end of the bone. This pulling and twisting of the metaphysis disrupts this weaker newly formed trabecular bone near the physeal cartilage, resulting in the appearance of a corner fracture (Hobbs 1989). Common areas for the CML include the distal radius and ulna, elbow, knee, and ankle. Kleinman et al. in autopsy studies of abused infants reported that bucket handle and corner fractures are full-thickness metaphyseal fractures that extend through the primary spongiosa of the bone, just proximal to the zone of provisional calcification (Kleinman and Marks 1995). Near the center of the physis, the amount of metaphyseal bone is thin but is much thicker at the periphery, resulting in a “bucket handle” radiographic appearance. Although often present in several locations, the presence of one CML lesion on skeletal survey is highly suspicious and specific for child abuse (Kleinman et al. 2011). Fracture callous does not always appear early in a CML, so dating the occurrence of the fracture by skeletal survey is not reliable.
Other Related Injuries
Brachial plexus injuries caused by abuse have been reported in young children (McMillan et al. 2010). Spine fractures may be the only indication of skeletal trauma and has an association with intracranial injury (Barber et al. 2013). Likewise, a child with a cervical spine fracture may initially present with a defect in the upper or lower extremity. When abuse is the cause of a spine injury, it is commonly associated with spinal cord injury without obvious radiographic abnormalities (SCIWORA). The skeletal survey should always include a lateral of the cervical, thoracic, and lumbar spines, since CT scan may also show a fracture. However, if clinical or radiographic evaluation suggests a spine fracture, further imaging with MRI should be obtained. If a child has AHT and an MRI is being done to further evaluate the brain, the MRI should include the entire spine (Kemp et al. 2010).
Upper Extremity Injuries in Abuse
Upper extremity fractures have been associated with abuse, typically in younger children. Fractures from abuse may be in unusual locations such as the distal clavicle, acromial tip, scapula, proximal humeral metaphysis, or distal humeral physis (Fig. 4). The mechanism of fracture is from violent blows or traction injuries and is suggestive of abuse in young children.


Fig. 4
Six week old infant was taken to emergency room by his mother after a reported fall. He was noted to have limited spontaneous use of left upper extremity. Radiograph showed an acromion fracture (arrow). Further evaluation of family situation revealed that the boyfriend had been babysitting alone and tried to “quiet him” when he was crying
Clavicle Fractures
Clavicle fractures are the most common birth fractures and are related to a large infant, dystocia, or a difficult delivery. Infants may normally have a separate ossification center at the tip of the acromion that resembles a fracture, so this must be distinguished from the sharp demarcated edges with callous seen in a healing fracture (Fig. 4). The older the child, the more likely a clavicle fracture is caused by an accidental injury. The probability of abuse in a child less than 3 years of age varied from 5.9 % to 20.7 % (Leventhal et al. 2007, 2008) but was 28.1 % in children less than 12 months of age (Leventhal et al. 2008). In an infant under 10 days of age with a history consistent with a birth injury, a skeletal survey is not indicated. For the 11–21-day-old infant with possible birth injury, the need for a skeletal survey is less clear. After 21 days of age, a fresh clavicle fracture requires a skeletal survey. For children from 12 to 23 months of age with a history of a fall, the skeletal survey should be performed if there is suspicion from the history or a non-plausible mechanism. If a child 1 month to 2 years of age presents with a healing fracture noted unexpectedly on a routine chest radiograph, a skeletal survey should be done.
Humerus Fractures
The probability of abuse in children less than age 3 years with a humerus fracture of any type from any etiology ranges from 9.3 % (Kowal-Vern et al. 1992) to 18 % (Shaw et al. 1997) to 50 % (Leventhal et al. 2008). The probability for abuse in the child who presents with a diaphyseal humerus fracture depends on whether the case was reviewed by Child Protection Services, in which 8.8 % were determined to be abuse related, or based on physician evaluation in which 17.6 % were abuse (Shaw et al. 1997). An age under 12–18 months is associated with an increased probability that the fracture will be from abuse (Thomas and Rosenfield 1991; Strait and Siegel 1995; Leventhal et al. 2008; Pandya and Baldwn 2010). However, in these same studies, a supracondylar humerus fracture was associated with a lesser probability of being caused by child abuse. Other features, including more proximal fractures, diaphyseal fractures, evidence of prior trauma, suspicious history, or spiral or oblique fractures, were associated with abuse (Pandya and Baldwn 2010). For a spiral fracture of the humerus, the plausible mechanism, the history of other injuries, and the skeletal survey are key to determining if this is abuse related (Hobbs 1989).
The distal humerus epiphyseal fracture is highly associated with child abuse. An infant may present with a swollen elbow of unknown cause or with a story that is not plausible. If this is an acute or recent injury, the infant or young child may be in much pain, and the elbow may be warm and tender. If the injury has been present for more than 10–14 days, it may be less painful or pain-free and have swelling related to the palpable healing fracture, which by then should be visible on a radiograph. The injury may be confused with infection or if displaced, an elbow dislocation. Radiographs may simply only show soft tissue swelling. If displaced, the proximal radius and ulna are not in line with the humerus. A skeletal survey should be done in an infant with a swollen elbow that is not an infection or in an infant with any fracture of the humerus. Ultrasound may show the nature of the displaced epiphysis from the shaft of the humerus. Follow-up skeletal survey may show the subperiosteal reaction at 10–14 days, typical for a healing fracture.
Forearm Fractures
Radius and ulna fractures are associated with abuse particularly in children less than 1 year of age (Leventhal et al. 2008). When looking at < 3-year-old children, abuse is considerably less likely, ranging from 7.5 % to 30 %, depending on the study population (Leventhal et al. 2007, 2008). The skeletal survey was noted to have a sensitivity of 75 % (CI 34.9–96.8) to detect a radius fracture and 50 % (CI 15.7–84.3) to detect an ulna fracture (Mandelstam et al. 2003). The distal radius contributes 80 % of the growth of the radius, so metabolic conditions such as vitamin D deficiency are frequently apparent early in this location. Olecranon fractures are a common feature of OI, and this diagnosis should be considered, especially if bilateral. A distal radius or ulna buckle fracture from a fall onto an outstretched hand in a child who cruises or walks does not require a skeletal survey if there is no other suspicion for abuse (Wood et al. 2014).
Hand Fractures
In older children, hand fractures are extremely common but are suspicious for abuse in infants. In infants younger than 10 months of age, fractures are typically torus fractures of the metacarpals or the proximal phalanges of the hand, as well as of the feet (Nimkin et al. 1997). Skeletal survey, particularly the oblique view, is necessary to detect these fractures, as clinical signs are unusual.
Differential Diagnosis
While it is essential not to miss child abuse as the underlying cause of a child’s injuries, it is just as important to remain objective, be open to alternative explanations, and make an accurate diagnosis. Inappropriately diagnosing child abuse is harmful to the child and family, risks the parents losing custody, and is a misuse of resources (Schwend et al. 2000). Be wary of false allegations, especially when there are custody and visitation disputes or if the charges are coming from the parent (Bernet 1993). Alternative diagnoses are also brought up in custodial and criminal cases, so diagnostic accuracy during the initial evaluation is essential.
Injury to a developing bone of an infant leads to subperiosteal hemorrhage, leading to subperiosteal healing bone by 10–14 days (Hobbs 1989). There is a normal physiologic diaphyseal reaction that is frequently present in infants younger than 6 months of age and is symmetric and diaphyseal only on the long bones of the extremities (Pergolizzi and Oestreich 1995). Initial radiographs can be normal, with a skeletal survey and follow-up survey being most important. Besides trauma and infection, other conditions such as Caffey’s disease (infantile cortical hyperostosis), vitamin C deficiency, vitamin D deficiency, metastatic neuroblastoma, Langerhans histiocytosis, vitamin A intoxication, leukemia, and various drugs are more rare causes of subperiosteal bone formation than child abuse (Hobbs 1989). Other causes of fracture include osteogenesis imperfecta, rickets of prematurity, disuse osteoporosis, copper deficiency, and osteomyelitis (Hobbs 1989). Congenital syphilis is rare but is increasing in prevalence. Congenital syphilis readily mimics the fractures of child abuse with diaphysitis, metaphysitis, and pathologic fractures in various stages of healing, mimicking child abuse (Lim et al. 1995). If the skeleton otherwise looks normal radiographically, this strongly excludes general conditions of genetic, metabolic, or bone disease (Hobbs 1989).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


