NICU
Naureen Memon
Miranda Bik-Yin Ip
Phuoc V. Le
Joseph H. Chou
Delivery Room Management
Intrapartum Fetal Heart Rate Monitoring
Baseline fetal HR: Normal HR is 110–160 bpm.
Fetal tachycardia: HR >160 bpm. Causes: Maternal or fetal fever/infxn, fetal hypoxia, thyrotoxicosis, maternal meds (β-agonists and parasympathetic blockers)
Fetal bradycardia: HR <110 bpm, w/ severe bradycardia <90 bpm. Causes: Hypoxia, complete heart block, maternal meds (β-blockers)
Variability: Absence of beat-to-beat variability may indicate: Severe hypoxia, anencephaly, complete heart block, maternal med effect (narcotics, MgSO4)
Accelerations: Are associated with fetal movement and indicate fetal well-being
Decelerations:
Early: Assoc w/ uterine compression of fetal head. Benign; not assoc w/ fetal compromise
Variable: Assoc w/ umbilical cord compression. Can cause perinatal depression, but if beat-to-beat variability is maintained, then fetus is not compromised
Late: Assoc w/ uteroplacental insuff. If beat-to-beat variability maintained, fetus usually well compensated. If not, then may represent significant fetal hypoxia
APGAR Scoring
| 0 | 1 | 2 | |
|---|---|---|---|
| Heart rate | Absent | <100 min | >100 min |
| Respiratory effort | Absent | Weak cry; hypoventilation | Good, crying |
| Muscle tone | Flaccid | Some flexion | Active motion |
| Reflex irritability | No response | Grimace | Cry or active withdrawal |
| Color | Blue or pale | Acrocyanotic | Completely pink |
Gestational Age and Birth Weight Classifications
| Maturity by Gestational Age | ||
|---|---|---|
| Preterm: <37 wk | Term: 37–42 wk | Postterm: >42 wk |
| Birth weight | ||
| Low birth weight (LBW) : <2500 g | ||
| Very low birth weight (VLBW): <1500 g | ||
| Extremely low birth weight (ELBW): <1000 g | ||
| Birth Weight/length for Gestational Age | ||
| Small for gestational age (SGA): Weight or length <2 SD | ||
| Appropriate for gestational age: Weight or length within 2 SD | ||
| Large for gestational age: Weight or length >2 SD | ||
| Asymmetric IUGR (delayed fetal weight gain with sparing of length and head growth) acute malnutrition or placental insufficiency; has potential for catch-up growth | ||
| Symmetric IUGR (delayed fetal weight gain w/ comparable delays of length and head growth) prolonged malnutrition, genetic processes, or congenital anomalies; has less potential for catch-up growth | ||
| (Pediatr Rev 2006;27:224) | ||
Be sure to plot length, weight, and head circumference on every infant!
New Ballard score to assess neuromuscular and physical maturity of infants, especially in those that are premature or if dates are unknown
Can be obtained online at www.ballardscore.com
For preterm growth charts, go to www.medcalc.com/growth
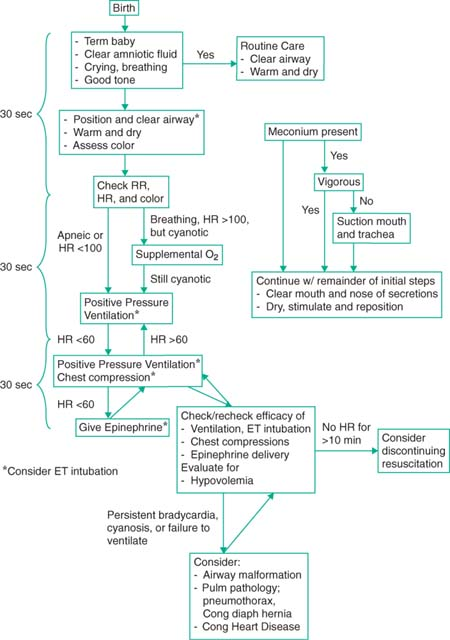
Neonatal Resuscitation
When preparing for a high-risk delivery, have an estimated weight and GA so that appropriate ETT, umbilical catheter size, and drug doses can be calculated
Suggested ETT size and depth of insertion according to weight and GA
Depth of insertion can be estimated by weight in kg + 6 cm
| Weight, g | Gestational Age, wk | Tube Size, mm (inner diameter) | Depth of Insertion from Upper Lip, cm |
|---|---|---|---|
| <1000 | <28 | 2.5 | 6.5–7 |
| 1000–2000 | 28–34 | 3.0 | 7–8 |
| 2000–3000 | 34–38 | 3.5 | 8–9 |
| >3000 | >38 | 3.5–4.0 | >9 |
| (Pediatrics 2000;106:e29) | |||
Sepsis Rule-Out Algorithms
Management of asymptomatic infants born at ≥35 wks gestation with risk factors for early-onset sepsis; protocols vary per institution.
Indications for intrapartum antibiotic prophylaxis (IAP)
+ GBS cx unless elective C-section w/o labor or ROM
GBS bacteriuria in index pregnancy
Prior baby w/ GBS disease
Maternal temp >100.4°F, even w/ negative GBS culture
GBS status unknown and ROM >18 hr, labor <37 wk or maternal temp >100.4°F
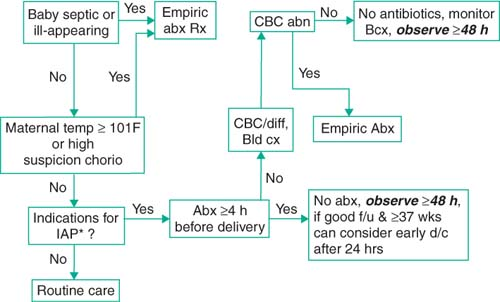 * see above text for IAP indications |
MGH guidelines: Management of asymptomatic newborn at risk for sepsis
Abnormal WBC: Total WBC <5000 or I:T ratio >0.2
I:T = number of immature PMNs/total number of PMNs
IV Abx:
Ampicillin >2 kg give 50 mg/kg/dose q8; ≤2 kg give 50 mg/kg/dose q12
Gentamicin ≥35 wk GA, give 4 mg/kg/dose q24h, <35 wk GA, give 3 mg/kg/dose q24h
Of note, maternal fever w/i 1 hr of delivery should be Rx’d as intrapartum fever
Mother w/ prior child w/ GBS dz; baby should have CBC/diff, bld cx, and Abx if IAP <4 hr or if intrapartum fever >100.4°F
The above are for management of asymptomatic infants born ≥35 wks’ gestation
Remember that these are only guidelines and do not replace clinical judgment.
Basic NICU Management
NICU Calculations and Formulas
For a number of excellent online NICU calculators go to www.nicutools.org
Vascular Access
(formulas may not be appropriate for SGA or LGA infants)
Always check placement with babygram.
Umbilical artery catheter (UAC): For arterial BP monitoring or freq ABGs
Low-line (cm) [asymptotically equal to] BW (kg) + 7 (want L3-L5, just above aortic bifurcation)
Assoc w/ more vasospasms of the lower extremities
High-line (cm) [asymptotically equal to] [3 × BW (kg)] + 9 (want T6-T10, above diaphragm)
Assoc w/ risk HTN and ↑ risk IVH, ↓ incidence of cyanosis of lower extremities
Umbilical vein catheter (UVC):
Normal: [0.5 × UA (cm)] + 1 (want above ductus venosus, at or below RA)
Low-line: Insert to point of initial blood return (for emergent use)
NICU Testing Guidelines
(Pediatrics 2006;117:572; Am Fam Physician 2007;75:1349; Arch Dis Child Fetal Neonatal Ed 2005;90:452)
| Routine Neonatal Testing Guidelines | |
|---|---|
| Test | Gestational Age |
| Cranial Ultrasound | <32 wk; d of life: 3, 10, 30, then monthly until discharge |
| Ophthalmologic exams | ≤31 wk or <1500 g or 1500–2000 g and high risk; screen at 31 wk corrected GA, but not sooner than 4 wk chronologic age |
| Hearing tests | BAERS; for all infants before discharge |
| Car seat tests | <37 wk or <2500 g or with respiratory instability |
Fluids, Electrolytes, and Nutrition
Growth parameters and expected weight gain
Weight <2 kg: Expect gain of 15–30 g/d or 10–20 g/kg/d
Weight >2 kg: Expect gain of >20 g/d
W/ preterm, may have initial weight loss of ≤15% (up to 20% in ELBW)
In term infants, may have initial weight loss of ≤10%
Fluid requirements: Premature infants have greater ECF volumes
Initial fluid requirements: 60–120 mL/kg/d
Term infants ∼60 mL/kg/d
ELBW ∼120 mL/kg/d (assuming that they are in the Giraffe incubators)
Goal after fluid stabilization: 100–150 mL/kg/d
Fluid restriction may be needed w/ PDA, BPD, CHF, renal failure, cerebral edema
Insensible loss inc w/: inc skin permeability, inc BSA:weight ratio, phototherapy, radiant warmer beds, respiratory distress syndrome, cold stress, inc activity
Insensible water loss decreases with double-walled incubators.
Monitor fluid status by daily weights, UOP, and serum Na, Hct, and BUN levels.
Fluid loss also results from vomiting, diarrhea, ostomy output, chest tube drainage
Inadequate hydration can lead to hyperosmolarity and may be a risk for IVH
Parenteral nutrition in preterm infant
Common total parenteral nutrition orders at MGH
Fluid orders on DOL #1: NPO and for…
Term infants: D10W at a rate of 60–80 cc/kg/d
Preterm: D10W at a rate of 80–100 cc/kg/d
Add electrolytes after adequate UOP & after checking serum lytes at 12–24 hr
TPN labs:
Daily: Na, K, Cl, CO2, glucose
Weekly: Above tests plus Ca, Mg, P, alkaline phosphatase, BUN, creatinine, triglyceride, total protein, albumin, bilirubin, AST, ALT, hematocrit
“Feeder-Grower” labs:
Hct and Retic: 24–28 wk GA: Weekly, >28 wk GA: Every other wk
Chem 10, alk phos:
Breast-fed <32 wk: Weekly Na, K, phos, Ca, alk phos
Formula-fed <32 wk: Weekly Ca, phos, alk phos
All breast-fed with supplement: Weekly lytes, Ca, phos
All infants on ProMod: Weekly BUN
Enteral Feeds
(Manual of Pediatric Nutrition. 4th ed)
Preterm neonates do not establish coordination of suck, swallow, and breathing until 32–34 wk GA; until then, enteral feeding via NGT (bolus vs. continuous) needed
Enteral nutrition should generally begin as soon as infant is clinically stable.
Initiation and advancement based on BW w/ attention to feeding tolerance
Most premature infants start w/ trophic feeds (low-vol; 10 mL/kg/d) to stim GI hormones, motility, and maturation and to prevent gut atrophy
Once stable, volumes increased slowly as tolerated w/ increments ∼10–20 mL/kg/d, allows for gut adaptation and minimizes risk of complications
Signs of feeding intolerance include: Inc gastric residuals >2×’s previous hr’s rate (continuous feed) or >½ previous bolus, inc in abd distention, vomiting, or bilious residuals, heme + or frank blood in stools, ↑ in apnea or bradycardia with feeds
Respiratory Syncytial Virus (RSV) Prophylaxis
(Pediatrics 2003;112:1442)
Synagis 15 mg/kg IM monthly during RSV season. 1st dose 1 mo before RSV season.
Recommended at discharge (not while in NICU) for:
<28 wk GA if born <12 mo before start of RSV season
29–32 wk GA if born <6 mo before start of RSV season
32–35 wk GA if born <6 mo before start of RSV season and w/ 2 risk factors
Infants <2 yo with chronic lung disease or congenital heart disease
Risk factors: School-aged siblings, day care, exposure to air pollutants, severe neuromuscular dz, congenital abnormalities of the airways, low birth weight (<2500 g), crowded living conditions, multiple birth, family history of asthma
Morbidity and Mortality with BW and GA
(N Engl J Med 2008;358:1700)
| Outcome | Birth Weight | ||||
| 501–760 g | 751–1000 g | 1001–1250 g | 1251–1500 g | ||
| Overall Survival | 55% | 88% | 94% | 96% | |
| Survival w/ Complications* | 65% | 43% | 22% | 11% | |
| *Complications include bronchopulmonary dysplasia, severe intraventricular hemorrhage, necrotizing enterocolitis, or bronchopulmonary dysplasia and severe intraventricular hemorrhage combined. | |||||
Pulmonary/Respiratory
Etiologies of Respiratory Distress
(NeoReviews 2005;6:e290)
| Parenchymal conditions |
| – Transient tachypnea of the newborn |
| – Meconium aspiration syndrome |
| – Respiratory distress syndrome |
| – Pneumonia |
| – Pulmonary edema |
| – Pulmonary hemorrhage |
| – Pulmonary lymphangiectasia |
| Airway abnormalities |
| – Choanal atresia/stenosis |
| – Laryngeal web |
| – Laryngotracheomalacia or bronchomalacia |
| – Subglottic stenosis |
| Developmental abnormalities |
| – Lobar emphysema |
| – Pulmonary sequestration |
| – Cystic adenomatoid malformation |
| – Congenital diaphragmatic hernia |
| – Tracheoesophageal fistula |
| – Pulmonary hypoplasia |
| Mechanical abnormalities |
| – Rib cage anomalies (e.g., Jeune syndrome) |
| – Pneumothorax |
| – Pneumomediastinum |
| – Pleural effusion |
| – Chylothorax |
Differentiating cardiac and respiratory causes of cyanosis (see Cardiology chapter)
Cyanosis w/o resp distress, O2 sat <85% on RA and 100% O2, likely dx intracardiac shunt
If O2 sat ↑ >85% on 100% O2, either intracardiac shunt vs. pulm cause of cyanosis. Need to perform a full hyperoxia test.
Hyperoxia test: Obtain baseline right radial (preductal) ABG w/ neonate on RA, then repeat ABG after providing 100% O2 for 10 min.
A Pao2 of >300 mm Hg is normal, >150 mm Hg suggests pulmonary disease, and 50–150 mm Hg suggests cardiac disease (or severe pulmonary HTN)
Respiratory Distress Syndrome (Hyaline Membrane Disease)
(Pediatrics 2008;121:419)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree