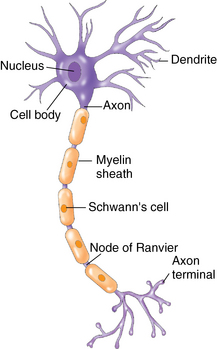
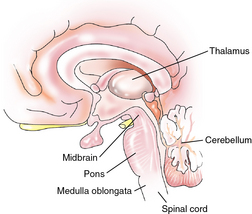
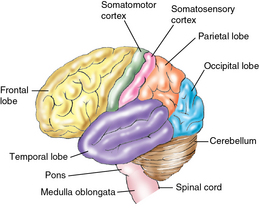
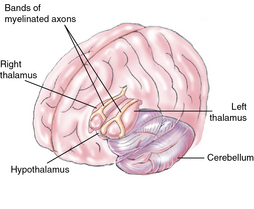
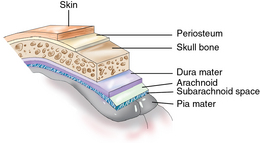
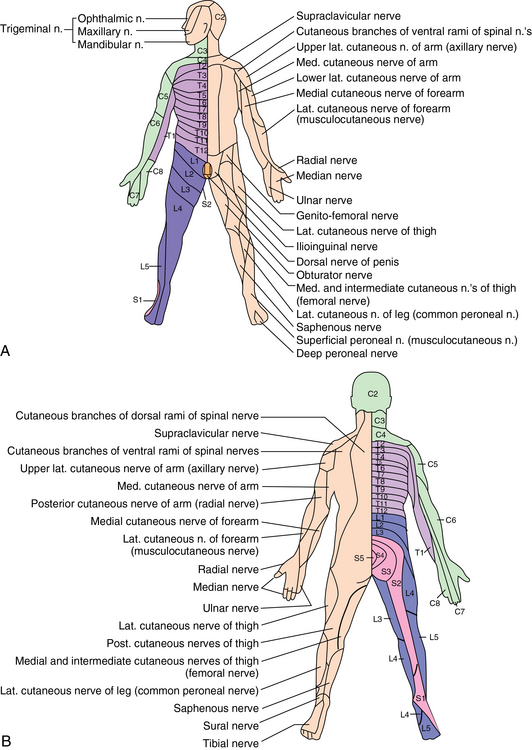
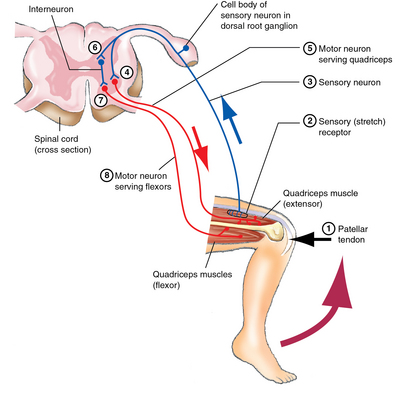
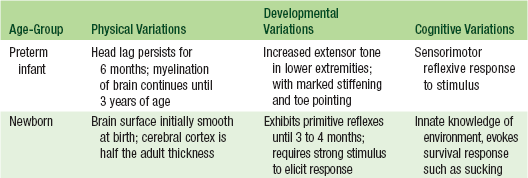
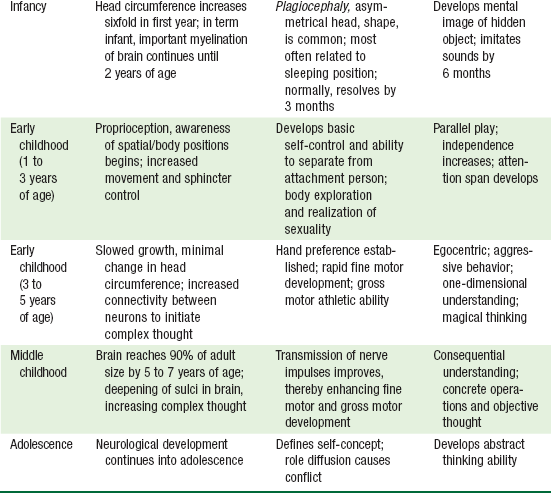
CHAPTER 19 The formation of the nervous system begins very early during the third week of embryonic life. The early integral development is essential in influencing the organization and development of the skeleton, skeletal muscles, eyes and ears, and other body systems.1 The notochord, which becomes the spinal column, develops during this period and forms the neural plate and neural folds. Closure of the neural plate is complete by the fourth week of embryonic development and the neural tube is formed. Any fetal insults that occur during this period can result in defects in the brain and spinal cord, such as spina bifida defects, which occur in 1 of 1000 live births. During the fifth week of fetal development, the anterior portion of the neural tube enlarges to form the segments of the brain. Brain growth proceeds, with the most rapid brain growth occurring between 15 and 20 weeks of gestation. By 24 weeks of gestation, the fetus has developed all of the nerve cells, or neurons, needed for the formation of the neural pathways. The neuron is the basic unit of the nervous system, and each neuron contains numerous dendrites and one axon (Figure 19-1). Dendrites are the protoplasmic branches of the cell body. Neural impulses enter the cell body through the dendrites and leave through the single axon. They then connect by a series of synapses with another dendrite of the next axon. Myelin, a lipoid material surrounding cell fibers, covers only a portion of the axons at birth. The development of intelligence in infants depends on the normal progression through the two primary developmental domains—problem solving and language.2 Brain growth is rapid after birth with 50% of postnatal brain growth achieved by 1 year of age. By 2 to 3 years of age, the brain is 80% of adult size.1 Head circumference increases sixfold in the first year of life and is the best indication of normal brain growth. Myelination, the deposit of the protective fatty substance around the axons, continues in the brain throughout the first 2 years of life, and in the preterm infant continues into the third year of life. Myelination proceeds from head to toe, cephalocaudal, beginning with the spinal cord and cranial nerves and then from midline to fingertips, proximodistal, following with the brainstem, corticospinal tracts, and sensory pathways. Preterm or very low birth weight (VLBW) infants may develop from toe to head, which is associated with persistent hypertonia in the lower extremities. The control of motor functions in infancy and early childhood is closely associated with the normal myelination of the nerve fibers.1 Completion of brain growth occurs in early adolescence. The cerebrum is the largest part of the brain and is covered by the cerebral cortex. The cerebrum is divided into two hemispheres, the left and right hemispheres, with the left hemisphere being dominant in 95% of individuals. The right hemisphere controls the functions of the left side of the body, and the left hemisphere controls the functions of the right side of the body. The hemispheres are connected by a bridge of myelinated axons, the corpus callosum, which lies between the fissures of the left and right hemispheres.1 The corpus callosum controls and integrates motor, sensory, and higher intellectual functions. The right and left hemispheres are divided into four lobes with arbitrary borders named the same as the skull bones that cover them. Each lobe controls particular bodily functions and behaviors (Figure 19-2). • Frontal lobe: Initiates movement control of the flexor muscles of hands and feet. Broca area in the frontal lobe controls the ability to articulate speech. Prefrontal area controls thought processes for anticipation and prediction of behavior, and the frontal region is involved in complex learning movement patterns and writing. Damage to the frontal region causes expressive aphasia. • Parietal lobe: Controls processing and interpretation of sensory input—visual, auditory, smell, taste, and touch sensations, including pain and temperature. Perceives where a stimulus or pressure is and on which part of the body, and provides proprioception, the sense of the position of the limbs of the body. Damage to the parietal region results in agnosia, an inability to recognize or perceive the meaningfulness of an object, persons, sounds, shapes, or smells. • Temporal lobe: Primary center for the perception and interpretation of auditory input, auditory association and perception, and memory recall. Wernicke area in the temporal lobe is related to spoken words and language comprehension. • Occipital lobe: Primary visual cortex in the brain and is the center for receiving and interpreting visual data and depth perception. The cerebellum is located in the posterior cranium and has an outer layer of gray matter overlying white matter. The cerebellum maintains the body’s equilibrium and coordinates both voluntary and involuntary movements of the limbs, trunk, head, larynx, and eyes.1 The motor cortex in the cerebrum relays signals to the cerebellum, which results in the fluid and skilled muscle movements requiring a high level of dexterity. It is the portion of the brain that processes the sensory input from the musculoskeletal system as well as from the visual, auditory, and touch receptors, and it transmits signals to the motor system to direct or correct muscle activity. Damage to the cerebellum causes ataxia (loss of coordination of motor movement, inability to perform rapid alternating movements, a wide-based gait), hypotonia, and nystagmus. In preterm infants, arrested development of the cerebellum can result in deficits in language, visual reception, and social/behavioral function. The brainstem is in the central core of the brain and includes the pons, medulla oblongata, and midbrain (Figure 19-3). The pons acts as the neural transmission center from all parts of the central cortex and supports ascending and descending nerve fibers. It controls basic breathing, eating, and motor functions. Cranial nerve V (trigeminal nerve) and cranial nerve VI (abducens nerve) arise from the pons. Damage to the peripheral pons causes a loss of sensory functions of the facial and mouth area and a loss of outward or lateral motion of the eye muscles resulting in strabismus. The medulla oblongata, which lies between the pons and the cerebellum, is a continuation of the spinal cord. The medulla processes impulses from the hypoglossal, vagal, spinal accessory, glossophyarngeal, and the vestibular and acoustic cranial nerves. It also aids in the life functions of respiration and circulation, and controls involuntary reflexes such as coughing, sneezing, and yawning. Damage to the medulla causes weakness in the shoulder muscles, affects tongue muscles and salivary function, decreases gastrointestinal motility, alters swallowing and speech functions, causes nerve deafness, and diminishes cardiovascular and respiratory functions. The diencephalon (Figure 19-4) is the extension of the brainstem and lies embedded in the cerebral cortex. It contains the thalamus, hypothalamus, pituitary gland, and the pineal gland (an endocrine gland that produces melatonin, a hormone that regulates sleep-wake cycle). Parts of the third ventricle and the nuclei of the cranial nerves also arise from the diencephalon. The midbrain contains the neural fibers that come from the spinal cord and merge into the thalamus and hypothalamus. The midbrain controls the integration of basic bodily functions. • Thalamus: Acts as the brain’s relay station and receives input from the sensory and motor systems of the body and dispatches input to the appropriate region of the cerebral cortex. • Hypothalamus: Regulates body temperature, metabolic processes, and involuntary response activity. • Pituitary gland: Responsible for hormonal control of growth, lactation, and metabolism. The brain is covered by protective layers that cushion and lubricate the outer surface (Figure 19-5). The dura mater lies just beneath the skull bone and periosteum and consists of layers of fibrous connective tissue. Adjacent to the dura mater is the arachnoid, the avascular, weblike membrane that cushions the cortex. The dura mater is separated from the arachnoid by the subdural space. The pia mater is the highly vascular area of the cortex that attaches directly to the gray matter or irregular surface of the brain. The subarachnoid area and a cushion of cerebrospinal fluid separate the arachnoid from the pia mater. There are 32 pairs of spinal nerves that innervate the upper and lower torso, extremities, skin, and muscles (Figure 19-6). The spinal nerves form complex nerve networks called plexuses. There are four major plexuses in the peripheral nervous system—the cervical, brachial, lumbar, and sacral plexuses. The body surface that is innervated by the plexus of a spinal nerve is called a dermatome. Although dermatomes map specific segments of the body surface, spinal nerve sensation can be transmitted to adjacent dermatomes (see Figure 19-6). The sensory pathways of the spinal nerves carry sensations of touch, temperature, and pain; the motor fibers activate reflexes and impulses that control skeletal muscles and the involuntary muscles of the viscera. The spinal nerves function as part of the lower motor neurons and become dysfunctional in the presence of spinal cord lesions. Reflex behavior provides the major assessment of brainstem function. A reflex is an expected response between a stimulus and an elicited motor response. The reflex arc operates outside the level of conscious control and is the basic defense mechanism of the nervous system. Reflexes help the body maintain appropriate muscle tension and react to painful or harmful stimuli. A stimulus creates an impulse that is transmitted instantaneously outward by the motor neurons of the spinal cord via the spinal nerve and peripheral nervous system to produce a brisk muscle contraction (Figure 19-7). Table 19-1 reviews the physical, developmental, and cognitive variations that occur during the development and maturation of the nervous system in infancy and childhood. The Information Gathering table reviews the pertinent areas for the neurological system for each age-group and developmental stage of childhood. Obtaining a complete history of gross motor and fine motor milestones in infancy, assessing speech and language development, and assessing learning ability is key to early identification of insults to the nervous system. Information Gathering for Neurological Assessment at Key Developmental Stages
Neurological system
Embryological development
Developmental variations
Anatomy and physiology
Central nervous system
Cerebrum
Cerebellum
Brainstem
Spinal cord
Peripheral nervous system
Spinal nerves
Spinal reflexes
Physiological variations
System-specific history
Age-Group
Questions to Ask
Preterm infant
History of hypoxia in early neonatal period?
Intraventricular insult?
Maternal alcohol/substance abuse?
Exposure to TORCH viruses?
Newborn
Vaginal or cesarean birth? History of birth injury? Shoulder presentation? Need for resuscitation/ventilation in immediate newborn period?
Maternal infection or toxemia? Fetal movement during pregnancy? Age of mother and father at time of infant’s birth?
Appropriate gestational age? Apgar scores? Jaundice? Neonatal meningitis? Congenital abnormalities? Newborn screening results?
Infancy
Difficulty feeding? Protuberant tongue or tongue thrust?
Any delay in achieving gross motor milestones? Does infant roll over? Sit without support? Crawl? Stand alone? Walk without support?
Cooing, babbling?
Any evidence of toe-walking?
Any loss of developmental milestones?
Early childhood
Hand dominance? Feeds self?
Any loss of developmental milestones?
Any stumbling, limping, poor coordination?
History of seizures/spasms, staring spells, daydreaming?
Speech development? Attention span? Completion of tasks?
Ability to dress independently?
Independent toileting achieved?
Middle childhood
Visual and auditory perceptions?
Learning difficulties/delays?
History of headaches?
Adolescence
Headache history?
Sports-related concussions?
Environmental risks
Maternal exposure to potential irritants?
Location of housing in relation to hazardous exposures?
History of housing and lead exposures? Contact with chemical cleaning agents, hazardous chemicals, smoke?
Pesticide exposures?
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Neurological system
Only gold members can continue reading. Log In or Register to continue