Neurologic Diseases in Pregnancy
Sarahn M. Wheeler
Irina Burd
A wide range of neurologic disorders can complicate pregnancy. The obstetric care provider is often challenged with managing these symptoms with a limited spectrum of medications known to be safe in pregnancy and a desire to minimize radiographic studies during parturition. Additionally, women with complex preexisting neurologic conditions often achieve pregnancy, necessitating the obstetric provider to be well versed in the treatment of these conditions and the unique implications of these diseases in the setting of pregnancy. This section will review common neurologic complaints and preexisting neurologic conditions and their management during pregnancy.
HEADACHE
Headache is a common complaint in pregnancy.
Although most of these headaches are due to benign causes, it is imperative that obstetric providers perform a thorough history and physical examination to identify those headaches that warrant further workup (Table 19-1).
In the presence of concerning signs or symptoms, neurologic consultation and diagnostic workup should be performed.
TABLE 19-1 History and Physical Exam Findings that Should Prompt Further Headache Workup | ||||||
|---|---|---|---|---|---|---|
| ||||||
Imaging/Diagnosis
Lumbar puncture (LP), magnetic resonance imaging (MRI), and head computed tomography (CT) can be considered for headache with concerning features.
MRI poses no radiation exposure risks to the fetus and is the imaging of choice for pregnant patients. However, MRI is expensive and often not readily available.
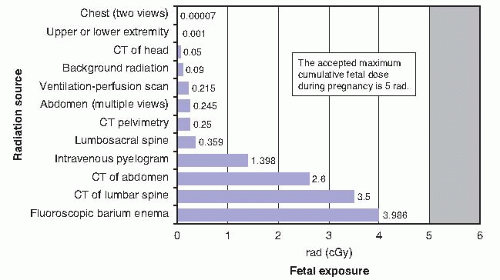
Head CT is the imaging of choice for nonpregnant patients, as it is less expensive and more readily available in most settings. Although head CT does expose the fetus to some radiation, it is approximately 0.05 rad. A fetus must be exposed to 5 rad prior to significantly increased fetal risks, including fetal anomalies or pregnancy loss (Fig. 19-1). As such, the diagnostic benefit of a head CT, as with any clinical test, should be weighed against its risks.
LP is not contraindicated in pregnancy and should be used if clinically indicated.
Common Obstetric Causes of Headache
Any headache beyond 20 weeks’ gestation and up to 12 weeks’ postpartum should be included on the differential diagnosis preeclampsia, and the patient should have a blood pressure check and evaluation for proteinuria. If suspicion for preeclampsia is high, further workup including 24-hour urine collection and laboratory evaluation may be indicated (see Chapter 14).
Post-epidural headache should be considered in postpartum patients particularly in postural headaches. Although acetaminophen, nonsteroidal anti-inflammatory drugs (NSAIDs), and caffeine are often sufficient treatment, anesthesia consultation for blood patching should be considered in patients who are refractory to conservative treatments.
Migraine
Although many chronic migraine sufferers report improved symptoms during pregnancy, it remains a common cause of headache in pregnancy.
Approximately 2% of women have their first migraine while pregnant.
Typical migraine symptoms include unilateral headache with a throbbing quality, nausea, vomiting, and sensitivity to light and sound. Some patients also describe precipitating symptoms such as visual changes or weakness, known as an aura.
Treatment of migraines in pregnancy: Many of the same pharmacologic and nonpharmacologic treatments that are useful outside of pregnancy are also used intrapartum.
Acute symptom management: Treatment of acute migraines can involve a variety of medications (Table 19-2).
Chronic symptom management: Preventive therapy for frequent migraines with beta-blockade and calcium channel blockers can be used in pregnancy. Patients should be aware that prolonged use of beta-blockers may be associated with mild intrauterine growth restriction, transient bradycardia of the neonate, or hyperbilirubinemia.
Refractory symptom management: Selective serotonin reuptake inhibitors (SSRI), serotonin norepinephrine reuptake inhibitors (SNRI), and tricyclic antidepressants may be useful, particularly for patients with comorbid depression.
Although most of the medications used for migraine treatment are safe in pregnancy, there are some notable exceptions. Ergotamine is contraindicated in pregnancy due to its association with hypertonic uterine contractions. Isometheptene is generally avoided due to concern for compromising uterine blood flow.
Tension Headaches
These are the most common type of headache.
Patients describe tightness or tension in their head often with radiation to the neck.
The frequency of tension headaches typically not altered by pregnancy
Treatment: Nonpharmacologic treatments such as heat, massage, rest, and stress management are often helpful. Acetaminophen is the first-line pharmacologic therapy. NSAIDs can be used in the second trimester. Muscle relaxants can often be a useful adjunct. Opioids should be reserved for rare circumstances and for a limited course.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree