Fig. 19.1
The neo-vagina of a normal size formed during surgery
Fig. 19.2
Squamous vaginal epithelium formed in 1.5 months after peritoneal colpopoesis
Technique
Preparation for Surgery
Preoperative evaluation is focused on defining congenital abnormalities of the genital system and on evaluating for the presence of, and the extent of, potential associated abnormalities, as well as attention to patients’ social support and the presence or absence of sexual partners. 94.4 % of our patients have a sexual partner prior to colpopoesis [11].
In each patient, we performed a physical and pelvic and abdominal ultrasound examinations, karyotyping, biochemical profile, CBC, amenorrhea hormonal profile. When needed, magnetic resonance imaging (MRI), intravenous pyelography (IVP), and X-ray of the spine are used. If indicated, extensive counseling is applied. The presence or absence of rudimentary uterine horns and functional endometrium are established.
During pelvic examination, careful attention is given to the position of the urethra, orientation of the vaginal dimple, especially in patients with previous colpoelongation or other techniques, and state and symptomatology related to the fibrotic tissue in patients with previous surgical intervention.
A step-by-step description of the surgery, methods, and the results of studies are provided to the patient, as well as postoperative expectations, especially related to maintenance dilation or intercourse and follow up examinations.
Description of the Operation [2–9]
The surgery is performed utilizing the Adamyan’s laparoscopic-assisted technique of Davydov’s colpopoesis.
After the positioning the patient in lithotomy position with legs in stirrups and the administration of IV antibiotics, evaluation under anesthesia takes place (Fig. 19.3) and diagnostic laparoscopy is conducted in order to identify/confirm the state of the pelvic peritoneum, pelvic organs, presence or absence of the adhesive process, inflammation, endometriosis, or other pathology, as well as mobility of the peritoneum and the state of the vesico-rectal space. During laparoscopy special attention is also given to presence, prominence, and location of the fibro-muscular streaks and the ovarian and tubal appearance (Fig. 19.4).
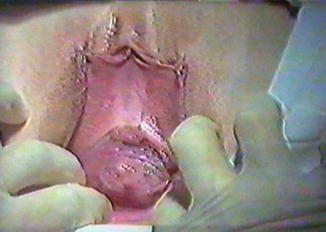
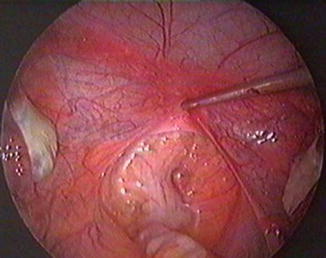
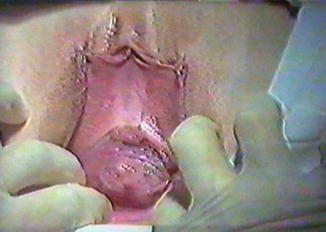
Fig. 19.3
Examination of the external genitalia in the beginning of surgery
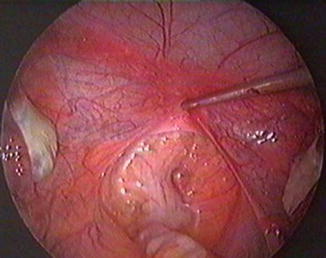
Fig. 19.4
Identification of the most mobile aspect of the peritoneum
With the laparoscope in place for assistance and guidance of vaginal dissection, a transverse incision is made between the lower aspects of the labia minora (Fig. 19.5). With a preference for blunt dissection and, when necessary due to previous scarification, combined sharp and blunt techniques, the channel is formed in the space between the urethra and the bladder and the rectum (vesico-rectal space) (Fig. 19.6).
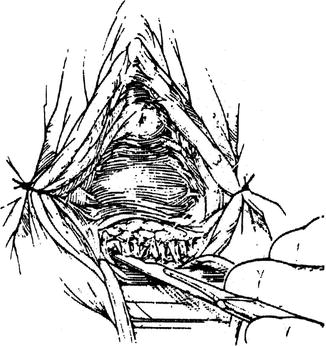
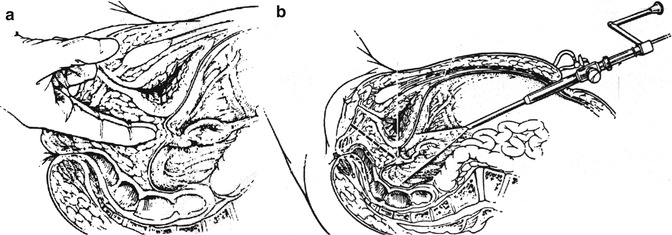
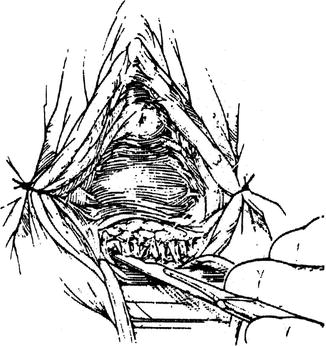
Fig. 19.5
Transverse perineal incision
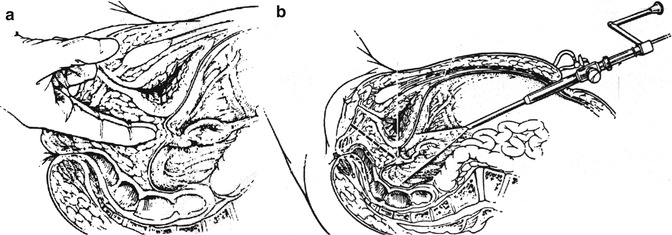
Fig. 19.6
(a) Blunt dissection under (b) laparoscopic guidance in formation of the neo-vaginal channel in the vesico-rectal space
The most mobile aspect of the pelvic peritoneum is introduced into the formed channel with the use of the laparoscopic manipulator and the laparoscope itself (Fig. 19.7a, b). This step is exceptionally important in order to prevent of excessive vaginal tension and labial shifting, as described in the literature [12]. The peritoneum is then grasped with hemostats, and the peritoneum is incised between them using scissors (Fig. 19.8a, b).
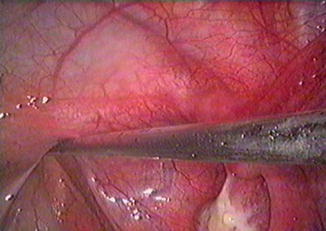
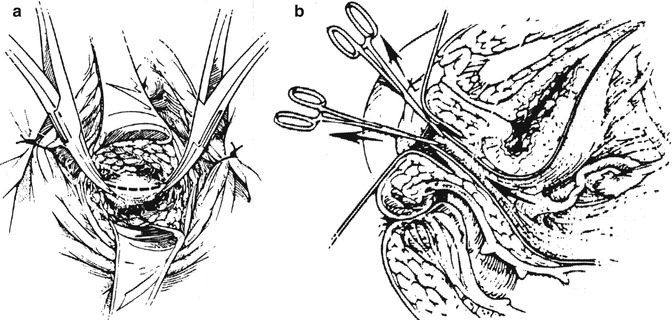
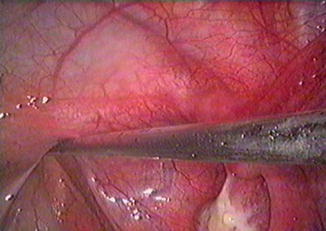
Fig. 19.7
(a, b) Presentation of the most mobile aspect of the peritoneum into the perineal incision
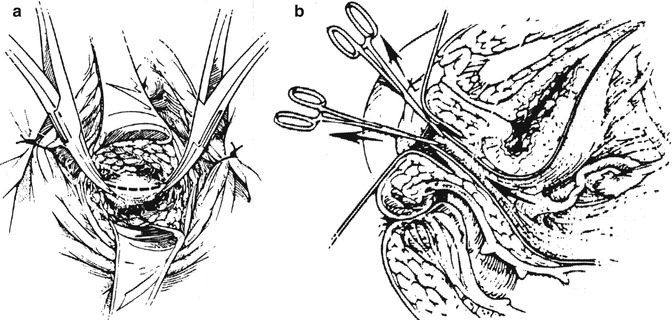
Fig. 19.8
(a) Peritoneal incision followed by (b) the flow of pneumoperitoneal gas
The edges of the peritoneum are further pulled into the formed channel and are attached to the dissected skin of the perineum using interrupted stitches of 3.0 Vicryl. Should the elasticity of the pelvic peritoneum be reduced by previous procedures, laparoscopic placement of this stitch can be employed. Should the peritoneum be prematurely entered due to excessive pressure on it during peritoneal introduction into the perineal incision, the suture including the lateral corners of the pelvic peritoneal incision may be placed and delivered to the perineal incision in order to facilitate the approximation of the perineal and peritoneal incisional edges. A 16-French Foley catheter and a double roll of 4-in. Kling or inflatable vaginal dilator, lubricated with estrogen vaginal cream or a combination of Vaseline and antibiotic cream, is employed.
The apex of the vagina is formed by laparoscopic placement of one or two pursestring stitches of 0 or 1 Proline at a distance of about 11–13 cm from the opening of the neovagina, depending on the patient’s pelvic length and corresponding dimensional anatomy. This stitch involves the peritoneum overlying the bladder, the fibro-muscular streaks, the peritoneum overlying the pelvic sidewall, and serosa of the sigmoid colon or perirectal gutter (Fig. 19.9a, b). A neovagina is thus created (Fig. 19.10a, b). The apical support is provided by the approximation of the fibro-muscular streaks in the described pursestring stitch. Minimal manipulation of the peritoneum is advised.
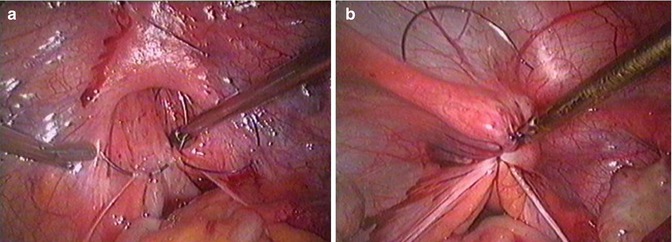
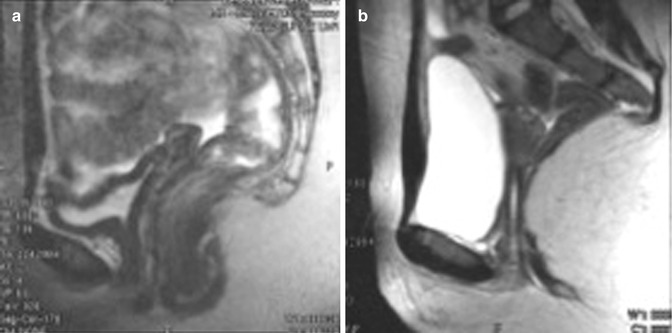
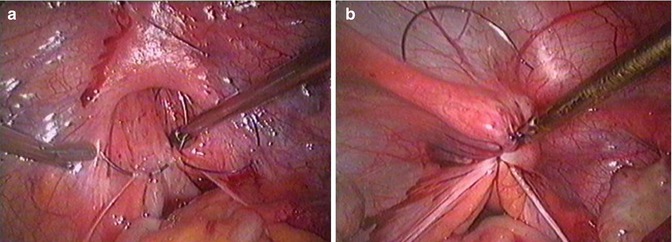
Fig. 19.9
(a, b) Formation of the vaginal apex via laparoscopic pursestrings stitch
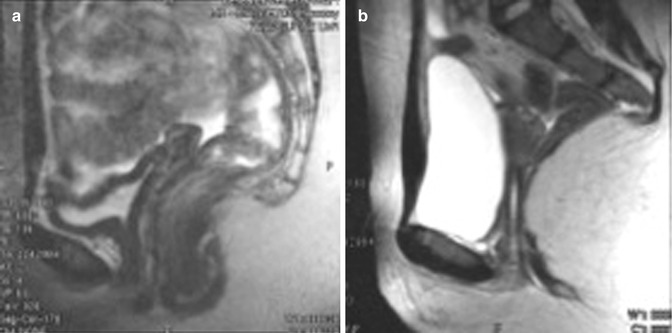
Fig. 19.10
(a) MRI image of the congenitally closed vesico-rectal space. (b) MRI image of the newly formed vagina using Adamyan’s technique.
Postoperative Management
Patients are mobilized in 3–6 h after the surgery and go home on the same day or the next morning with the instructions to follow a regular diet and for pelvic rest as the only restrictions in their activity. In our experience, patients who present from far regions of Russia or other countries, prefer to stay at the hospital until at least the removal of the vaginal tampon (Kling) or inflatable dilator.
Oral antibiotics are used while Foley catheter is maintained until removal of the vaginal packing in 36–48 h. At 36–48 h the tampons are removed and the vaginal walls are carefully examined. Each patient is guided in the performance of her first digital neovaginal examination, followed by focused individualized postoperative counseling, centered on the maintenance of the neovagina with dilation and counseling of the patient on perioperative experience.
At 1 week patients are reexamined with attention to the tissue reaction, vaginal width and length, the condition of the vaginal apex, and the state of the suture line. The aspects of sexual engagement at 4 weeks or thereafter as well as sexual satisfaction are introduced.
We uniformly recommended that sexual intercourse occur not earlier than 4 weeks after the procedure—when the glove or dilator that the patient uses for the maintenance of the neovagina no longer shows evidence of bloodstaining. No maintenance dilation is needed after initiation of regular intercourse.
Surgical Results
Operative time has ranged between 25 and 45 min for all patients without previous surgery or perineal structural abnormality. Median blood loss has been less than 25 cc.
The main characteristics of the neovagina are evaluated at 3–4 months after the surgery. During the gynecologic examination the peritoneo-perineal suture lines are not visible, the length of the neovagina is 11–12 cm, the walls are adequately stretchable, and the width is comfortable to the patients. The walls of the vagina are rougated and moisturized. Conducted with 43 women, morphological and electrono-microscopic evaluation established the presence of the normal vaginal epithelium at this time during postoperative period [11].
The review of the long-term results of our original technique of laparoscopically assisted peritoneal colpopoesis studied functional aspects of formed neovaginas in patients with MRKH as compared with a control group of women who have no somatic pathology, who have regular sexual activity, and who have no history of surgery involving pelvic organs or the pelvic floor [13].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


