Neonatology
Akshaya J. Vachharajani
Amit M. Mathur
APPROACH TO THE NEONATE IN RESPIRATORY DISTRESS
You are looking at a newborn infant in respiratory distress.
Assessment and appropriate treatment of this neonate should be the immediate goal.
Determination of the underlying causes should be the secondary goal.
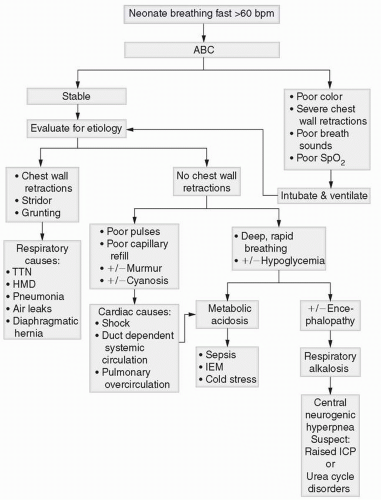
The algorithm in Figure 7-1 summarizes the approach to the infant in respiratory distress.
History
Is the neonate term, late preterm, or preterm?
Are there any risk factors for sepsis in maternal history?
Was meconium noted at delivery?
Physical Examination
Note color and oxygen saturations, capillary refill, pulse volume, and blood pressure.
Measure vital signs; these are vital in assessing the severity of the respiratory distress and also indicate the urgency for intervention.
Etiology
Signs of respiratory distress such as flaring of alae nasi, chest wall retractions, and grunting point to a respiratory (alveolar) etiology
An inspiratory stridor indicates upper airway obstruction.
An inspiratory stridor with poor cry suggests vocal cord paralysis.
Tachypnea (respiratory rate >60 breaths per minute) without chest wall retractions is a good clue to an underlying cardiac etiology or retained interstitial fluid.
Hyperpnea (deep sighing respirations) suggests metabolic acidosis (sepsis, shock, inborn error of metabolism). For more information about cardiac causes, see Figure 7-2.
Laboratory Studies and Imaging
A chest radiograph to differentiate parenchymal (hyaline membrane disease, pneumonia, meconium aspiration, fluid in the minor fissure) from pleural (effusion, pneumothorax) or chest cavity causes (diaphragmatic hernia) of respiratory distress
A capillary blood gas to follow pH and CO2
A complete blood count (CBC) and differential white blood cell count further strengthen or rule out an infectious etiology for the distress. A blood culture is the gold standard for diagnosing or ruling out sepsis, although it can be false-negative in 30% of cases for a variety of reasons (common causes: inadequate blood sample and pretreatment with antibiotics).
Treatment
Guidelines for intubation/surfactant therapy
Some indications for endotracheal intubation and mechanical ventilation of an infant include apnea, poor oxygen saturation despite supplemental oxygen by either nasal cannula or continuous positive airway pressure (CPAP), severe respiratory distress with anterior chest wall retracting to the spine, or poor capillary refill or color.
Prophylactic surfactant therapy through an endotracheal tube was a practice in infants who are <28 weeks estimated gestational age. Recent randomized control trials suggest that prophylactic surfactant, even in the most premature babies, may be avoided by administering CPAP immediately after birth in the delivery room (SUPPORT TRIAL).
See Tables 7-1 and 7-2 for further information about endotracheal intubation in neonates.
Ongoing fluid management
Maintaining fluid and electrolyte balance with 80 mL/kg/day of maintenance fluids (50 mL/kg/day of “starter” parenteral nutrition [2.5 g/kg of protein] plus 30 mL/kg/day of D10W) is a good prescription for the first 24 hours after birth.
Subsequently, the gestational age, urine output, daily weight, and serum electrolytes help guide the amount and type of maintenance fluids including the commencement of enteral feeds.
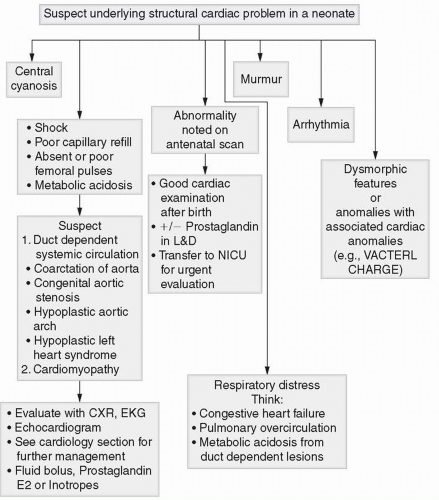 Figure 7-2 Algorithm to use when cardiac disorder should be suspected in a neonate. Look at relevant sections and algorithms for further information about the symptoms and signs mentioned here. |
TABLE 7-1 Endotracheal Tube Size in Neonates | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Special Considerations: Pulmonary Hypertension
Term and late preterm infants with respiratory distress (especially small for gestational age and meconium-stained amniotic fluid) are at a risk of developing pulmonary hypertension. Their size and gestation may delay aggressive intervention (intubation, mechanical ventilation). They could develop pulmonary hypertension (because unlike preterm infants, they have well-developed media in their pulmonary arteries that respond to hypoxia with vasoconstriction).
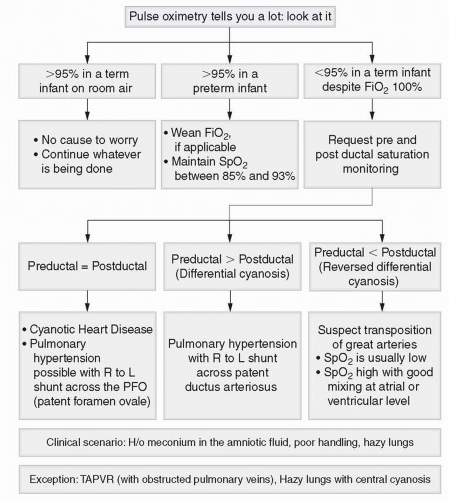
The first sign of trouble is poor handling with desaturation. Preductal and postductal saturation differential of >10% (differential cyanosis, pink hands, blue feet) indicates right-to-left shunting across the patent ductus arteriosus (PDA). Absence of this sign does not preclude the right-to-left shunting, which may be across the foramen ovale.
It is advisable to maintain oxygen saturation >95% in term infants until their disease process is identified and pulmonary hypertension is ruled out.
APPROACH TO THE NEONATE WITH A HEART MURMUR
I hear a murmur today! You have missed it (did you examine the infant?), and the nurse hears it.
A murmur may or may not indicate heart disease.
Examine the infant.
Use the fifth sign (pulse oximetry) for its diagnostic value.
Measure blood pressure in all four extremities.
Look at chest radiograph and electrocardiogram (ECG) if available.
Perform a hyperoxia test if necessary.
This composite information can be used for a diagnosis.
TABLE 7-2 Endotracheal Tubes and Depth of Insertion in Neonates* | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||
Differential Diagnosis
Does this neonate have heart disease?
A neonate who has any of the characteristics in the flow chart above should be suspected to have heart disease.
All neonates are screened for a congenital heart disease after birth, with pre- and postductal pulse oximetry before discharge. Pre- and postductal pulse oximetry in room air should be individually 95% or greater. If the Spo2 is less, then the baby should have a detailed examination including an echocardiogram to evaluate for structural heart disease.
If a term or preterm neonate looks well and has a normal examination, then think of the following:
Innocent murmur. In a term infant who is on room air, has a pulse oximetry >95%, is feeding well, looks well, and has a normal examination except the murmur, the murmur is very unlikely to represent a cardiac emergency requiring an urgent echocardiogram and consult. A majority of such murmurs are innocent and need only monitoring and clinical follow-up.
Tricuspid regurgitation from physiologic pulmonary hypertension
Hemodynamically insignificant PDA that is closing. Repeat examinations confirm the disappearance of the murmur.
Is the neonate in shock or congestive heart failure?
Poor capillary refill, poor pulse volume, tachycardia, low blood pressure, and metabolic acidosis suggest shock. Remember the definition of compensated and hypotensive shock from PALS (compensated shock is shock without hypotension and hypotensive shock is shock with hypotension). Use it clinically.
Tachycardia, tachypnea or respiratory distress, hepatomegaly, or cardiomegaly on chest radiograph suggests congestive heart failure.
Etiology
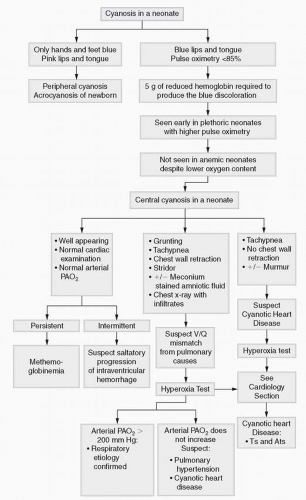
Is the heart disease cyanotic or acyanotic? The differential diagnosis is extensive, and the diagnosis is difficult. Use the algorithm presented in Figure 7-3 for guidance.
A hyperoxia test is useful, and making a diagnosis of pulmonary hypertension versus cyanotic heart disease is critical. If the Spo2 is >95% on room air or supplemental oxygen, it is unlikely that the neonate needs a hyperoxia test.
Pulmonary hypertension is best diagnosed based on clinical circumstances. The presence of the murmur of tricuspid regurgitation is a small piece of information that is not diagnostic. Red flags for pulmonary hypertension are in Figures 7-3 and 7-4.
A term infant with meconium-stained amniotic fluid at birth with low pulse oximetry and hazy lung parenchyma with high Pco2 and low Po2 and differential cyanosis probably has pulmonary hypertension from meconium aspiration syndrome. If the infant has a normal Pco2 and a low pulse oximetry, cyanotic heart disease may be suspected in this same infant because the normal or low Pco2 points against significant lung disease. The hyperoxia test may not be diagnostic in this situation. A very low Pao2 can be obtained on the hyperoxia test in both severe pulmonary hypertension and cyanotic heart disease.
The information from pulse oximetry, outlined in Figure 7-4, may be useful in diagnosing congenital heart disease.
A big infant (term) with hazy lungs and low Pao2 should make the clinician suspicious for total anomalous pulmonary venous return (TAPVR) with obstructed
veins. Big infants do not commonly have hyaline membrane disease, and making a diagnosis of pulmonary hypertension in these infants and starting nitric oxide can be lethal if they have the TAPVR; the nitric oxide will cause pulmonary edema and worsen the prognosis. It is imperative to consider nitric oxide therapy very carefully. An echocardiogram should be obtained as soon as possible.
The etiology is not as important as recognizing the physiologic situation, instituting the treatment (prostaglandin or afterload-reducing agents), and calling for urgent cardiology evaluation.
Clinical Diagnoses
Certain heart murmurs are common in certain clinical scenarios.
Murmur in a large for gestational age infant of a diabetic mother or a neonate on chronic steroid therapy: Think of hypertrophic cardiomyopathy.
Murmur in a neonate with trisomy 21: Think of atrioventricular canal defect.
Murmur in a preterm neonate: Think of PDA.
Murmur in a preterm neonate with a cataract: Think of PDA and rubella syndrome.
Murmur in a neonate with an arrhythmia: Think of the Ebstein anomaly, especially if the mother received lithium while pregnant.
For further details on murmurs, please see Chapter 12, Cardiac Concerns.
APPROACH TO THE NEONATE WITH APNEA AND BRADYCARDIA
You are called to look at an infant with heart rate drops. This may be the only evident sign, but it is usually a manifestation of apnea. Apnea is not recorded if one is not observant; obstructive apnea may be missed as the apnea monitors used in clinical practice detect chest wall movements (plethysmographs). The chest wall will continue to move in obstructive apnea, and no alarms will go off. The chest wall stops moving with central apnea, and hence, the monitors in clinical use will detect only central apnea.
Urgent assessment and instituting lifesaving interventions should be the immediate goal.
Examine the infant first and assess for signs of well-being or sepsis.
Heart rate drops in a sick neonate may demand urgent therapeutic interventions such as endotracheal intubation.
Stabilize the infant first (ABCs).
Think about the etiology and additional appropriate intervention after initial stabilization.
Differential Diagnosis
Events are recent in onset, and the neonate is ill appearing.
Sepsis. Management includes a CBC, blood culture, chest radiograph (pneumonia) or obstructive series (necrotizing enterocolitis), lumbar puncture, and commencement of antibiotics. Lumbar puncture is considered mandatory in a neonate with heart rate drops because this may be the only symptom of meningitis. Up to 30% of meningitis cases can exist with a negative blood culture.
Respiratory distress. Management includes increasing respiratory support such as administering CPAP, which should be administered before ordering a capillary gas analysis. A capillary gas analysis may reveal normal pH and CO2 because minute ventilation is maintained by increasing the respiratory rate. Waiting to institute CPAP until the capillary gas results are abnormal may lead to alveolar atelectasis that may not respond to CPAP. Mechanical ventilation through endotracheal intubation may then be required.
Events are recent in onset, and the neonate is well appearing.
Sepsis. Indications for septic workup include a history of temperature instability, feeding intolerance, abdominal distension, and lethargy. See previous discussion for management.
PDA. Evaluate pulse volume, pulse pressure, and precordial pulsations. PDA can occur with or without a murmur.
Anemia. Severe anemia in premature infants can present as new onset of apnea and bradycardia. Check a CBC, and if the Hb is <7 g/dL, consider transfusing pRBCs. Remember anemia can coexist with sepsis.
Blocked ectopic atrial beat. This is a common cause of heart rate drop in preterm infants and is self-limiting. It does not necessarily cause hemodynamic compromise and warrants an ECG.
Obstructive apnea from incoordinated suck and swallow, if associated with recently introduced oral feeds or noticed while the infant is feeding from a bottle
Incorrect position of a feeding tube. Check with chest radiograph.
Eye examination for retinopathy of prematurity (ROP). This is a common cause of heart rate drop as a result of the vagal stimulation from eyeball compression during the examination (these infants could also have tachycardia from anticholinergic effects of cyclopentolate drops for the eye examination).
Vagus nerve induced. In a ventilated infant where the airway is patent (endotracheal tube), it is unlikely to be obstructive in origin and more likely to be central. Consider vagus nerve-induced bradycardia from increased intracranial pressure or more commonly a low-lying endotracheal tube irritating the carina.
Not ready for weaning. In an infant who is being weaned from ventilator support, heart rate drops and apnea indicate that it is necessary to think twice about extubating the infant or weaning the current support irrespective of blood gas analysis. It may also be a clue to starting or adjusting the dose of caffeine before extubating or stopping CPAP.
Intraventricular hemorrhage (IVH). Consider if it is the first 24 hours of life in an extremely premature infant (<26 weeks gestation), especially if there is a rapid hemoglobin drop. An ultrasound of the head is diagnostic. IVH is most likely to occur in the 1st week of life, and hence, ultrasound of the head after the 1st week of life (in response to apnea and bradycardia) is less likely to be fruitful.
Hydrocephalus. Consider if an infant with known IVH has an increasing occipitofrontal circumference, bulging fontanelle, and increasing frequency of heart rate drops. Weekly ultrasounds should be considered.
Events are not new in onset, and the neonate has a history of heart rate drops.
If the infant is well, then spending time on eliciting history is worth the time and trouble.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree