Antepartum factors
Postpartum factors
Maternal diabetes/gestational diabetes
Premature labor/precipitous labor
Chronic medical illness – cardiac, renal, pulmonary, neurologic disease
Emergency caesarean section
Gestational hypertension/pre-eclampsia/chronic hypertension
Assisted delivery – forceps/vacuum
Age< 16 years or >35 years
Breech or abnormal presentation
Primigravida or grand multipara
Macrosomia
Maternal infections/TORCH/sexually transmitted diseases/chorioamnionitis
Abruptio placenta/cord prolapsed/placenta previa
Oligohydraminos/polyhydraminos
Prolonged labor/obstructed labor
Bleeding in second or third trimester
Meconium-stained amniotic fluid
Previous fetal or neonatal deaths/fetal malformations/diminished fetal activity
Narcotics given to mother within 4 h of delivery
Multiple gestations
Use of general anesthesia
Fetal anemia/isoimmunization
Altered fetal heart rate changes
Premature or prolonged rupture of membranes
Significant intra partum bleeding
Preparation for Resuscitation
Personnel
At every delivery, one must ensure that at least one trained NRP personnel is present and his/her primary responsibility is the newly born. For anticipated high-risk deliveries or for those with expected problems, at least two trained people are required. For multiple births, separate team is required for each baby [1, 3, 4].
Equipment
All the equipment necessary for a complete resuscitation should be regularly checked to ensure that they are available in various sizes and are functional. The equipments needed included in the Table 39.2 below.
Table 39.2
Equipment required for resuscitation
Radiant warmer or other heat source |
Resuscitation trolley with firm surface |
Warm blankets/pre-warmed linen or towels, shoulder roll |
Stethoscope with neonatal head |
Oxygen source, compressed air source |
Oxygen blender (for mixing air and oxygen with flow meter) |
Suction source, suction catheter (5, 6, 8, 10, 12 F) |
Delee’s mucus extractor and meconium aspirator |
Pulse oximeter and oximeter probe |
Nasogastric tubes (8 F) |
Ambu or self-inflating bag, flow inflating bag, T-piece resuscitator |
Face masks (newborn and premature sizes, cushioned rim masks) |
Laryngoscopes (handles no. 00,0 and 1 blade; batteries), stylet |
Endotracheal tubes (2.5, 3, 3.5, 4 mm) |
Epinephrine (1:10,000 solution) 3 ml or 10 ml ampoules |
Volume expanders (normal saline, Ringer’s lactate, 5 % albumin, O-negative whole blood (cross matched against mother’s blood)) |
Clock (Apgar timer) |
Syringes, hypodermic needles, and tubes for collection of blood samples |
Equipment for umbilical cord catheterization |
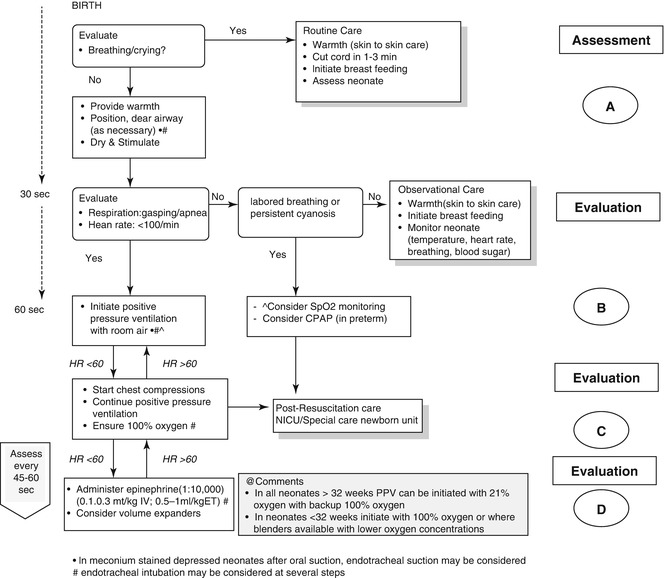
The Resuscitation Flow Diagram (Fig. 39.1)
The above flow diagram describes the steps necessary to determine the need for resuscitation and all the NRP resuscitation procedures [3].
Initial Assessment
At the time of birth, as per the IAP -NRP FGM (first golden minute) guidelines one should ask only one question, i.e., breathing or crying and then proceed after that as per the response as yes or no.
If the newborn baby is breathing well or crying, then the baby does not need resuscitation and should be kept with the mother and sent for routine care.
Routine Care Involves
Provide warmth (skin-to-skin care)
Cut cord in 1–3 min
Initiate breastfeeding
Assess neonate/ongoing evaluation
If any answer is “No” to the question on breathing or crying, then one should continue with initial steps of resuscitation.
Block A (Airway)
These are initial steps to establish an airway and begin resuscitating newborn. Approximately 60 s (“The Golden Minute”) are allotted for completing the initial steps, reevaluating, and beginning ventilation if required (Fig. 39.1) [3].
Initial Steps of Resuscitation
1.
Keep baby warm by wrapping him with towel and placing him on mother’s abdomen/chest for skin-to-skin contact with the mother. If the baby has not cried, then place the baby under radiant heat warmer on a resuscitation table.
2.
Open the airway by slightly extending the neck, thus creating the “sniffing” position.
3.
Clear airway as necessary. Secretions can be cleared by wiping the nose and mouth with towel or by suctioning with a bulb syringe or suction catheter. Always suction “mouth before nose” by thinking “M” before “N” in the alphabet to prevent aspiration of mouth content. Clearing the airway involves endotracheal suctioning to clear meconium for non-vigorous newborn with meconium-stained fluid [1].
4.
Dry and stimulate to breath. To minimize heat loss, the baby should be received in pre-warmed towel. The same can be used to dry him and this should be removed and another fresh pre-warmed towel should be used for continued drying and stimulation. Tactile stimulation can be provided by slapping or flicking soles of the feet or by gentle rubbing the newborn’s back, trunk, or extremities.
Assessment of the Effect of Block A
The next step is to evaluate to determine if further resuscitation actions are indicated. The entire resuscitation process up to this point of initial steps should take no more than 30 s (unless suctioning of meconium from the trachea was required). Evaluate simultaneously for respirations (apnea, gasping, or labored breathing) and heart rate (whether heart rate is greater than or less than 100 bpm [beats per minute]).
Respirations – Observe baby for good respiratory efforts. Rate and depth of respiration should increase after a few seconds of tactile stimulation.
Heart rate – The heart rate should be more than 100 bpm. The simplest method to determine heart rate is to feel for a pulse at the base of umbilical cord. If you cannot feel a pulse, use stethoscope to auscultate. Counting the number of beats in 6 s and multiplying by 10 provide a quick estimate of the beats per minute.
Block B (Breathing)
If the baby is apneic, or has gasping respirations, or if the heart rate is below 100 bpm, you should proceed immediately to providing PPV with room air. However, if the baby is breathing and the heart rate is above 100, but the respirations appear labored or the baby appears persistently cyanotic administer continuous positive pressure (CPAP) with mask. Consider SpO2 monitoring and one should attach an oximeter to determine the need for supplemental oxygen, and it is recommended that the probe be placed on newborns right hand or wrist so as to detect pre-ductal saturation.
Positive Pressure Ventilation (PPV)
Three devices are available to ventilate newborns to give PPV are self-inflating bag, flow-inflating bag, and T-piece resuscitator [1, 3].
Concentration of Oxygen During Resuscitation [1]
Meta-analyses showed a decrease in mortality and CNS effects in room air-resuscitated group of neonates. Therefore, it is recommended that:
In term as well as preterm newborns, resuscitation can be initiated with room air.
Titrate O2 to achieve SpO2 in target range as described using pulse oximetry for uncompromised babies (the targeted pre-ductal SpO2 at 1 min is 60–65 %, 2 min – 65–70 %, 3 min – 70–75 %, 4 min – 75–80 %, 5 min – 80–85 %, and at 10 min it is 85–95 %).
Use oxygen blender, if available, to deliver an oxygen concentration between 21 and 100 %.
If bradycardia (HR <60) after 90 s of resuscitation with lower concentration of O2, increase concentration to 100 % until recovery of normal heart rate is achieved.
Resuscitation Rate during PPV
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree