Needles, Sutures, and Knots
Mastering the use of needles, sutures, and instruments, as well as the technique of knot tying, is the technical foundation of the surgeon’s craft. A bewildering array of needles and sutures are available; some offer distinct advantages in specific situations, while others are simply competitive equivalents. This chapter describes the variety of available needles and sutures, as well as guidelines for their selection and use.
NEEDLES
Surgical needles consist of three structural parts: the swage or eye, the body, and point types, depending upon their intended surgical use. Each variation has advantages and disadvantages.
THE SWAGE (EYE)
Three types of eye are in common surgical use: swaged, controlled release (“pop-off”), and open. With a swaged-on shank, the suture is placed inside the hollowed end of the needle and crimped into place by the manufacturer. The convenience and ease of surgical manipulation makes this design ideal for most obstetric applications. The diameter of the swaged-on needle end is larger than that of the rest of the needle and determines the size of the suture tract (Bennett, 1988).
Controlled-release needles are similar to swaged-on needles but are designed to be released (“pop-off”) with a sharp tug of the needle holder. This enables needle removal of interrupted sutures without the suture being cut.
The advantage of open-eyed needles is that they allow the use of a variety of suture types and diameters. Such needles generally are manufactured in uncommonly used sizes because prepackaging with a spectrum of suture types is economically unfeasible. Open-eyed needles are rarely used in obstetric surgery, but occasionally they are helpful in specialized situations, such as uterine artery ligation or cerclage placement.
THE BODY
The needle body may be round, triangular, or ovoid, and is tapered gradually to the point. Triangular needles have three cutting edges. Ovoid needles may be flattened on top and bottom with rounded sides, or flattened on all four sides, producing a square or rectangular body. Some needle bodies also are ribbed longitudinally on the inner curvature to allow them to be securely grasped by the needle holder.
The needle body may be either straight or curved. Most curved needles have either a ½ or  circle configuration, although a
circle configuration, although a  -circle needle is sometimes used in vaginal surgery (Fig. 1-1). The
-circle needle is sometimes used in vaginal surgery (Fig. 1-1). The  -circle needle is most commonly used in obstetrics, however, the ½- or
-circle needle is most commonly used in obstetrics, however, the ½- or  -circle design facilitates maneuvering in small places.
-circle design facilitates maneuvering in small places.
FIGURE 1-1. Parts of a curved surgical needle and various needle circle lengths. (Modified from Ethicon, Inc., 1993, with permission.)
THE POINT
Needles are most commonly classified according to the cross section of their point (Fig. 1-2). Needle points may be either tapered, cutting, reverse cutting, or blunt. Cutting needles are more likely to pull through tissue than are tapered points, which are used for softer tissues such as uterus and fascia. The blunt point is used for very friable tissues, or occasionally for cannulating, and does not easily penetrate gloves.
FIGURE 1-2. Surgical needle points and bodies. (Reprinted with permission from Ethicon, Inc., 1993.)
Because conventional cutting needles have the cutting edge directed toward the wound edge, they have a greater tendency to pull through when tightened than does the reverse cutting needle, with its flat surface toward the wound (Fig. 1-2). While most commonly available cutting needles are of the reverse cutting design, conventional cutting needles may be useful for very-fine skin suturing.
Lewis and colleagues (1995) reviewed a number of methods to reduce the incidence of sharp injuries in obstetric and gynecologic surgery. They conclude that many maneuvers with sharp instruments can be replaced with less dangerous techniques.
USING THE NEEDLE
Curved needles are designed to be grasped and driven through tissue with a needle holder. The placement of the needle in the holder is dependent upon the tissue to be sutured. Where a long tract is planned or little resistance will be encountered—with uterine closure, for example—the needle may be grasped  or
or  of the distance from point to eye. Where tougher tissue is encountered—for example, the pubic periosteum—the needle is more appropriately grasped in the middle, or even slightly toward the point, to facilitate needle passage and to avoid deformation of the needle.
of the distance from point to eye. Where tougher tissue is encountered—for example, the pubic periosteum—the needle is more appropriately grasped in the middle, or even slightly toward the point, to facilitate needle passage and to avoid deformation of the needle.
Curved needles should not be grasped with the hand. In a review of surgical glove perforation in obstetrics, Serrano and associates (1991) described a 13 percent rate of glove perforation. The majority of perforations occurred in the nondominant hand, suggesting perforation due to grasping of the needle. Such technique increases the risk of infection transmission to both patient and physician (Dalgleish and Malkovsky, 1988). Longer, straight needles of the Keith type are sometimes used manually (without a needle holder) for mattress-type skin closures. These, too, are injury prone.
SUTURES
Sutures have been used for centuries either to approximate tissue or to ligate vessels. Wound suturing was described as early as 3500 BC in an Egyptian papyrus, and was used by Galen, physician to the gladiators, to stop their bleeding (Snyder, 1976; Stone, 1988). During the Middle Ages, however, many earlier advances were forgotten, and hemostasis was accomplished primarily through cauterization. With the Renaissance came renewed interest in the use of suture material; by the fifteenth century, horsehair, flaxen thread, and gut material were described. In the nineteenth century, both buckskin and silver wire were used in various types of gynecologic surgery (Snyder, 1976; Stone, 1988).
Joseph Lister, who pioneered the concept of antisepsis (1869), made the first major advance in suture material. His chromatization of gut suture in 1876 resulted in significant prolongation of suture tensile strength. In Lister’s day, the violin was often referred to as a “kit.” The most common source of gut material for suture was violin strings fashioned from sheep or ox intestines; thus the term “kitgut” was introduced, which later became “catgut” (Stone, 1988).
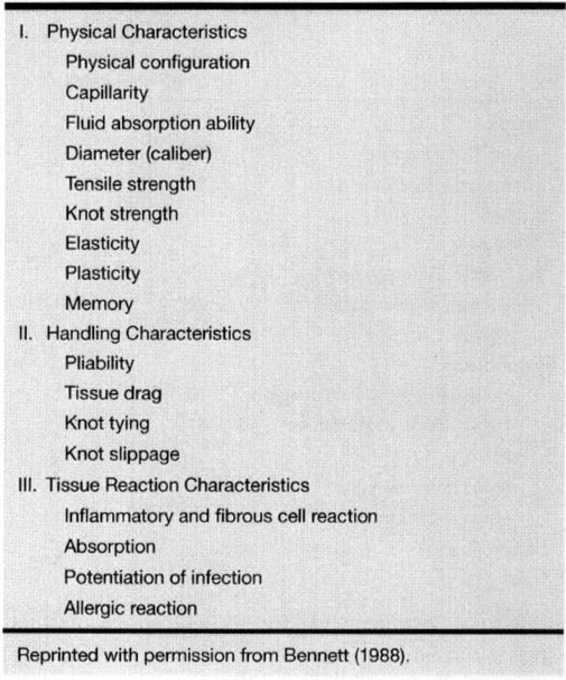
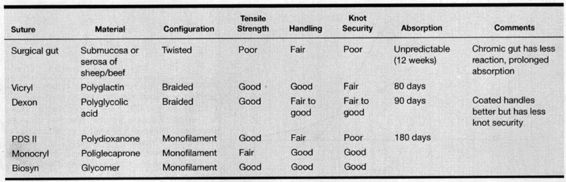
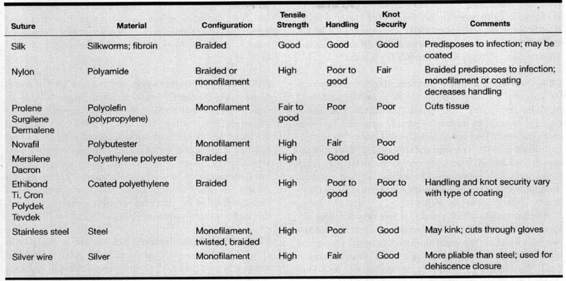
Table 1-1 describes various characteristics of suture material. The ideal suture would cost little, tie easily and securely, possess superb tensile strength, and have no adverse effect upon wound healing or infection rates. Unfortunately, no suture meets all of these requirements. Therefore, compromises must be made when selecting suture material because each type has both advantages and disadvantages.
TABLE 1-1. Characteristics of Suture Material
PHYSICAL CHARACTERISTICS
Physical configuration refers to mono- or multifilamentous construction of the suture material. Multifilamentous materials tie more easily, but also have an increased tendency to harbor bacteria in the braiding (Bennett, 1988).
Capillarity refers to ability of suture to absorb fluid from a wet end to a dry end. Fluid absorption ability is the capacity of a suture to absorb fluid when immersed. Both of these characteristics also increase the tendency to absorb and retain bacteria. For example, braided nylon, a material with high fluid-absorption capability and capillarity, absorbs three times as many bacteria as the corresponding monofilament suture (Bucknall, 1983).
Diameter is determined in millimeters, but is commonly expressed according to USP standards (3-0, 4-0, etc). However, specific tensile strength and diameter affect USP terminology; thus 4-0 catgut has a slightly larger diameter than 4-0 nylon.
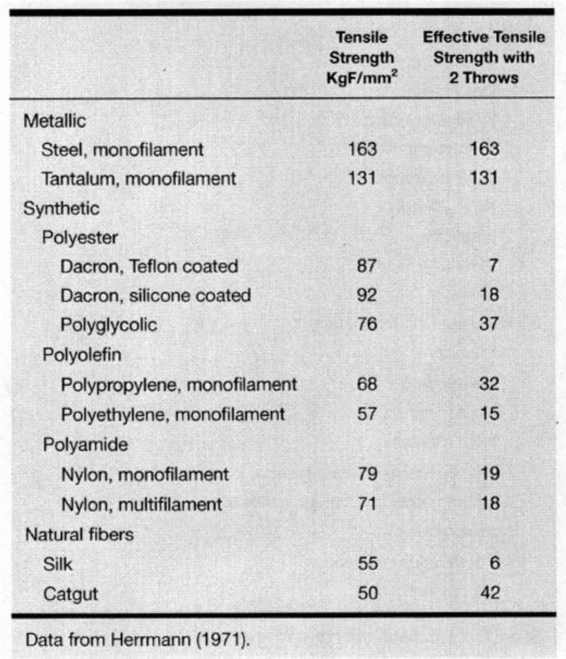
Tensile strength is defined as the amount of weight necessary to break a suture divided by its cross-sectional area. Thus the breaking load will be quadrupled by a doubling of suture diameter. A knotted suture has roughly ⅓ the strength of an unknotted suture; the strength depends to some degree upon the type of knot used (Rodeheaver and associates, 1981; Tera and Aberg, 1977). Table 1-2 lists relative tensile strengths of various knotted and unknotted suture materials. Note the dramatic decline in strength of knotted versus unknotted suture for all except metallic sutures. Figure 1-3 represents the relationship between suture diameter and tensile strength (Herrmann, 1971). Figures 1-4 and 1-5 represent tensile strength over time following suture placement.
TABLE 1-2. Physical Characteristics of Surgical Suture Materials
FIGURE 1-3. Knot pull-breaking strength of various sizes of surgical sutures. Size and strength are not linearly related. (Reprinted with permission from Herrmann, 1971.)
FIGURE 1-4. Nonabsorbable sutures, percentage strength remaining. Polyester (Ethibond and Mersilene) sutures (A) and polypropylene (Prolene) sutures (B) retained 100 percent of original breaking strength after 400 days. Monofilament nylon (Ethilon) sutures (Q retained about 80 percent of original breaking strength. Multifilament nylon (D) lost slightly more of its original strength than the monofilament suture. Silk sutures (E) degrade and lose strength more rapidly, with usually less than 50 percent of the original strength remaining at two months. Data are from size 2-0 and 4-0 sutures implanted in rat subcutaneous sites. (Reprinted with permission from Salthouse, 1980.)
FIGURE 1-5. Absorption profile of chromic surgical gut (G) and synthetic absorbable polyglactin 910 (Vicryl) suture (V). Size 4-0 sutures were implanted in a rat gluteal muscle and absorption was calculated from cross-sectional area remaining. Absorption of surgical gut is seen by 14 days; synthetic absorbable suture shows evidence of absorption at about 35 days, but is more rapid thereafter. (Reprinted with permission from Salthouse, 1980.)
Tensile strength also is affected by surgical technique. For example, a stray knot in a Prolene suture decreases tensile strength by 17 percent and grasping a suture with forceps or needle holder decreases suture strength in a dose-dependent fashion (Stamp and associates, 1988; Abidin and associates, 1989).
Knot strength refers to the force necessary to cause a given type of knot to slip, either partially or fully, and is dependent upon the coefficient of friction of the material and the material’s stretch capability (Bennett, 1988).
Elasticity refers to the tendency of the suture to return to its original form after stretching. With high elasticity, a suture will be easily stretched by tissue swelling and will not tend to cut into or through the tissue. Plasticity refers to the tendency of the suture to retain its new form after stretching. A highly plastic suture will retain its larger form even after tissue swelling subsides, and may become loose. The tendency of suture material to cut through tissue is also directly related to tensile strength, inversely related to suture diameters, and dependent upon tissue type. The tendency for suture to cut through tissue is least with fascia, followed by muscle, peritoneum, and fat (Bennett, 1988; Tera and Aberg, 1976a).
The forces required for suture to tear various tissue types also changes with the duration of the healing process. From week 1 to week 2 following surgery, the tendency of suture to cut through tissue is less than in the immediate postoperative period (Aberg, 1976).
Memory refers to the tendency of a material to return to its original shape after deformation, for example, tying (Bennett, 1988). Suture with a high memory attempts to return to its original shape, and thus does not hold a knot well. Nylon is an example of a suture with a high degree of memory.
HANDLING CHARACTERISTICS
Pliability is a subjective term related to how easily suture can be bent (Bennett, 1988). Relatively pliable sutures such as silk are easier to handle than stiffer, monofilament nylon sutures.
The coefficient of friction of a suture can be viewed as a measurement of “slipperiness” (Bennett, 1988). The inherent coefficient of friction of a given suture material may be altered by the application of special coatings. Sutures with high coefficients of friction are more difficult to pull through tissue. Materials with low coefficients of friction (monofilament nylon or coated polyglactin, for example) are easier to set by a slipknot, but may more easily come undone. For example, a simple square surgeon’s knot with uncoated Dexon approaches maximum knot security, but the same knot tied with coated Vicryl is insecure (Trimbos, 1984).
TISSUE REACTION CHARACTERISTICS. All suture material is a foreign substance and will elicit a tissue reaction directly related to the amount of suture material present (Bennett, 1988). In this respect, the less suture used, the better. Furthermore, the diameter of suture used under many circumstances is more closely linked to adhesion formation than the inherent reactivity of the material itself (Stone, 1988).
Three sequential histologic stages have been described in the normal reaction of tissue to suture material (Madsen, 1953; Postlethwait and colleagues, 1975). Stage I occurs during days 1—4, and consists of a leukocytic infiltrate including polymorphonuclear leukocytes, as well as lymphocytes and monocytes. During Stage II (days 4-7), there is infiltration with macrophages and fibroblasts. Stage III, which occurs after the seventh day, consists primarily of a chronic inflammatory response and the appearance of additional fibrous tissue, with the formation of a fibrous capsule by day 28 (nonabsorbable suture) or a continued inflammatory response resulting in eventual complete absorption of the suture (absorbable suture).
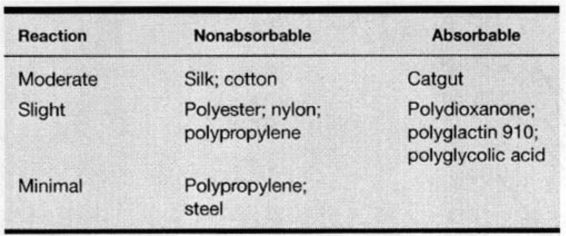
Table 1-3 ranks suture material according to tissue reactivity. Within this ranking, multifilamentous suture elicits greater tissue reaction than monofilamentous material and increases the risk of infection to a greater degree (Alexander, 1967; James, 1961; Sharp, 1982; and their associates). Risk of infection is also greater with braided suture material that can harbor bacteria in the interstices, where they are less susceptible to actions of leukocytes. Knots similarly provide interstices favorable to bacterial growth, suggesting that the number of knots placed should be minimized (Bennett, 1988; Osterberg, 1983).
TABLE 1-3. Relative Tissue Reactivity to Sutures
SPECIFIC SUTURE TYPES
Specific properties of absorbable and nonabsorbable sutures are detailed in Tables 1-4 and 1-5. The terms absorbable and nonabsorbable are relative. Plain catgut, for example, which is an absorbable suture, may persist in tissue for many years (Postlethwait and colleagues, 1975), and with the exception of polyester (Dacron), polypropylene (Prolene), and stainless steel, all “nonabsorbable” sutures eventually degrade or are absorbed (Nilsson, 1982; Edlich and associates, 1974). By convention, sutures that retain significant tensile strength beyond 60 days are commonly classified as “nonabsorbable” (Bennett, 1988).
TABLE 1-4. Comparison of Absorbable Sutures
TABLE 1-5. Comparison of Nonabsorbable Sutures
CATGUT. Catgut sutures are made from the submucosa of sheep or from the intestinal serosa of cattle. Chromic
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree