Genital Tract Lacerations and Puerperal Hematomas
A number of injuries may affect the genital tract during labor and delivery. Although these are more common and tend to be more severe with traumatic and instrumental delivery, they may complicate any delivery. Most commonly, these lacerations are minor and involve the perineal body, superficial vagina, and cervix. Deeper lacerations may involve large vessels that, if not repaired, will cause serious hematomas. These, in turn, may dissect below the levator muscle sling to cause vulvar and vulvovaginal hematomas, or they may dissect upwards to form subperitoneal hematomas.
One of the most dreaded injuries during childbirth is rupture of the uterus. While uncommon, rupture of the previously intact uterus remains one of the most dangerous obstetric catastrophes. More commonly, the uterus ruptures at the site of a previous cesarean incision during a planned trial of labor following one or more prior cesarean deliveries.
LOWER GENITAL TRACT LACERATIONS
VAGINAL LACERATIONS
The most frequent vaginal lacerations are spontaneous posterior tears involving the midline or in the anterior periurethral areas. Posterior lacerations of the perineal body or vagina should be repaired if they involve more than the vaginal mucosa. Repair of such posterior injuries is described in Chapter 5. Anterior tears involving the labia minora and periurethral area are inspected; if they are not bleeding, they generally do not require repair. If the lacerations are close to the urethra and require repair, it is prudent to insert a Foley catheter. This not only facilitates the repair with the knowledge that the urethra is not being compromised, but also guards against the development of edema, which may make it difficult for the patient to void. Repair is generally performed with a fine suture, such as 000 or 0000 chromic catgut, Dexon, or Vicryl.
Occasionally there may be deep sidewall lacerations so extensive that they dissect into the ischiorectal fossae. This is heralded by the appearance of the yellow fibroadipose tissue characteristic of this space. While such injuries are indeed impressive on visualization, the muscular layers usually are easily repaired. The fibroadipose tissue itself cannot be repaired as the suture material simply will pull or cut through this tissue. Inspection should be carried out and any isolated bleeding vessels ligated with either a clamp and free tie or with a suture ligature. Following this, the vaginal mucosa is closed with either a running-locking suture or with interrupted sutures. Most obstetricians prefer to use a running-locking suture because it is more hemostatic. A large needle and 00 chromic suture are used for this closure with successive bites incorporating substantial amounts of tissue. Remarkably, at the postpartum examination there usually is little residual evidence of these injuries.
CERVICAL LACERATIONS
In the second edition of Williams Obstetrics, J. Whitridge Williams (1911) observed: “Slight degrees of cervical laceration must be regarded as an inevitable accompaniment of childbirth. Such tears, however, heal rapidly and rarely give rise to symptoms. In healing, they cause a material change in the shape of the external os, thereby affording us a means of determining whether a woman has borne children or not.” Since Williams made these observations, little has been published on cervical lacerations during childbirth. Indeed, while virtually every obstetric textbook includes a discussion of cervical lacerations, there is no referenced work reporting the incidence of even those lesions associated with hemorrhage. Fahmy and associates (1991) reported on a series of colposcopic examinations performed in 189 successive parturients within 6–48 hours of delivery with attention directed toward evidence of type, site, and extent of cervical trauma and its relation to various obstetric factors. In two-thirds of the parturients, they found trauma that presented as an erosion in 79 percent, as lacerations in 56 percent, as bruising in 30 percent, and as a “yellow area” in 17 percent. In approximately two-thirds of the cases, the diameter of the cervical erosion or the length of the laceration did not exceed 5 mm, and 80 percent of the lacerations involved only mucosa. Injury was more frequent in primiparas, in the anterior cervical lip, with occiput posterior positions, and with premature rupture of membranes. Residual cervical damage was reported in 8 percent of the 117 women in whom follow-up colposcopic examination was performed at 6–8 weeks.
Inspecting the lower birth canal and cervix after delivery is routine. Visualization of the full circumference of the cervix is often facilitated by applying suprapubic pressure, which elevates the uterus and concurrently causes the cervix to balloon into full vision. Commonly, cervical lacerations at both 3 and 9 o’clock are noted. An assistant and the use of right-angle retractors may facilitate exposure. Further visualization of the cervix is aided by the use of ring forceps to grasp the anterior and posterior lips of the cervix.
Significant lacerations are more common with an instrumental delivery, including midforceps or midvacuum delivery, and with intrauterine manipulation, such as that with the delivery of a second twin or a breech infant. Other clinical settings in which cervical injury is more common include tumultuous and precipitous labors. Cervical and/or vaginal lacerations, and even uterine rupture, should be suspected when bright-red bleeding persists despite good uterine tone.
On rare occasions, an edematous anterior cervical lip is caught between the fetal head and the symphysis pubis. If this is undetected, and the edematous lip cannot be manually reduced, lowered tissue perfusion in combination with repetitive pressure may result in ischemia sufficiently severe that the cervical lip undergoes necrosis and separation. Even more rarely, there may be an angular or circular detachment of the entire cervix. Remarkably, in such instances the blood supply has usually been compromised to the degree that there is no significant bleeding.
SURGICAL REPAIR
When bleeding necessitates surgical repair, adequate analgesia and surgical exposure are key. In the absence of bleeding, cervical lacerations usually are not repaired. The extent of the laceration must be identified and extension to involve the vaginal fornices. Important factors to consider in performing the repair include the possibility of extension with involvement of the descending branch of the uterine artery when lacerations extend above the vaginal fornix at either the 3 or 9 o’clock positions. Further assessment of the extent of the laceration may be obtained on bimanual examination. The possibility of injury to the uterine artery with development of a broad ligament hematoma should be considered and the patient observed for this development. Additionally, the proximity of the ureter to the area of surgical repair must be considered. The suture repair should be confined to the proximity of the cervix and not be swept laterally into the broad ligament.
If lacerations extending above the vaginal fornix are bleeding and need extensive repair, laparotomy may be required to achieve adequate exposure and to ensure that the ureter is not damaged. Insertion of a Foley catheter and the monitoring of urinary output, while reassuring, are not conclusive evidence that the ureter has not been incorporated into a repair. If there is any question about the possibility of ureteral damage, cys-toscopy should be performed and drainage of urine into the bladder from the involved ureter should be visualized and/or a stent passed into the ureter.
For surgical repair, right-angle retractors are inserted anteriorly, ring forceps are used to grasp the cervix posteriorly, and the cervix’s entire circumference is inspected. An assistant may be indispensable for adequate visualization. The vault of the vagina posteriorly and the lateral fornices are exposed by manipulating the cervix with ring forceps. Lacerations that are hidden behind the redundant cervix would accordingly be exposed (Fig. 12-1). The raw edges of the laceration can be approximated with interrupted absorbable sutures; each stitch is placed through the entire thickness of the cervix (Fig. 12-2). A 00 suture of chromic catgut, Dexon, or Vicryl is appropriate. The apex of a deep laceration may not be obvious if it lies above the vaginal vault. In such cases, beginning the closure of the laceration at the most distal portion and using each successive suture as a means of traction may facilitate visualization (Fig. 12-3). Unless the higher sutures can be placed accurately and safely above the upper end of the tear, a laparotomy should be considered because extensive bleeding can occur from an unligated vessel. If the decision is to observe the woman, then close attention to vital signs, urinary output, and the hematocrit is necessary. When the cervical laceration also extends onto the vagina, the vaginal laceration should be repaired in a similar fashion. Either interrupted sutures or a running-locking suture are appropriate.
FIGURE 12-1. Right-angle retractor and ring forceps are being used to visualize a cervical laceration in the posterior vaginal fornix. This laceration can be closed with either a running-locking suture or with interrupted sutures.
FIGURE 12-2. A laceration involving the 9 o’clock position of the cervix is shown. The anterior and posterior edges of the wound are well demonstrated with the use of ring or ovum forceps. Interrupted sutures are used for closure, with the suture incorporating the full thickness of the laceration.
FIGURE 12-3. A cervical laceration has extended into the lateral vaginal fornix. Successive interrupted sutures are placed with traction to progressively bring more of the laceration into the surgical field so that it can be repaired.
PUERPERAL HEMATOMAS
The first reported case of vulvovaginal hematoma is attributed to Rueff in 1554. When Lyons (1949) surveyed the literature some 400 years later, he found 188 cases, and only 12 years later Pedowitz and associates (1961) reported that 770 cases of vulvovaginal hematoma had been described.
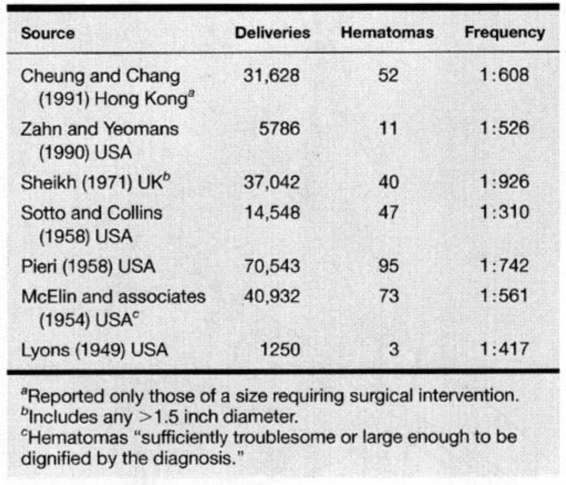
The reported frequency with which hematomas complicate delivery varies widely. Table 12-1 lists seven reports in which the frequency of hematomas varied from approximately 1 in 1000 to 1 in 300 deliveries. Importantly for comparisons, criteria used to define a hematoma varied widely. For example, Sotto and Collins (1958) described any hematoma greater than 1.5 inches in diameter, whereas Benrubi and colleagues (1987) multiplied cross-sectional diameters and reported those greater than 2.5 cm. Others used subjective criteria, including “those instances in our own practice wherein the hematomas were sufficiently troublesome or large enough to be dignified by diagnosis” (McElin and associates, 1954) and those “judged of a size sufficient to require surgical intervention” (Sheikh, 1971; Zahn and Yeomans, 1990). Accordingly, any interpretation of these data will be limited by the lack of a standardized definition for vulvovaginal hematomas.
TABLE 12-1. Frequency of Vulvovaginal and Supravaginal Hematomas
CLASSIFICATION
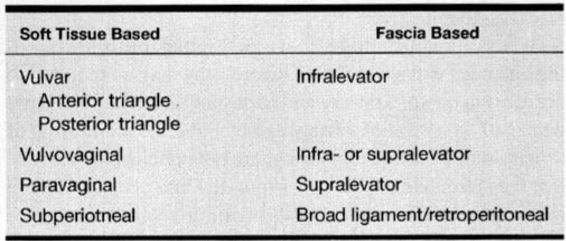
Table 12-2 presents the most commonly used classification system for genital tract hematomas. Hematomas are designated as vulvar, vulvovaginal, paravaginal, and subperitoneal. In this system, a combination of visual inspection and palpation is used to localize the predominant position of the hematoma.
TABLE 12-2. Commonly Employed Classification Systems for Genital Tract Hematomas
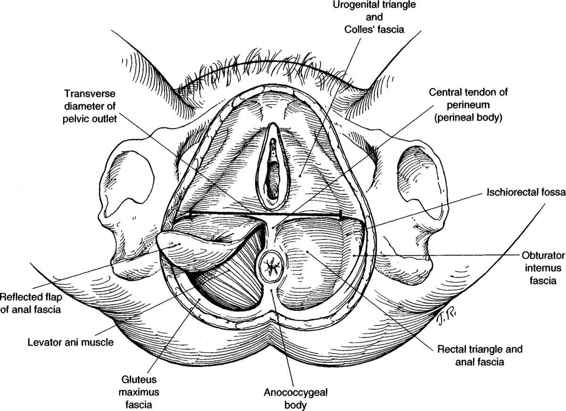
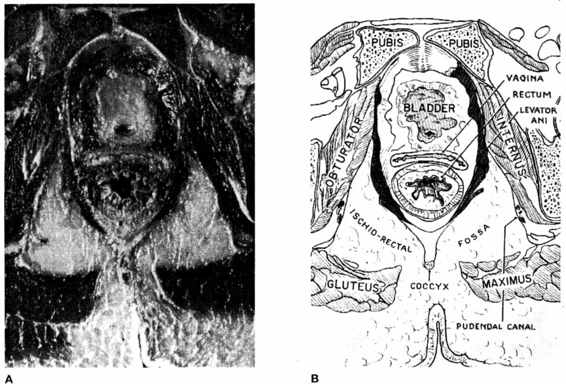
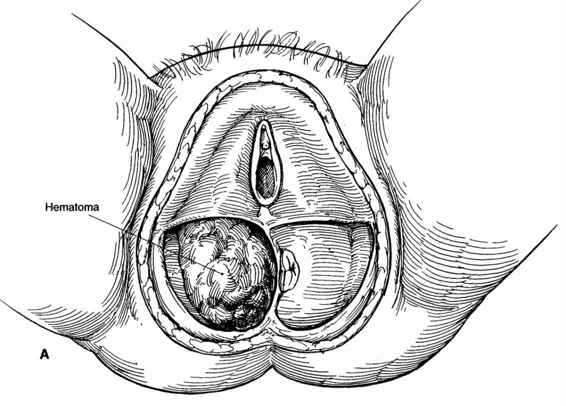
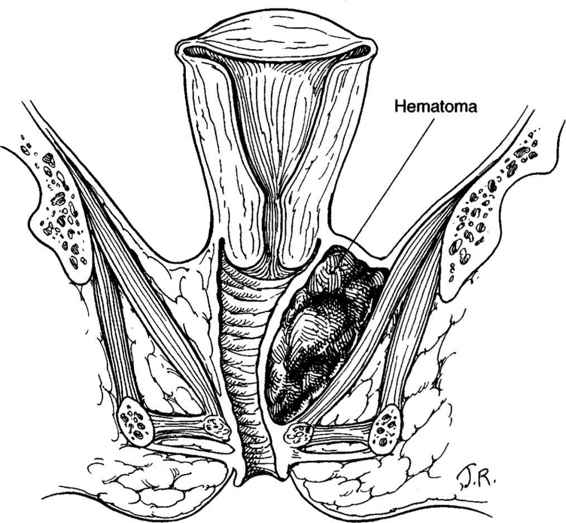
VULVAR HEMATOMAS. These hematomas are subdivided into those located in the anterior and posterior triangles. The central tendon of the perineum prevents these hematomas from spreading across the midline (Fig. 12-4). Using an alternate classification system based on the levator muscle, vulvar hematomas are infralevator in location. Their extension is limited superiorly by the levator ani muscle and they are limited from spread onto the thigh by Colles’ fascia and the fascia lata. Vulvar hematomas involving the posterior triangle may dissect into the ischiorectal fossa, where considerable blood can accumulate quickly (Fig. 12-5). Shown in Figures 12-6A and B are sagittal and coronal representations of such a hematoma, demonstrating both the fascial limitations to spread of the hematoma and the large potential space of the ischiorectal fossa and buttock within which the hematoma can accumulate.
FIGURE 12-4. Dissection of the female perineum with the integument and superficial fascia removed. The fat has also been removed from the ischiorectal fossa in this diagram.
FIGURE 12-5. Female pelvis on horizontal section with accompanying diagram to show muscle groups, bone, and potential spaces. (Courtesy of Grant, 1962, with permission.)
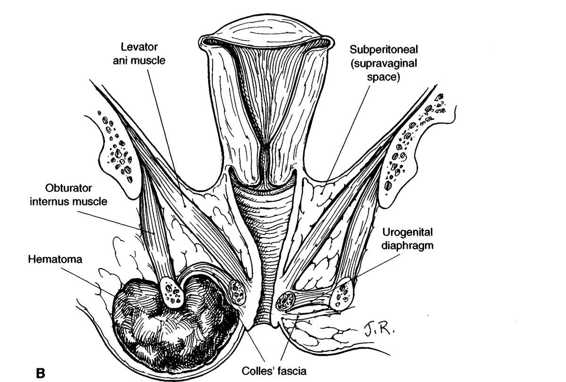
FIGURE 12-6. A. Infralevator hematoma in rectal triangle. B. Coronal section through hematoma illustrating its relationship to adjacent structures.
VULVOVAGINAL HEMATOMAS. These hematomas involve the vulva and the lower vagina. They are most commonly associated with either a mediolateral episiotomy or a spontaneous lateral vaginal wall tear with extension into the perineal body. Vulvovaginal hematomas also may complicate midline episiotomies. On visual inspection, it is not always possible to determine whether there has been supralevator extension of the hematoma from a cut or tear of the levator plate, or whether there is simply displacement of the levator plate by the most cephalad extension of the hematoma. In contrast, the paravaginal hematoma is clearly a supralevator hematoma that occupies the middle to upper portion of the vagina (Fig. 12-7).
FIGURE 12-7. Coronal section through a paravaginal or supralevator hematoma.
SUBPERITONEAL HEMATOMAS. These also are known as supravaginal or retroperitoneal hematomas. They are above the cardinal ligaments and may extensively involve the broad ligament with continued retroperitoneal dissection to the level of the kidneys or even higher. These hematomas can result in significant hemorrhage and may also rupture into the abdominal cavity. While the current outlook for sub-peritoneal hematomas is much better than the 75 percent mortality rate Lyons (1949) reported, there are still maternal deaths from these complications.
ETIOLOGY AND RISK FACTORS
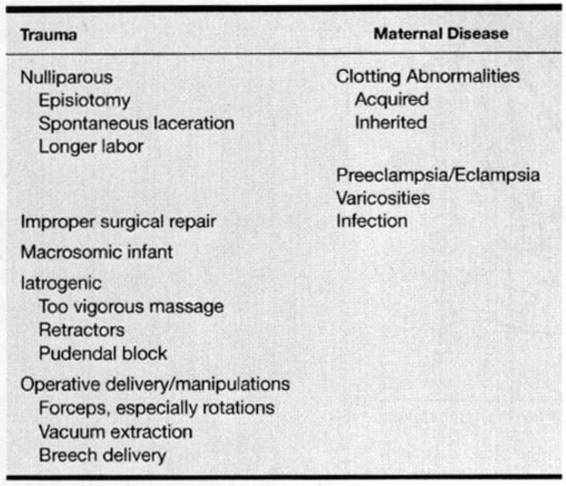
The development of puerperal hematomas is associated with several factors that can be divided into broad categories of maternal trauma or maternal factors that may predispose to hematoma formation (Table 12-3). Ridgway (1995) found that nulliparity, episiotomy, and forceps delivery are the most common risk factors. Indeed, 50–75 percent of these hematomas are reported in nulliparous women (Propst and Thorp, 1998; Zahn and Yeomans, 1990). McElin and colleagues (1954) reported an episiotomy, predominantly left mediolateral, in 93 percent of women who subsequently developed hematomas. Similarly, an episiotomy—usually midline—was performed in all women with hematomas reported by Zahn and Yeomans (1990). These latter authors also described frequent use of forceps and concurrent vaginal sidewall lacerations in a third of their patients. While Sheikh (1971) reported associated episiotomies in only half of women developing hematomas, another third sustained a spontaneous laceration without an episiotomy. Almost 20 percent of his patients developed a significant hematoma despite delivery over an intact perineum. It is also important to remember that 40–65 percent of women who develop a genital hematoma do so following spontaneous vaginal delivery (Pedowitz and colleagues, 1961; Sheikh, 1971; Benrubi and associates, 1987). Other reported risk factors for puerperal hematomas include preeclampsia (30 percent), multifetal pregnancies (15 percent), and breech delivery (10–15 percent).
TABLE 12-3. Risk Factors Associated with Puerperal Hematomas
VESSEL INJURY
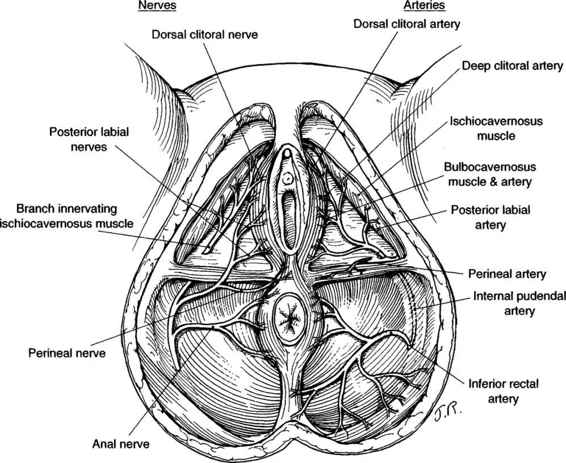
Injured vessels that most commonly cause vulvar hematomas are branches of the pudendal artery: inferior rectal, transverse perineal, and posterior labial arteries (Fig. 12-8). Some vaginal hematomas involve the descending branch of the uterine artery. Subperitoneal hematomas may be associated with the uterine artery and its branches as well as other vessels in the broad ligament (Walsh and Ganser, 1948).
FIGURE 12-8. The arteries and nerves of the pelvic floor as seen from below demonstrating the branching of the internal pudendal artery and the pudendal nerve.
CLINICAL PRESENTATION
Diagnosis and classification of vulvar and vaginal hematomas involves inspection and palpation. Attention is usually first called to the hematoma by the woman herself when she complains of severe perineal pain that is not relieved by analgesics. Unfortunately, the pain is too often attributed to the episiotomy and a hematoma is missed early. Blood loss is almost always underestimated with puerperal hematomas (Sheikh, 1971; Scudamore, 1964). The severity of associated anemia depends on the magnitude and rapidity
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree