Nail bed repair tips and tricks
Suture recommendations
5-0 or 6-0 Chromic; a spatulated needle may help pass through the nail bed tissue
Permanent sutures are to be avoided as removal can be painful
Suturing recommendations
Follow the curve of the needle – failure to do so will tear the nail bed
Simple sutures (no mattress)
Single passes with the needle are encouraged to avoid tearing the nail bed
Linear lacerations
Primary suture or glue repair
Stellate lacerations
Glue repair may be easier and less traumatic to the nail bed
Nail bed tissue loss
Look at underside of nail plate. If nail bed remnant is adherent to removed nail plate, it can be used as a graft
Split graft from intact nail bed (from the same digit) can be used in the acute setting for sterile matrix loss
The cyanoacrylate has been shown to offer significant time savings with clinical outcomes comparable to suture repair (Strauss et al. 2008). If the nail plate is completely avulsed, any visible nail bed laceration should be repaired with either a fine absorbable suture or glue as described above. If there is associated loss of matrix substance that cannot be repaired primarily, the clinician should first examine the underside of the avulsed nail plate. If nail bed portions are identified adherent to the avulsed nail plate, the plate can be repositioned on the nail bed as a “composite graft” aligning the nail such that the missing matrix segments are replaced in their anatomic position (Tos et al. 2012). If no nail bed graft is readily available to replace lost matrix substance, the surgeon can harvest graft from either a spare part, the injured digit, or a toe. Sterile matrix loss can be replaced with split matrix grafts. A split graft can be harvested from either intact sterile matrix of the injured digit or of an adjacent digit. Split grafts offer the advantage of replacing lost tissue without significant donor site morbidity or donor nail deformity. The split graft is harvested by removing the nail plate and shaving a portion of the sterile matrix with a sharp no. 15 blade. The graft should be thin enough so the blade can be visualized through the graft. No repair of the donor site is needed.
Split grafts however cannot be used to reconstruct lost germinal matrix, which requires the growth potential afforded only by a full thickness nail bed graft (or vascularized toe flap). As would be expected such a graft would cause an obvious donor nail deformity, and thus, these grafts should come from either a spare part (e.g., an amputated digit) or a digit that is easily concealed (e.g., a toe). Split and full thickness grafts can be applied directly to the exposed distal phalanx (Brown et al. 1999).
If the nail plate remains intact after a significant crush injury, the clinician will often see a subungual hematoma . Invariably, the hematoma is reflective of an underlying nail bed injury. Controversy exists as to how to best treat subungual hematomas. If the hematoma is small and there is no associated fracture, simple trephination of the nail plate will allow hematoma evacuation, pressure reduction, and pain relief. Trephination can be performed with a heated paper clip or a battery-powered cautery. If the hematoma is large (traditionally cited as >25 % of the surface of the nail plate), some authors recommend nail plate removal and direct repair of the nail bed laceration. This has not been shown to be better however to simple trephination or observation – even when distal phalanx fractures are present (Gellman 2009; Roser and Gellman 1999). In the setting of contamination or if there is displacement of the underlying distal phalanx fracture, removal of the nail plate is indicated to allow irrigation, debridement, and direct repair of the nail bed and to assist with fracture reduction as needed.
The Seymour Fracture
The distal phalanx physis in the skeletally immature patient represents a potential fault line that can fail in the setting of crush or force loading injuries. Given the radiolucent nature of the physis, radiographic findings of physeal fractures can be subtle. The clinician must therefore have a high index of suspicion for this particular fracture pattern when evaluating the pediatric patient with a fingertip injury (Abzug and Kozin 2013; Krusche-Mandl et al. 2013). Clinically, the patient will often present with a partial avulsion of the proximal nail plate through the eponychial fold. The digit may have a “mallet” appearance. Radiographically, the physis will look wide compared to physes of adjacent, uninjured digits, and there may be displacement of the distal phalanx diaphysis in the dorsopalmar plane (Fig. 1a–d).


Fig. 1
Seymour fracture. (a) Clinical appearance of proximal nail bed entrapped in fracture. (b) Clinical appearance of proximal nail bed freed from fracture. (c) Radiograph demonstrating classic Seymour fracture through open physis. (d) Radiograph demonstrating reduction of fracture and stabilization with a percutaneous wire
When the fracture is displaced, it often tears the proximal nail bed and therefore becomes exposed to the environment. It should thus be considered an open fracture. The nail bed can become interposed between the fracture fragments and prevent reduction. Failure to recognize the injury pattern and reduce the fracture in a timely manner can result in permanent nail deformity, permanent growth disturbance, and osteomyelitis. Removal of the avulsed nail plate will immediately reveal the associated nail bed injury. If the nail bed is interposed between the fracture fragments, it should be withdrawn. The fracture can then be reduced and stabilized with a smooth Kirschner wire. The nail bed laceration should then be repaired.
Operative Treatment of Nail Bed Injuries
Many of these procedures can be done in the emergency room setting under local anesthesia with IV sedation, especially in older children. Lidocaine with epinephrine (1 % Lidocaine with epinephrine 1:100,000) has been proven safe at the digital level and may preclude the need for a digital tourniquet (Lalonde 2011; Lalonde and Martin 2013). The patient is placed supine with the injured extremity on a hand table. After a sensory examination has been performed in age-appropriate children, the digit is anesthetized. If epinephrine has not been used, a finger tourniquet should be applied to the base of the digit to provide a bloodless operative field. The nail plate can be removed by passing a Freer Elevator directly under the volar surface of the nail. Care should be taken to angle the elevator toward the nail plate and not toward the nail bed – this will minimize iatrogenic injury to the nail bed. The lateral nail edges should be freed from the lateral nail folds also with the elevator. Once the nail has been mobilized from its attachments to the nail bed and lateral nail fold s, a small clamp should be attached to the lateral aspect of the nail plate and then turned multiple times like “twisting spaghetti on a fork.” This maneuver will allow the nail to roll out from under the dorsal nail fold. The underlying nail bed should now be visible (Fig. 2a). Any gross contamination, bone devoid of an adequate soft tissue envelope, or clearly necrotic tissue should be debrided.
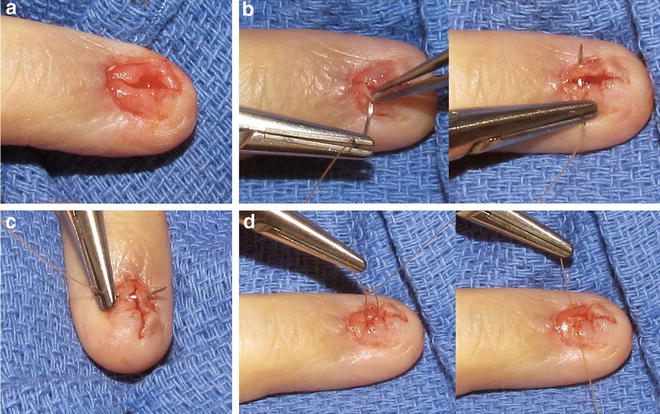
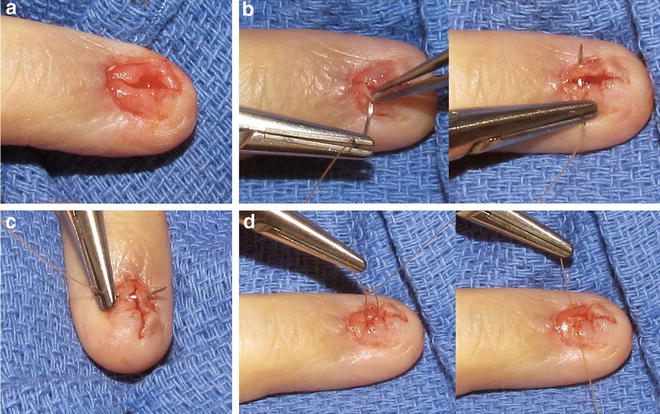
Fig. 2




Nail bed repair with suture. (a) A longitudinal nail bed injury through the sterile matrix. (b) A demonstration of nail bed repair with one suture pass following the curve of the needle. (c) A demonstration of nail bed repair with one suture pass following the curve of the needle. (d) A demonstration of completing the suture by tying a square knot without tearing the nail bed
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


