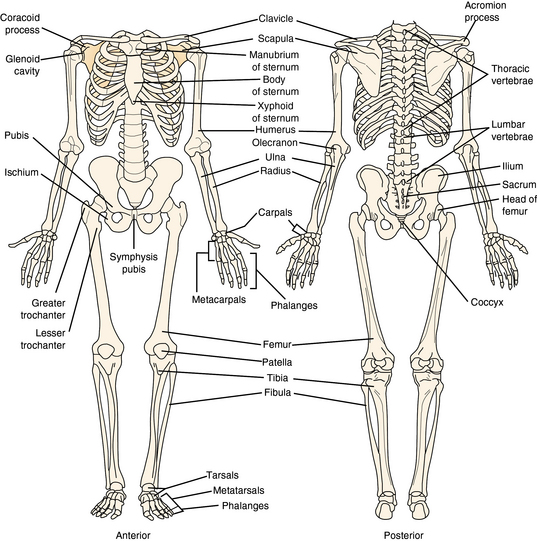
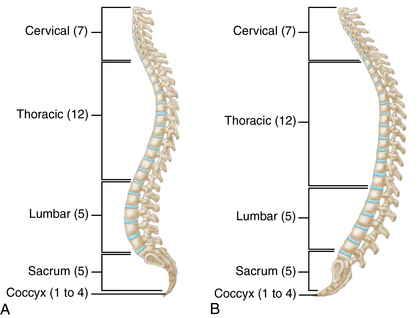
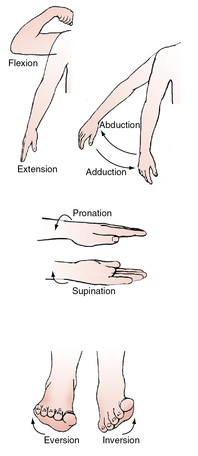
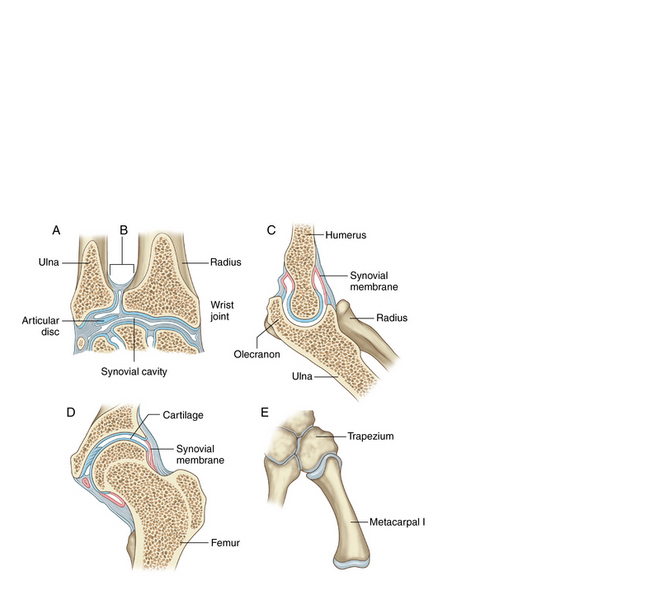
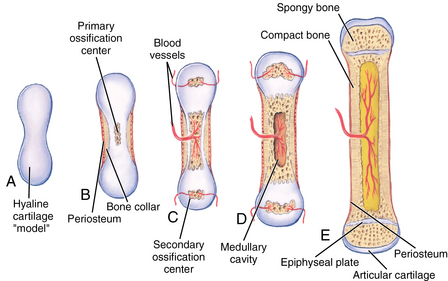
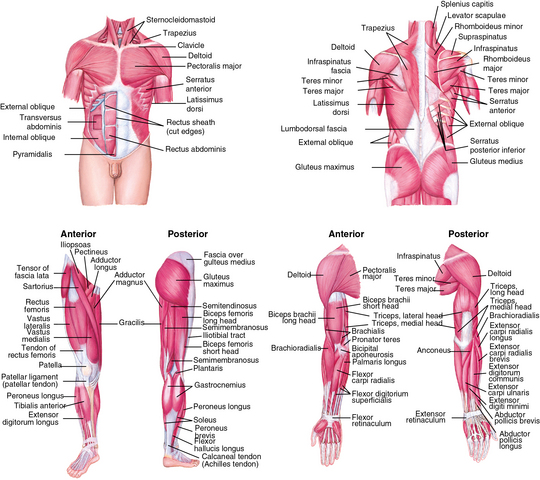
CHAPTER 18 The rudimentary skeletal system forms as early as the fourth week of gestation when the development of the vertebrae begins and the upper extremities begin as buds on the fetus. As early as the seventh week of gestation, embryonic vascular growth progresses toward the center of the osteoblasts in the long bone, which forms cartilage. During the ninth week of gestation, ossification, or bone growth, begins in the ossification centers in the lower thoracic and upper lumbar vertebrae, and ossification continues in the femur. The hand pads develop from the extremity buds by days 33 to 36, and the finger rays begin to form on days 41 to 43.1 It is during this period of gestation that polydactyly, the presence of extra digits, or syndactyly, the webbing or fusing of the digits, occurs along with other deformities of the extremities. The calcaneus, the largest tarsal bone of the foot, ossifies at the sixth month of fetal life. The position of the fetus in utero has the greatest impact on the skeletal system and the most common variants present at birth. At birth, the epiphyses of the long bone are composed of hyaline cartilage. Shortly after birth, the secondary ossification centers begin to replace the cartilage along the epiphyseal plate. During early periods of rapid growth, ossification occurs in secondary sites throughout the body: the ends of the long bones, the vertebrae, the flat bones in the clavicle, and the skull. The replacement of cartilage by bone is known as endochondral ossification. The epiphyseal plate ossifies, becoming the diaphysis, the shaft of the long bone; and cartilage at the metaphyseal plate replaces bone cells (Figure 18-1). FIGURE 18-1 Growth plates and transition from cartilage to bone at the epiphyseal plate. A, Hyaline cartilage “model.” B, Periosteum and bone collar form. C, Blood vessels and osteoblasts infiltrate primary ossification centers. D, Osteoclasts form medullary cavity. E, Ossification is complete. Hyaline cartilage remains as articular cartilage and in the epiphyseal plate. (From Applegate E: The anatomy and physiology learning system, ed 4, St. Louis, 2011, Saunders.) Several factors influence the health of the bones and growth of cells at the epiphyseal plate. Trauma during childhood can cause separation of the epiphysis and the blood vessels to rupture, resulting in cessation of bone growth and a shortened extremity.1 Nutritional factors such as adequate protein in the diet, the amount of calcium intake, and adequate intake of vitamin D, particularly in breastfed infants, impact bone growth. Vitamin D absorbs dietary calcium and phosphorus from the intestines and promotes bone health by maintaining normal levels of these minerals in the blood. Adequate levels of vitamin D in childhood may also have a role in improving muscle and immune function. Parents are often advised to keep infants and children out of the sun due to long-term risks of skin cancer, therefore reducing vitamin D synthesis from the skin. Maintaining adequate levels of vitamin D in infants and children is important to maintaining bone strength. Rickets is a deficiency of vitamin D in which the growth plate is impaired by calcification of newly formed bone on the metaphyseal plate. Alterations in thyroid or growth hormones can also impact normal growth.1 Recent evidence indicates environmental and chemical hazards may be a contributing factor to malformations in the musculoskeletal system. The clavicle lies in a horizontal plane above the first rib and rotates between the sternum and the superior surface of the scapula (Figure 18-2). The scapula, a large, flat triangular bone, forms the posterior portion of the upper extremity and the superior, lateral angle articulates with the capsule or rounded head of the humerus, the large bone in the upper arm. The distal end of the humerus forms the condyle and is divided into the medial epicondyle and the lateral epicondyle. The proximal end of the ulna attaches at the articulating surface of the humerus and forms one of two long bones in the forearm. The olecranon is the outer, rounded distal surface of the ulna and forms the major portion of the elbow. The distal end of the ulna is small and articulates with the wrist bones. The radius is along the lateral side or thumb side of the forearm, and the distal end of the radius forms a large portion of the wrist bones. The hand consists of eight carpal and five metacarpal bones. Many of the carpal bones are cartilaginous at birth. A radiograph of a child’s hand at 2½ years of age illustrates ossification of only the capitate and hamate bones in the hand. Development and ossification of the hand continues until 11 years of age when all of the carpal bones are ossified except for the small pisiform bone, which develops by 12 years of age. Abnormalities of the phalanges, or fingers, such as syndactyly, webbing, or fusion between adjacent digits of the hands or feet, may be indicative of profound developmental delay (Figure 18-3). Polydactyly, the presence of supernumerary digits, is a more common variant and is not usually associated with other congenital anomalies. FIGURE 18-3 A, Syndactyly. B, Polydactyly. (A, From Davis P, Cladis F, Motoyana E: Smith’s anesthesia for infants and children, ed 8, Philadelphia, 2012, Mosby. B, From Valiathan A, Sivakumar A, Marianayagam D, et al: Thurston syndrome: report of a new case, Oral Surg Oral Med Oral Pathol Oral Radiol Endod 101(6):757-760, 2006.) The infant has a C-shaped spinal curve at birth in comparison to the double S curvature that is present in late adolescence. Thoracic and pelvic curves are present at birth, and the secondary cervical curve is present by 3 to 4 months of age when the infant begins to hold up his or her head. The lumbar curvature begins to form as the infant bears weight and begins to walk. The young child often has an exaggerated thoracic-lumbar curvature and a protuberant abdomen until 3 years of age, when gait and balance become more normal (Figure 18-4). The sacrum is composed of five separate bones at birth and by 18 to 20 years of age is fused into one large bone. The coccyx consists of three or four small bones that begin to ossify between the first and fourth years of life and fuses into one bone by 25 years of age (Figure 18-5). FIGURE 18-4 Protuberant abdomen of the young child. (From Seidel H, Ball J, Dains J, et al: Mosby’s guide to physical examination, ed 7, St. Louis, 2011, Mosby.) The patella is the small triangular bone that forms the kneecap and lies over the junction of the femur and the tibia. The health of the patella during growth and development depends not only on strong bone growth but also on the strength of the ligaments and tendons supporting the patella. Monitoring the velocity of growth is the key focus of routine well-child visits and when following children with chronic health conditions. For the child with slow growth or delayed onset of puberty, obtaining past growth charts and evaluating the progression of the growth curve along with familial patterns of growth and pubertal development is critical to assessing an abnormal growth pattern. The rate of muscle growth and development increases rapidly beginning at age 2 years. Early muscle growth is balanced by a normal decrease in adipose tissue in early childhood.1 The growth and maturation of the muscles continues with the ossification of the skeletal system (Figure 18-6). Muscle tone is the state of normal tension of the muscles, and term infants normally have strong muscle tone at birth. Abnormalities in muscle tone in an infant may be noted shortly after birth when an infant is floppy. Less than normal muscle tone is described as hypotonia; rigidity or increased muscle tone is known as hypertonia; and spasticity is resistance to flexion and extension and range of motion of the muscles. Normal muscle function requires the normal function of the lower motor neurons (LMNs) in the spinal cord and the normal reflexivity of the muscle fibers. Normal muscle tone requires the normal function of the spinal cord stretch reflex and the balance of the upper motor neurons (UMNs) and LMN function. Lesions on the UMNs result in increased tone and LMN lesions result in decreased tone. FIGURE 18-6 Muscular system, front and back. (From Mourad LA: Orthopedic disorders, St. Louis, 1991, Mosby.) The greatest increase in muscle size occurs during puberty when boys’ muscle mass and muscle cell size begins to exceed that in girls. In early and middle childhood, girls’ muscle size increases at a greater rate than in boys up until puberty. Table 18-1 presents physiological and developmental changes in the musculoskeletal system from the newborn through adolescence. TABLE 18-1 Physiological Variations of the Musculoskeletal System at Key Developmental Stages Obtaining a complete history or a symptom-related history of the musculoskeletal system is key to accurate assessment in children and adolescents. The Information Gathering table reviews the pertinent areas for each age-group and developmental stage of childhood. Information Gathering for Assessment of the Musculoskeletal System at Key Developmental Stages For a thorough and complete assessment of the musculoskeletal system, infants must be undressed except for the diaper, and children must be undressed except for underwear. A young child cannot be thoroughly assessed when wearing socks and shoes or when gowned. In preadolescence and adolescence, maintaining modesty while assessing the spine can be challenging, particularly in girls. Maturing females must be in underwear and gown to obtain a thorough examination of the spine. Musculoskeletal terminology is presented in Box 18-1, and skeletal positions are presented in Figure 18-7. Initial inspection of the musculoskeletal system in the child from birth to adolescence begins with inspection of skin for color and temperature; inspection of palmar creases; and noting of scars, unusual pigmentation or lesions, swelling, and bruising. Bruising is the most common sign of physical abuse and intentional injury in children. Bruising over bony prominences such as the shins, knees, and forehead are common in children and usually the result of active play. However, bruising seen on the buttocks, neck, face, and earlobes should be considered suspect and require further information gathering and assessment for signs of abuse.2 Erythema, swelling, tenderness, or temperature changes should also be noted over the joints or extremities. Joints in the body have a slightly moveable to freely moveable motion throughout the period of growth and development. The hinge joint, between the humerus and the ulna, permits motion in one plane, whereas the pivotal joint, between the radial-ulnar joint, allows rotation only. The condyloid joint in the wrist allows flexion, extension, adduction, abduction, and circumduction. Saddle joints, such as in the thumb, have a similar motion to the condyloid joint in the wrist except that the joint forms a concave-convex fit to achieve motion. The hip and shoulder joints are examples of ball-and-socket joints. Finally, the gliding joints allow a gliding motion between two flat surfaces, such as in the vertebrae and carpal joints in the hands and feet (Figure 18-8). Range of motion should be passively evaluated in infants and young children and assessed actively when children are cooperative with examination. Any limitation of range of motion in joints and extremities or asymmetrical response should be further investigated. Muscle tone and strength should also be evaluated. In early childhood, the radial-ulnar joint is particularly vulnerable. Subluxation, or partial dislocation, of the radius from the humerus, often referred to as Nursemaid’s elbow, is common in children from 2 to 4 years of age. Often there is no clear history of trauma, but laxity of the ligaments in the young child predisposes them to injury. In cases of a subluxation, the child usually refuses to use the affected arm. Passive range of motion is possible except for supination (palm facing upward). Dislocation of the shoulder can also occur in the young child and is marked by swelling, pain, and a limp arm. Trauma to the upper extremities is common in children and adolescents. Strains, sprains, or fractures can occur with strenuous activity, falls, motor vehicle or pedestrian injuries, or participation in competitive sports. Careful assessment is warranted in the growing child when any history of trauma is obtained. Fractures that are highly suggestive of intentional injury or abuse in children are rib fractures, especially posterior rib fractures, scapular fractures, sternal fractures, fractures of the spinous processes, and metaphyseal lesions.2 Clavicular fractures and long bone fractures in children older than 1 year of age are common traumatic injuries of childhood.
Musculoskeletal system
Embryological development
Developmental variations
Anatomy and physiology
Upper extremities and torso


Spine

Lower extremities and feet
Monitoring growth
Muscle development
Physiological variations
Age-Group
Variation
Preterm infant and newborn
Lower extremities in external rotation and flexion at hips; upper femur is anteverted and knees are flexed; tibias are internally rotated; feet are dorsiflexed
Infancy
Tibias gradually rotate externally to about 20 degrees toward midline by 12 months of age; flat feet and bowed legs until walking is firmly established
Early childhood
Stance with wide base of support, hyperflexion of hips and knees with disjointed (toddling) pattern when walking; arms held abducted and elbows extended; in-toeing is common beginning at 15 months; normal arm swing and heel-toe walking generally begin by 18 months of age; longitudinal arch not present in infant but begins to develop by 2½ years of age. At 3 years of age, children exhibit mature pattern of motion and muscle action; resolution of in-toeing and marked torsion of lower extremities normally disappear by school entry
Middle childhood
Knock-knee is present until 7 years of age; by 8 to 10 years of age, femur rotates to position of about 14 degrees toward midline from average of 45 degrees at birth
Adolescence
Hormonal changes impact ligaments and tendons; laxity of knees is particularly common in adolescent females, making them vulnerable to injury
System-specific history
Age-Group
Questions to Ask
Preterm infant
History of hypoxia in early neonatal period? Intraventricular insult? Any maternal alcohol or substance abuse? When did prenatal care begin?
Newborn
History of maternal infection while in utero? Any trauma sustained at birth? Need for resuscitation or ventilation in immediate newborn period? Presentation at birth? Breech or shoulder? Family history of skeletal deformities or genetic disorders?
Infancy
Family history of bone or joint disorders? Any delay in achieving gross motor milestones? Does infant roll over? Sit without support? Crawl? Stand alone? Walk without support? Any evidence of toe-walking? Any evidence of widening of wrist joints?
Middle childhood
Involved in organized/competitive sports? Any complaint of pain when walking/running or pain that awakens child at night? History of joint stiffness or swelling? Weight of school backpack? History of prolonged steroid use with chronic conditions?
Adolescence
Involved in organized/competitive sports? Any limited range of motion of joints? Is gait normal and erect? History of fractures, sprains, or trauma? Weight of school backpack? Any evidence of habitual slouching? Family history of skeletal deformities? Start of menstrual periods?
Environmental risks
Contact with chemical cleaning agents, hazardous smoke, or chemicals? Exposure to toxic pesticides? History of elevated lead level?
Physical assessment
Preparation for the examination
Inspection and palpation
Joints
Upper extremities and clavicle
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Musculoskeletal system
Only gold members can continue reading. Log In or Register to continue