Multiple Pulmonary Nodules
Eva Ilse Rubio, MD
DIFFERENTIAL DIAGNOSIS
Common
Fungal Infection
Mycoplasma Infection
Less Common
Tuberculosis (TB)
Viral Infection
Septic Emboli
Metastatic Disease
Lymphoproliferative Disease
Post-Transplant Lymphoproliferative Disorder
Langerhans Cell Histiocytosis, Pulmonary
Wegener Granulomatosis
Sarcoid
Rare but Important
Hypersensitivity Pneumonitis
Thoracic Lymphoma
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Location within pulmonary parenchyma
Centrilobular vs. random
Upper vs. lower lobe predominant
Tendency to present as cavitary lesions
Septic emboli, Aspergillus, Wegener, papillomatosis
Patient demographic/clinical considerations
High risk TB population?
Regional endemic fungal infections?
Immunocompromised patient?
Many primary neoplasms metastasize to lungs; usually there is known primary when lung metastases are detected
Helpful Clues for Common Diagnoses
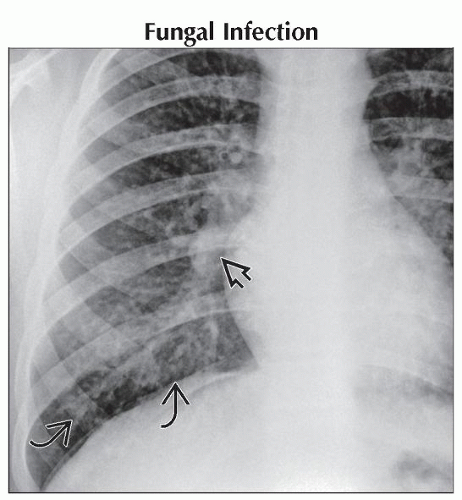
Fungal Infection
Histoplasmosis
Common in midwestern USA
Variable appearance: Multiple nodules, alveolar, ill-defined peripheral opacities
Coarsely calcified mediastinal/hilar lymph nodes are common
Pulmonary nodules often calcify
Candida
Typically seen in patients with multiple underlying medical conditions
Variable parenchymal pattern: Nodules, segmental consolidation, ± cavitation
Look for other systemic disease: Spleen, liver, bloodstream, sinuses
Aspergillus
Allergic: Typically seen in asthma or cystic fibrosis patients; ill-defined consolidation or branching mucoid plugs
Saprophytic: Preexisting architectural abnormality (bronchiectasis, cavity); classic fungus ball
Mildly invasive: Chronically ill patients; focal infiltrate or fungus ball in cavity
Frankly invasive: Immunocompromised patients; variable appearance of peripheral consolidation, “halo” sign, cavitary lesions
Coccidiomycosis
Imaging appearance compared to TB
Highly variable appearance: Nodules, infiltrates, or thin-walled cavities
Pleural effusions, adenopathy possible
Blastomycosis
Rare in children
More severe infection/multiorgan involvement if immunocompromised
Variable pattern: Nodules, peripheral consolidation, interstitial opacities
Mycoplasma Infection
Wide spectrum of radiologic and clinical presentations
May manifest as bronchopneumonia, atelectasis, or interstitial opacities
Typical in older school-aged children
Helpful Clues for Less Common Diagnoses
Tuberculosis (TB)
Secondary tuberculosis may present as diffuse bilateral < 3 mm nodular opacities
May be associated with pleural effusions, lymphadenopathy
Consider concomitant solid visceral or CNS involvement
Viral Infection
Cytomegalovirus
Typically seen after bone marrow transplant
Bilateral, diffusely distributed, small nodular opacities
Human papillomavirus
Endobronchial spread of laryngeal papillomatosis
Bilateral nodules of varying size, may cavitate
Septic Emboli
Common organisms: Staphylococcus aureus, Streptococcus
Search for underlying source: Soft tissue infection, osteomyelitis, central line infection, endocarditis
Imaging
Multiple, basilar-predominant, nodular or ill-defined opacities
Eventual cavitation common
Source vessel may be identified
Metastatic Disease
Wilms tumor
Lungs are most common site of mets
Pulmonary: Multiple pulmonary nodules, masses
Cardiovascular: Tumor extension into renal vein, IVC, right atrium
Ewing sarcoma
Lungs are most common site of metastatic disease; metastases may be seen at diagnosis or years later
Rhabdomyosarcoma
Common tumor in children arising from GU tract, orbits, chest wall
Lungs are most common site of metastatic disease
Osteosarcoma
Most common malignant bone tumor in children
Lungs are most common site of metastases: Nodules that may be ossified; spontaneous pneumothorax; hemothorax
Lymphoproliferative Disease, Post-Transplant Lymphoproliferative Disorder
Variable appearance: Infiltrates or nodules
Hilar/mediastinal adenopathy may be seen
Langerhans Cell Histiocytosis, Pulmonary
Parenchymal findings: Nodule that cavitates; thick- or thin-walled cysts
Other thoracic features: Pneumothorax, adenopathy, fibrosis
Wegener Granulomatosis
Vasculitis, cavitating nodules (basilar predominant), ± ground-glass halo
Other respiratory/thoracic manifestations: Rhinorrhea, epistaxis, mucosal ulcerations, airway stenosis, pleural effusions, pulmonary hemorrhage
Other visceral manifestations: Glomerulonephritis, splenic lesions
Sarcoid
Pulmonary: Small reticulonodular opacities
Thoracic: Hilar, paratracheal adenopathy
Helpful Clues for Rare Diagnoses
Hypersensitivity Pneumonitis
Variable pattern of fine nodules, alveolar or interstitial opacities
Thoracic Lymphoma
Pulmonary nodules more common in Hodgkin vs. non-Hodgkin
Typically seen with mediastinal/hilar adenopathy
Variable pattern of round nodules or ill-defined opacities
Image Gallery
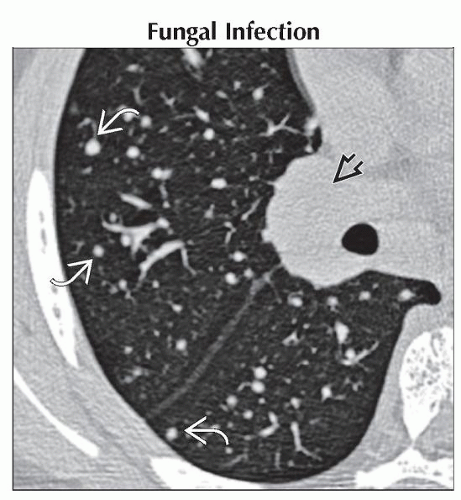 Axial CECT in the same patient shows the typical appearance of the small pulmonary nodules
 at the lung base. Bulky right hilar adenopathy at the lung base. Bulky right hilar adenopathy  is redemonstrated. is redemonstrated.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|