Monozygotic (MZ) twins result from mitotic division of a single zygote into ‘identical’ twins. Whether they share the same amnion or placenta depends on the time at which division into separate zygotes occurred (Fig. 27.1). Division before day 3 (approx. 30%) leads to twins with separate placentas and amnions (dichorionic diamniotic [DCDA]). Division between days 4 and 8 (approx. 70%) leads to twins with a shared placenta but separate amnions (monochorionic diamniotic [MCDA]). Later division (9–13 days) is very rare and causes twins with a shared placenta and a single amniotic sac (monochorionic monoamniotic [MCMA]). Incomplete division leads to conjoined twins. Monochorionic (MC) twins have a higher fetal loss rate, particularly before 24 weeks.
Aetiology
Assisted conception, genetic factors and increasing maternal age and parity are the most important factors, largely affecting DZ twinning. About 20% of all in vitro fertilization (IVF) [→ p.92] conceptions and 5–10% of clomiphene-assisted conceptions are multiple. Embryo transfer of more than two fertilized ova at IVF is now performed in the UK only under exceptional circumstances.
Diagnosis
Vomiting may be more marked in early pregnancy. The uterus is larger than expected from the dates and palpable before 12 weeks. Later in pregnancy, three or more fetal poles may be felt. Many are diagnosed only at ultrasound: as this is now performed in most pregnancies, the diagnosis is seldom missed.
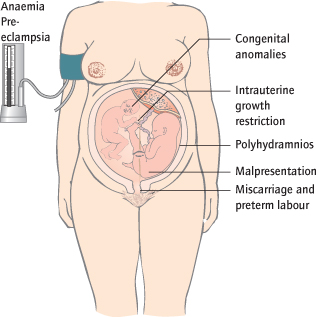
Antepartum Complications
Virtually all obstetric risks are exaggerated in multiple pregnancies (Fig. 27.2).
Maternal
Gestational diabetes and pre-eclampsia particularly are more frequent. Anaemia is common, partly because of a greater increase in blood volume causing a dilutional effect and partly because more iron and folic acid are needed.
Fetal
Twins have greater mortality (6-fold increase) and long-term handicap (5-fold increase). Triplets fare even worse with an 18-fold increase in handicap. The major risk factors are preterm delivery, intrauterine growth restriction (IUGR) and monochorionicity (see below).
All Multiples
Miscarriage:
One of a twin or more of a higher multiple pregnancy can ‘vanish’, where there is first trimester death. Late miscarriage is also more common, particularly in MC twins as a complication of twin–twin transfusion syndrome (see below).
Preterm labour is the main cause of perinatal mortality: 40% of twin and 80% of triplet pregnancies deliver before 36 weeks; 10% of twins deliver before 32 weeks.
Intrauterine growth restriction (IUGR) (Fig. 27.3) is much more common.
Congenital abnormalities are not more common per baby in dichorionic, but they are in monochorionic pregnancies.
Co-Twin Death:
If one of a pair of DC twins dies, the other usually survives, although the risk of preterm delivery is increased.
Complications of Monochorionicity
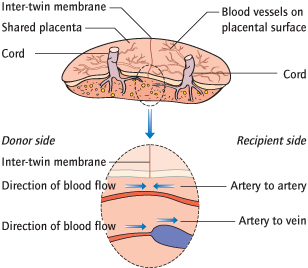
These largely result from the shared blood supply in the single placenta (Fig. 27.4).
Twin–Twin Transfusion Syndrome (TTTS):
This occurs only in MCDA twins, the most common form of identical twins, and in about 15%. It results from unequal blood distribution through vascular anastomoses of the shared placenta (Fig. 27.4). One twin, the ‘donor’, is volume depleted and develops anaemia, IUGR and oligohydramnios. The other or ‘recipient’ twin gets volume overloaded and may develop polycythaemia, cardiac failure and massive polyhydramnios, causing, in extremis, massive distension of the uterus. Disease is staged according to Quintero in stages 1–5. Both twins are at very high risk of in utero death or severely preterm delivery. Even with optimal treatment, survival of both twins occurs in only 50%, with one twin in 80%; about 10% of survivors have neurological disability.
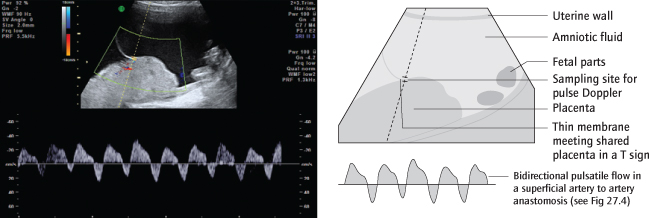
Intrauterine growth restriction is more common in MC twins, in the absence of clear blood volume discordancy. A particular problem is where the umbilical artery waveform of the smaller twin is very erratic (selective IUGR with intermittent absent or reversed end diastolic flow, abbreviated to sIUGR with iAREDF). This may be the result of the superficial artery–artery anastomoses, shown in Fig. 27.4; an ultrasound of these is shown in Fig. 27.5. Sudden in utero death occurs in up to 20% (Semin Fetal Neonatal Med 2010; 15: 342).
Co-Twin Death:
If one of an MC twin pair dies, either due to TTTS or any other cause, the drop in its blood pressure allows acute transfusion of blood from the other one: this rapidly leads to hypovolaemia and, in about 30% of cases, death or neurological damage.
Monoamniotic Twins:
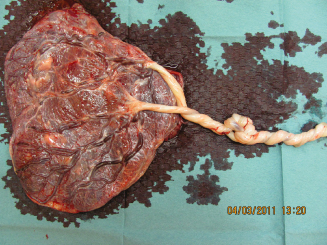
In this rare situation, not only the placenta but also the amniotic sac is shared. The cords are always entangled (Fig. 27.6). In utero demise is common, probably because of this and/or sudden acute shunting of blood between the two babies in anastomoses between the close cord insertions.
Intrapartum Complications
Malpresentation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree