Minor Burns
Penelope Terhune Louis
Approximately 2 million burn injuries occur every year in the United States. Of these, about 30,000 are treated in an inpatient setting. There are 1,000 to 5,000 pediatric deaths per year secondary to burn injury. Minor burns, which constitute approximately 95% of all burns treated in the United States, are generally superficial and do not exceed 10% of the total body surface area. They have no significant involvement of the hands, feet, face, or perineum, and they rarely require hospitalization. No full-thickness component and no other complications exist. In the management of minor burns, survival is not the issue; most of these burns heal regardless of therapy. Undertreatment and overtreatment are common and may result in infection or delayed healing, with discomfort and prolonged morbidity. The goals of minor burn management include wound healing, patient comfort, and rapid rehabilitation.
BURN ASSESSMENT
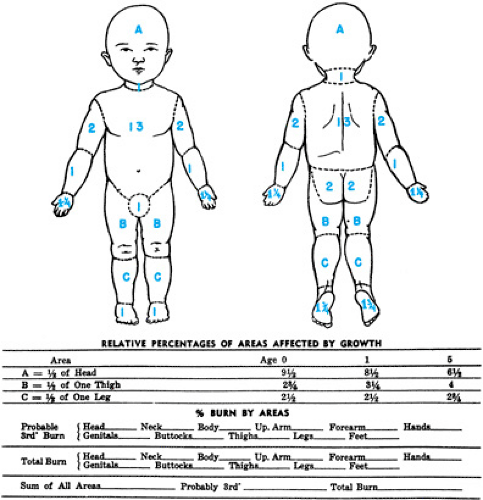
The seriousness of a burn injury can be defined by its depth, its location, the surface area involved, and patient’s age and general health. Even in minor burns, accurate estimation of the surface area is mandatory. The Lund and Browder chart should be used to adjust for the smaller surface area of the lower extremities of children (Fig. 124.1).
Burn Classification
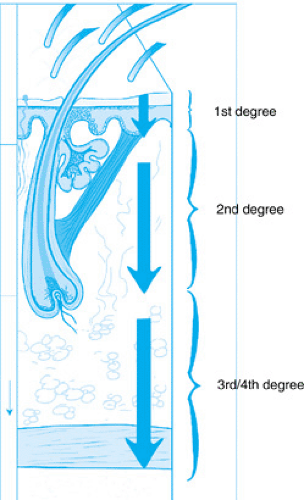
The four-level burn classification is based on the depth of the injury: first-, second-, third-, and fourth-degree burns (Fig. 124.2). In first-degree burns, tissue destruction is superficial,
involving only the epidermis. Local pain and erythema are present without blistering or systemic response. First-degree burns are the result of contact with hot liquids, exposure to ultraviolet light, or flash burns. Second-degree burns can be divided into superficial and deep partial-thickness burns. Superficial partial-thickness injuries involve only the epidermis and dermis. The wounds appear red and moist, and blisters form. Tactile and pain sensors are intact. Caused by scalds, flash, and contact with hot objects, second-degree burns heal with minimal scarring.
involving only the epidermis. Local pain and erythema are present without blistering or systemic response. First-degree burns are the result of contact with hot liquids, exposure to ultraviolet light, or flash burns. Second-degree burns can be divided into superficial and deep partial-thickness burns. Superficial partial-thickness injuries involve only the epidermis and dermis. The wounds appear red and moist, and blisters form. Tactile and pain sensors are intact. Caused by scalds, flash, and contact with hot objects, second-degree burns heal with minimal scarring.
The second-degree burns classified as deep partial-thickness burns involve the entire epidermis and dermis but leave the skin appendages intact. These deeper injuries have a mottled appearance, with areas of pale injury that are dry and anesthetic. These wounds usually heal spontaneously in 4 to 6 weeks. However, they may heal with late hypertrophic scarring and contracture formation. Deep partial-thickness burns may require excision and grafting.
Third-degree burns involve destruction of the epidermis, dermis, and subcutaneous tissue. The area appears white, red, or black and contains deep blisters or thrombosed blood vessels. The elasticity of the burned dermis is destroyed, resulting in a dry, leathery texture. These full-thickness burns require skin grafting if they are larger than 2 or 3 cm in diameter or are in an area of cosmetic importance.
Fourth-degree burns involve deep injury to bone, joint, or muscle, usually resulting from high-voltage electrical injury.
Factors Affecting the Severity of Burns
The location of the burn is important. Critical areas include the eyes, ears, face, hands, feet, and perineum. Other factors that are important are the age of the patient, associated trauma, inhalation injury, and preexisting health problems. Patients must be hospitalized for their injuries if they have severe burns, if they require fluid therapy, if they have involvement of the perineum, hands, feet, or joint surfaces, if they have circumferential extremity involvement, cellulitis, or infection at the burn site, or if they have associated trauma, facial burns, smoke inhalation, or carbon monoxide poisoning.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree