Micrognathia
Anne Kennedy, MD
DIFFERENTIAL DIAGNOSIS
Common
Technical
Idiopathic
Oligohydramnios
Trisomy 18
Less Common
Amniotic Band Syndrome
Rare but Important
Pierre Robin Syndrome
Diabetic Embryopathy
Treacher Collins Syndrome
Cornelia de Lange Syndrome
Otocephaly
Other Syndromes/Conditions
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Is micrognathia real or technical due to incorrect scan plane?
Reproducible finding if real
Use 3D ultrasound if available
Helpful to assess additional dysmorphic features (e.g., ear malposition, ear malformation, eye orientation)
Volume acquisition increases likelihood that true midline sagittal view of profile is being analyzed
Surface rendering → way to qualitatively evaluate chin from different perspectives
Help parents understand appearance and consulting services plan treatment
Mandibular measurements
Plethora of measurement described with some nomograms available, most are technically challenging & not widely used
Jaw index
Mandibular area
Inferior facial angle, mandibular angle
Mandible width/maxilla width ratio
Helpful Clues for Common Diagnoses
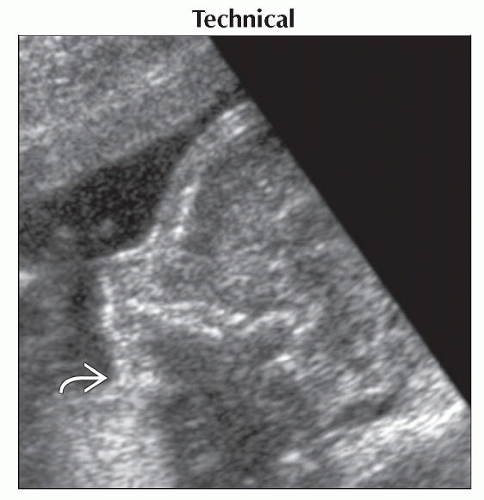
Technical
Incorrect scan plane
Idiopathic
No other abnormalities identified
May be familial; look at both parents
Oligohydramnios
Part of Potter sequence
Beaked nose, redundant skin, low set ears, club feet
Trisomy 18
Facial features include micrognathia and clefting
Usually associated with growth restriction and multiple anomalies
Omphalocele, congential heart disease, abnormal finger positioning, arthrogryposis/radial ray malformation, central nervous system anomalies, congenital diaphragmatic hernia
Helpful Clues for Less Common Diagnoses
Amniotic Band Syndrome
Random constriction/amputation defects; “slash” defects
Careful search for bands mandatory as no significant recurrence risk
Linear echoes in amniotic fluid
Extend from fetal parts to uterine wall
Fetus appears tethered or in fixed position
Occasionally, inspection of placenta after delivery may be only way to confirm diagnosis
Helpful Clues for Rare Diagnoses
Pierre Robin Syndrome
Micrognathia often severe
U-shaped palatal cleft hard to see sonographically as lip intact but may be evident on MR
Glossoptosis (posterior displacement of tongue), also easier to see on MR
Diabetic Embryopathy
Caudal regression sequence ± extremity malformations
Brain malformations including holoprosencephaly
Congenital heart disease, especially transposition and double outlet right ventricle
Long standing diabetes → IUGR, oligohydramnios
Gastrointestinal malformations (e.g., anorectal atresia)
Genitourinary malformations (e.g., renal agnesis)
Treacher Collins Syndrome
Genetic disorder characterized by craniofacial deformities
Down sloping palpebral fissures
Malar hypoplasia
Microtia
Cornelia de Lange Syndrome
Typical facies: Prominent upper lip, crescent-shaped mouth, micrognathia, fine arched eyebrows, long eyelashes
Upper extremity limb reduction defects
Congenital diaphragmatic hernia, occasionally bilateral
Intrauterine growth restriction (IUGR)
Otocephaly
Extremely rare but lethal anomaly
Microstomia
Aglossia or oroglossal hypoplasia
Agnathia or mandibular hypoplasia
Synotia: Low set medially rotated ears
Fetus cannot swallow → marked polyhydramnios
Other Syndromes/Conditions
Online Mendelian Inheritance in Man (OMIM) database includes 211 genetic conditions featuring micrognathia
Many other multiple anomaly complexes without unifying diagnosis also feature micrognathia
Micrognathia is rarely isolated
Presence mandates careful search for other anomalies and consideration of of formal fetal echocardiography
22q11 deletion associated with micrognathia and conotruncal malformations
Families should be evaluated by clinical genetics service
Important to recognize autosomal recessive conditions as 25% recurrence risk
Neu-Laxová syndrome
Lethal syndrome with IUGR
Microcephaly
Exophthalmos, absent eyelids
Nager syndrome
Severe micrognathia and malar hypoplasia
Spectrum of radial ray malformations
28% survival reported
Some dispute as to nature of inheritance, some cases appear dominant
Other Essential Information
Micrognathia may be associated with skeletal dysplasia
Assess bone density
Measure long bone lengths
Look at vertebral contours
Use 3D ultrasound
If associated with ear anomalies may also be associated with renal malformations
Neonatal renal ultrasound worthwhile
Other potential complications
Polyhydramnios → increased risk of preterm labor
Respiratory distress ± feeding difficulties and typically requires one or more surgical procedures for repair
Increased risk of genetic/syndromic condition
Image Gallery
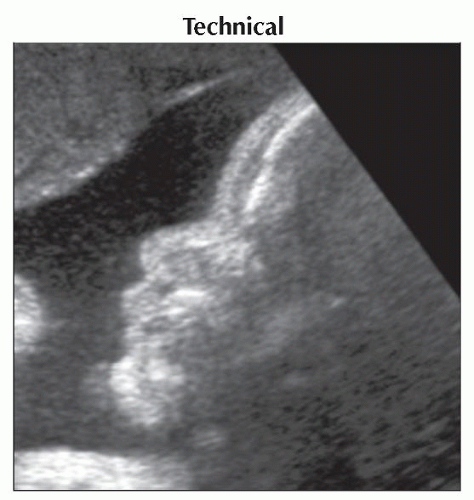 Sagittal transabdominal ultrasound in the same fetus as previous image, shows normal profile in the third trimester. The apparent micrognathia was due to incorrect scan plane. |
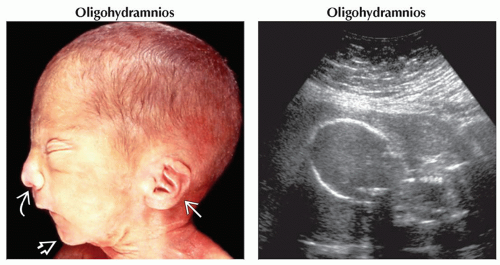 (Left) Clinical photograph shows typical Potter syndrome facies with low set ears
 and flattened nose and flattened nose  . Also note micrognathia . Also note micrognathia  . (Right) Transabdominal ultrasound is extremely compromised by maternal obesity and oligohydramnios. The lack of fluid causes compression of the fetus resulting in the “squashed” appearance seen in Potter syndrome, which was due to renal agenesis in this case. . (Right) Transabdominal ultrasound is extremely compromised by maternal obesity and oligohydramnios. The lack of fluid causes compression of the fetus resulting in the “squashed” appearance seen in Potter syndrome, which was due to renal agenesis in this case.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|