Fig. 1
PA radiograph of a small finger metacarpal neck fracture in a 14-year-old boy after a fall onto the right hand
Digit involved | Estimated relative frequency of fracture |
|---|---|
Thumb | 20 % |
Index | 16 % |
Long | 16 % |
Ring | 18 % |
Small | 30 % |
Bone involved | Estimated relative frequency of fracture |
|---|---|
Distal phalanx | 19 % |
Middle phalanx | 18 % |
Proximal phalanx | 43 % |
Metacarpal | 20 % |
Neck | 65 % |
Shaft | 8 % |
Base | 27 % |
Pathoanatomy and Applied Anatomy Relating to Pediatric Metacarpal Fractures
Metacarpal fractures arise from axial loads or bending forces, typically sustained during sporting injuries, falls onto the hand, or direct blows with a clenched fist. Metacarpal fractures typically result in apex dorsal angulation due to the line of pull of the intrinsic muscles of the hand. The thick periosteum surrounding pediatric metacarpals may minimize fracture displacement and facilitate closed reduction. In some cases, the periosteum may also become entrapped in the fracture site making anatomic reduction difficult or impossible. Specifically in the metacarpals, the periosteum provides a smooth surface for tendon gliding and speeds bone healing (Kozin and Waters 2010).
Pediatric fractures of all kinds are unique in their ability to remodel over time. Greater remodeling potential has been observed in younger children, fractures adjacent to the physis, and when the deformity is in the plane of motion – the sagittal plane in the hand. Children under age ten may remodel fractures up to 20–30° in the sagittal plane, while children older than age ten may remodel fractures up to 10–20° in the sagittal plane (Kozin and Waters 2010). Knowledge of the physeal anatomy of the hand is crucial to understanding the treatment and outcomes of pediatric metacarpal fractures. The index, long, ring, and small metacarpals have epiphyses at the distal aspect of the bones; however, the thumb metacarpal has an epiphysis at the proximal end (Lindley and Rulewicz 2006). Secondary ossification centers are located at the distal ends of the metacarpals of the index, long, ring, and small fingers. The secondary ossification center for the thumb metacarpal is located at the proximal end of the bone (Lindley and Rulewicz 2006; Fig. 2). The finger metacarpal secondary ossification centers appear at 12–27 months of age and close in late adolescence, at approximately aged 14–15 years in girls and aged 16–17 years in boys (Lindley and Rulewicz 2006). The thumb metacarpal secondary ossification center appears at 24–36 months of age and closes by 14–16 years of age (Gruelick 1959; Stuart et al. 1962).


Fig. 2
PA radiograph of the left hand of a 6-year-old girl demonstrating normal ossification centers . Secondary ossification centers are located at the distal ends of the metacarpals of the index, long, ring, and small fingers. The secondary ossification center for the thumb metacarpal is located at the proximal end of the bone
Physeal fractures are common in the pediatric hand. The anatomy of the collateral ligaments leads to Salter-Harris II and III fractures of the distal end of the metacarpals (Bogumill 1983). The ulnar and radial collateral ligaments originate at the metacarpal epiphysis and insert on the proximal phalangeal epiphysis (Bogumill 1983). Specific physeal fracture patterns involving the metacarpals will be discussed in subsequent sections.
Assessment of Pediatric Metacarpal Fractures
Clinical assessment of any pediatric injury can be challenging, particularly assessment of the pediatric hand. In addition to a thorough neurovascular examination, metacarpal injuries should always be evaluated for rotational deformity. Irreducible rotational deformity may influence treatment decisions and be an appropriate indication for operative treatment. To assess rotational deformity, the digital cascade is observed in flexion. If the patient cannot comply with active flexion of the digits, tenodesis by passive wrist extension can be used to evaluate the digital cascade. The alignment of the nail plates of the fingers should be examined with the fingers flexed and extended and compared to the contralateral hand. Subtle changes of the rotational alignment of the nail plates may also indicate malrotation (Freeland and Lindley 2006; Figs. 3 and 4). Approximately 5–10° of malrotation is typically evident on clinical examination and may be enough to cause dysfunction (Lindley and Rulewicz 2006). All metacarpal fractures should be evaluated with posteroanterior (PA), lateral, and oblique films of the hand. When obtaining an oblique radiograph, it is important to recognize that positioning the hand in supination permits better visualization of the second and third metacarpals and positioning the hand in pronation permits better visualization of the fourth and fifth metacarpals. This is particularly important because subtle fracture-dislocations of the fourth and fifth carpometacarpal joints are difficult to detect on routine radiographs. When reviewing hand films, the phalangeal line test can be used to identify subtle injuries (Campbell 1990). On a PA hand radiograph, the line drawn from the center of the phalangeal neck through the center of the phalangeal metaphysis at the level of the physis should pass through the center of the metacarpal or phalangeal head regardless of joint flexion. If this line is disrupted, there is likely an injury present (Campbell 1990; Fig. 5). It is important to recognize that subtle malrotation is not detectable on radiographs. As a consequence, emphasis on careful clinical examination cannot be overstated.




Fig. 3
Patient with a long finger metacarpal fracture and resultant malrotation (excessive pronation) of the long finger

Fig. 4
Subtle representation of malrotation in patient with ring finger metacarpal fracture and slight scissoring of the ring finger under the long finger

Fig. 5
Phalangeal line test demonstrating normal alignment of the thumb, index, and long digits with interruption of the phalangeal line in the ring and small digits due to metacarpal shaft fractures
Specialized radiographs may be helpful in specific clinical scenarios. A Brewerton view (Fig. 6) can be helpful in assessing metacarpal head fractures or other articular injuries of the metacarpophalangeal joint. In order to obtain the Brewerton view, the dorsal aspect of the hand is placed against the cassette with the metacarpophalangeal joints flexed to 65°. The central beam is then angled 15° to the ulnar side of the hand (Lane 1977; Fig. 7a, b).

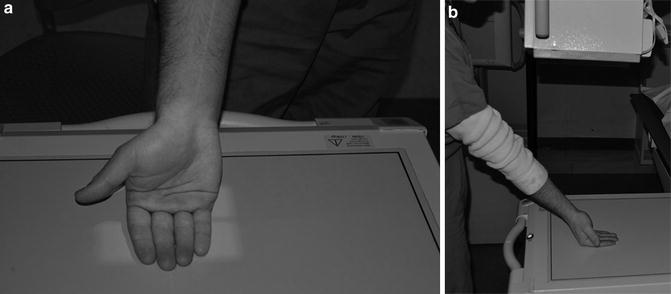


Fig. 6
Brewerton view of a Salter-Harris III fracture of the long finger metacarpal head in a 13-year-old boy who fell onto a clenched hand while snowboarding. The patient had a 15° rotational deformity and was indicated for surgery
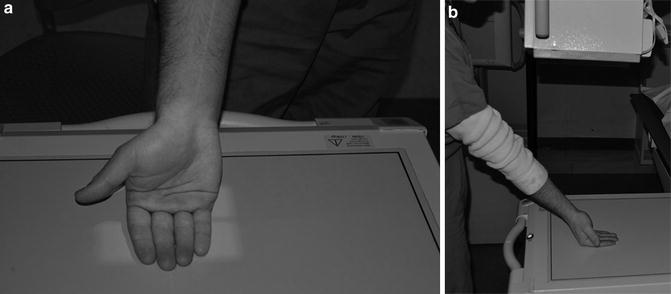
Fig. 7
(a, b) Photographs demonstrating the proper technique to obtain Brewerton view of the metacarpal head . The dorsal aspect of the hand is placed against the cassette with the metacarpophalangeal joints flexed to 65°. The central beam is then angled 15° to the ulnar side of the hand

Fig. 8
(a, b) PA and oblique radiographs of a right ring finger metacarpophalangeal joint fight bite in a patient who presented 3 weeks after the original injury. Radiographs demonstrate osteolysis of the metacarpal head suggestive of osteomyelitis. The patient also had incompetence of the ring finger extensor mechanism
Associated Injuries
In order to fully evaluate the patient with a metacarpal fracture, one must be cognizant of two specifically associated injuries – human bite injuries and hand compartment syndrome. Both of these injuries can have devastating consequences if the diagnosis is missed or delayed.
Human bite injuries are commonly associated with metacarpal head fractures or metacarpal neck fractures. Occasionally, bite injuries may not be associated with any fracture. The incidence of these injuries is not well known as patients may only present these injuries if they are associated with pain from a fracture or with a deep infection (Shoji et al. 2013). Bite injuries may be incurred in a variety of ways but commonly are due to a clenched fist contacting another person’s mouth. This so-called fight bite often involves a laceration through the skin at the level of the metacarpophalangeal joint. In this situation, the laceration occurs with the metacarpophalangeal joint in flexion, but with extension of the joint, the skin laceration may no longer align with injuries to the deeper structures. Violation of the metacarpophalangeal joint capsule is typically distal to the skin wound, while any injury to the extensor mechanism is usually located proximal to the skin wound (Bunzli et al. 1998). These injuries can lead to inoculation of the joint with oral bacteria resulting in complications such as septic arthritis, tenosynovitis, or osteomyelitis. Patients presenting with these injuries may not be forthcoming with the details or etiology of the injury (Shoji et al. 2013). For these reasons, all skin lacerations near the metacarpophalangeal joint should be considered fight bites until proven otherwise. All of these injuries should also be evaluated with radiographs. Radiographs may demonstrate an underlying fracture or foreign body (possibly a retained tooth fragment) or, in the case of delayed presentation, may show signs of osteomyelitis and destruction of the metacarpal head (Chadaev et al. 1996; Fig. 8a, b). Fight bite injuries should be treated with urgent irrigation and debridement of the wound and the metacarpophalangeal joint. This can be performed in the emergency room setting or in the operating room. All patients should have an up-to-date tetanus vaccination and be placed on prophylactic oral antibiotics for 3–5 days to cover Staphylococcus, Streptococcus, Eikenella, Corynebacterium, and anaerobes (Bunzli et al. 1998). If a patient presents in a delayed fashion or with an actively infected human bite, he or she should be taken to the operating room for irrigation and debridement (Fig. 9). In these cases, the wound should be left open to drain, and consideration should be given to treatment with a longer course of oral antibiotics or admission to the hospital for intravenous antibiotics (Bunzli et al. 1998).




Fig. 9
Operative photograph during irrigation and debridement of a 3-week-old fight bite . There was purulence in the metacarpophalangeal joint and destruction of two-thirds of the metacarpal head due to osteomyelitis

Fig. 10
Photograph demonstrating the placement of a non-sterile tourniquet on the upper arm of a patient indicated for operative treatment. Note that the tourniquet is well padded with a soft roll to prevent any soft tissue injury

Fig. 11
Sterile cotton stockinette is placed over the operative arm, and a sterile blue towel is wrapped around the edge of the tourniquet prior to draping
Hand compartment syndrome is a rare entity but, when encountered, is a surgical emergency. Compartment syndrome may occur anytime that there is a prolonged increase in interstitial tissue pressures in a fascial compartment causing ischemia (Dolan et al. 2012). Causes of compartment syndrome of the hand vary from crush injuries and blunt trauma to infiltration of intravenous substances to a tight cast or splint. One should have a higher index of suspicion for compartment syndrome in the setting of high energy trauma, multiple metacarpal shaft fractures, or carpometacarpal fracture-dislocations (Leversedge et al. 2011). There are six compartments of the hand – thenar, hypothenar, adductor, interosseus, carpal tunnel, and digits (Leversedge et al. 2011; Table 3).
Table 3
Six compartments of the hand and their respective contents
Compartment | Contents of compartment |
|---|---|
Thenar | Flexor pollicis brevis |
Abductor pollicis brevis | |
Opponens pollicis | |
Hypothenar | Abductor digiti minimi |
Flexor digiti minimi brevis | |
Opponens digiti minimi | |
Adductor | Adductor pollicis |
Interossei | 4 dorsal interossei |
3 volar interossei | |
Carpal tunnel | Median nerve |
4 flexor digitorum superficialis tendons | |
4 flexor digitorum profundus tendons | |
Flexor pollicis longus tendon | |
Digit |
Compartment syndrome is largely a clinical diagnosis and should be considered whenever the patient’s pain appears out of proportion to the injury. Other clinical signs and symptoms of compartment syndrome include “balloon hand” with tense swelling, paresthesias or progressive neurologic deficits, pain with passive stretch of the fingers or interossei, pallor, or pulselessness (Al-Qattan 2008; Leversedge et al. 2011; Table 4).
Table 4
Signs and symptoms of hand compartment syndrome
Signs and symptoms of hand compartment syndrome |
|---|
Pain out of proportion to injury |
Tensely swollen hand/“balloon hand” |
Pain with passive stretch |
Paresthesias or progressive neurologic deficit |
Pallor |
Pulselessness |
If a clinical diagnosis of compartment syndrome is not clear or cannot be obtained due to the patient’s mental status, the interstitial pressures may be measured directly. There is some debate about what measurements should constitute the diagnosis of compartment syndrome. Many consider any interstitial pressure measurement within 30 mmHg of the patient’s diastolic blood pressure at the time of measurement indicative of compartment syndrome (Matsen et al. 1980).
Once the diagnosis of compartment syndrome is established, the patient should be taken emergently to the operating room for fasciotomy. The thenar compartment may be released by a longitudinal incision along the radial border of the thenar eminence. The hypothenar compartment is released in a similar fashion with a longitudinal incision along the ulnar margin of the hand. Cadaveric studies have shown that in over half of the population, the thenar and hypothenar compartments may be comprised of more than one discreet compartment (DiFelice et al. 1998). Release of the dorsal and volar interossei is accomplished via two longitudinal incisions along the dorsal second and fourth metacarpal shafts (DiFelice et al. 1998). The adductor pollicis can be released through the longitudinal incision overlying the dorsal second metacarpal shaft or a separate, dedicated incision over the dorsal first web space to ensure adequate decompression. The carpal tunnel may also be surgically released. Care must be taken during surgical dissection to ensure all compartments are fully released. Fractures may be treated surgically at the time of fasciotomy or may be treated conservatively if minimally displaced.
Classification
Metacarpal fractures are typically classified according to the location of the fracture and further described in terms of fracture displacement, involvement of the physis, and intra-articular extension (Table 5). Classification of metacarpal fractures is largely the same between adults and children. This chapter will discuss metacarpal fractures and their management based on the location of the fracture.
Table 5
Classification of metacarpal fractures
Location of fracture | Possible subclassification |
|---|---|
Metacarpal head fracture | Intra-articular |
Open fracture/“fight bite” | |
Metacarpophalangeal fracture-dislocation | |
Metacarpal neck fracture | |
Metacarpal shaft fracture | |
Metacarpal base fracture | Intra-articular |
Carpometacarpal fracture-dislocation | |
Bennett fracture | |
Baby Bennett fracture |
Outcome Tools
Primary outcome measures for pediatric metacarpal fractures include pain as measured on a visual analog scale and metacarpophalangeal joint and interphalangeal joint motion as measured with a goniometer. There is no specific upper extremity functional outcome measure which has been validated for use in children. The American Academy of Orthopaedic Surgeons (AAOS) and the Pediatric Orthopaedic Society of North America (POSNA) developed the POSNA pediatric musculoskeletal functional health questionnaire for use in evaluating the global functional health of children with musculoskeletal disorders. The questionnaire focuses on upper extremity function, transfers and mobility, physical function and sports, comfort, happiness and satisfaction, and expectations for treatment (Daltroy et al. 1998). This questionnaire has been studied in children with and without musculoskeletal disorders and has been validated for use in children (Haynes and Sullivan 2001). Although the questionnaire encompasses upper extremity function as a factor in global functionality, it is not sufficient for evaluating upper extremity function in isolation. Future research may focus on the development of a limb-specific outcome measure which could be used to evaluate children.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


