Fig. 1
High branching bifid median nerve
A Riche-Cannieu anastomosis commonly exists between the recurrent motor branch of the median nerve and the deep branch of the ulnar nerve (50–75 %) within the fibers of the flexor pollicis brevis (FPB) that can provide dual innervation of the intrinsic muscles of the hand. In patients with a Riche-Cannieu anastomosis, the FPB may remain fully innervated after an injury to the median nerve. A more distal connection between the median and ulnar nerves has also been described. The palmar ulnar-median communicating branch of Berrettini is a distal communicating branch between the ulnar and median sensory nerves and may be present in majority of the population (Doyle and Boyte 2003; Leversedge et al. 2010).
The intraneural topography of the median nerve has been studied extensively. At the carpal tunnel, the median nerve is typically 94 % sensory and 6 % motor fascicles (Leversedge et al. 2010). Chow et al. noted that at the level of the wrist, the median nerve typically consists of three fascicular groups. The radial aspect of the nerve is composed of one large fascicular group, containing sensory and motor fascicles. The ulnar aspect of the median nerve at the wrist is comprised of two sensory fascicular groups (Chow et al. 1986).
The median nerve provides innervation to PT, FDS, FCR, and palmaris longus (PL). The AIN innervates the flexor pollicis longus (FPL), FDP to the index finger, and the pronator quadratus (PQ). The recurrent motor branch of the median nerve innervates the first and second lumbricals, abductor pollicis brevis (APB), opponens pollicis (OP) and the superficial head of the FPB; while branches from the proper digital nerve to the index and the common digital nerve to the index/middle finger innervate the first and second lumbricals, respectively. Median nerve deficits are generally classified as high or low, based on their location proximal or distal to the original of the AIN in the forearm. High median nerve injuries affect both the intrinsic and extrinsic median nerve-innervated musculature with a loss of almost all of the forearm flexor compartment muscles, intrinsic opposition, FPL, and PQ. Low median nerve injuries generally result in loss of APB and OP with partial preservation of FPB function.
Assessment of Median Nerve Injury
Assessing for nerve injuries in children is often difficult compared to examining skeletally mature individuals. The particularly difficult component of assessment is the critical sensory loss to the thumb and radial digits. The function of the FPB, still partially intact from the ulnar nerve, can fool careful observers as to the functioning of the thenar intrinsics in infants and toddlers who cannot easily cooperate during a physical examination. In fact, direct communication and participation in an exam is limited in young children. A thorough physical examination must be performed, and a high level of suspicion for nerve injuries should be maintained when a child presents with a penetrating injury or a fracture commonly associated with nerve lesions. Any uncertainty can be settled, by surgical examination of the nerve. Initial assessment in the emergency department of a seemingly benign puncture or penetrating injury may result in a missed median nerve laceration and is further complicated by the child’s anxiety in the emergency setting. Children may present with median nerve lesions from a remote injury. In delayed or occult presentation of median nerve injury in children, neglect or mutilation of an insensate digit in the median nerve distribution may be the presenting symptom and the reason for referral (Birch and Achan 2000) (Fig. 2a, b).
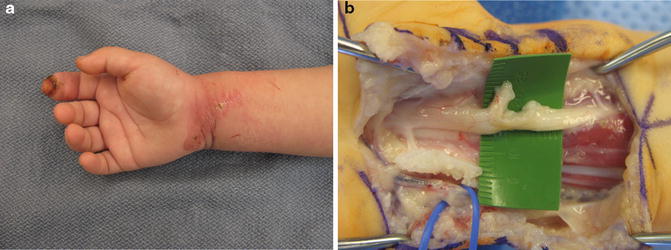
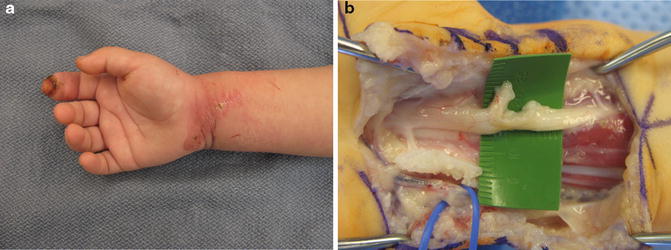
Fig. 2
(a) Healed laceration with occult median nerve injury in a child presenting with a mutilated index finger. (b) Intraoperative photograph of occult median nerve injury
Physical examination of the motor component of the median nerve is generally performed by examining the median nerve-innervated musculature. A reliable motor examination for both extrinsic and intrinsic muscles of the median nerve can be obtained by examining thumb opposition and flexion at the IP joint. In younger children, observation during activities requiring these motions can provide similar information to examination of an older child who is able to follow commands. If the examiner can gain the confidence of the child, palpating for muscle contraction can help differentiate between the integrity of the median- versus ulnar-innervated thenar intrinsics. Grading muscle strength using the standard British Medical Research Council system is almost impossible in young children, and the examiner needs to rely on the presence of muscle contraction and the child’s functional abilities during tasks to infer strength. Incorporating the evaluation of a physiotherapist can be useful.
Physical examination of the sensory component of the median nerve is more challenging. Hermann et al. reported that the normal moving two-point discrimination for children aged 4–18 is 2–4 mm. His evaluation of 348 healthy children and adolescents demonstrated that a moving two-point discrimination examination was reliable in children 6 years of age or older (Hermann et al. 1996). In children younger than 6 years old, other methods of assessing sensation and sympathetic function must be utilized. Observation of sweat in the median nerve distribution, skin wrinkling, and timed tactile gnosis can be employed to further investigate the integrity of the sensory components of the median nerve. Moberg endorsed the ninhydrin fingerprinting test to assess sweat patterns in the fingers following nerve injury (Moberg 1964). The tactile adherence test is a simple alternative test described to assess anhidrosis in which a plastic pen can be rolled against the fingertip. Frictional movement with tactile adherence will be noted if sweating is intact. However, if the skin is dry and lacks innervation, there will be no adherence of the plastic pen (Harrison 1974). An additional test of sudomotor function is the “wrinkle test” originally described by O’Riain. The patient’s hand is placed in a basin of warm water for approximately 30 min. Normally innervated skin will wrinkle, while the skin in the distribution of the injured nerve will remain smooth (O’Riain 1973) (Fig. 3) (Vasudevan et al. 2000).


Fig. 3
Three-year-old female with thumb ulnar digital nerve laceration. The “wrinkle test” illuminates the injury as the radial-sided pulp wrinkles in response to fluid immersion, while the ulnar side of the thumb pulp does not
A healthy level of suspicion for nerve injury should be held by the clinician for all children presenting with lacerations, penetrating injuries, or fractures with high associations with nerve lesions, such as posterolaterally displaced extension-type supracondylar fractures, displaced metaphyseal distal radius fractures, and Galeazzi fractures (Hosalkar et al. 2006). When nerve injuries occur in the setting of lacerations, the damage is often to the surrounding tendons, muscles, and vessels as well, but to parents and some physicians, the child’s ability to grossly flex fingers and thumb often hides the true nature of the injury. This is especially the case in lacerations involving the volar wrist crease, where unless the injury penetrates deep enough to affect the FDP, the true extent of the injury can easily be overlooked. Wounds sustained secondary to glass can be deceivingly small and conceal the true extent of the injury (Iconomou et al. 1993). Upper extremity fractures in children are more than twice as likely to be associated with nerve injuries as lower extremity fractures (Hosalkar et al. 2006). Up to 21 % of extension-type fractures of the supracondylar humerus, especially those with posterolateral displacement of the distal fragment have been associated with AIN injury. Median nerve injury has also been reported following diaphyseal fractures of the radius and ulna as well as Galeazzi fracture-dislocations (Babal et al. 2010).
In addition to a thorough physical examination, radiographs of the affected extremity can provide additional information as to the nature of the injury. More advanced imaging, such as CT or MRI, is not generally warranted in the evaluation of a suspected median nerve injury. Electromyography (EMG) and nerve conduction velocity testing can be a valuable tool in assessing median nerve injuries associated with closed injuries and with delayed recoveries. The problem with these studies is that young children do not tolerate the needle portion of the EMG testing without anesthesia therefore, the value of the results must be considered before ordering an EMG. If required, it is important to communicate exactly what information is needed to help direct the electrophysiologist to avoid unnecessary parts of the electrodiagnostic testing.
Median Nerve Injury Treatment Options
Nonoperative Management of Median Nerve Injuries
An initial trial of observation is often warranted in median nerve deficits associated with fractures, as they are often lower grade nerve injuries. Careful neurovascular examination of the involved extremity should be performed and documented both before and after a closed reduction is performed. Nerve injuries in this setting can be the result of a direct contusion or a traction injury from displacement of the fracture fragments. Spontaneous recovery in Sunderland first-degree median nerve injuries generally occurs within 3 months as there has been no disruption of the internal structures of the nerve (Sunderland 1951; Seddon 1942). Second-degree Sunderland injuries (axon disrupted, endoneurium intact) have the potential to recover at approximately 1 mm/day or 1 in./month, and children should be followed with serial physical examinations during the first 3–6 months following injury. An advancing Tinel’s sign can be serially documented in these children to track the progress of nerve recovery. In such cases, an EMG/NCS study to assess baseline injury is utilized, but it is important wait for at least 3 weeks from injury to ensure that any Wallerian degeneration is underway to obtain an accurate assessment of nerve function. A repeat study is used after 4–6 months (depending on the anatomic location of the injury) in the absence of any clinical recovery. Clinical signs of recovery include advancing Tinel’s; return of pseudomotor functions (sweat, skin pads); return of sensation (often hypesthesia initially), and motor function (Birch 2011; Kaufman et al. 2009; Waters and Bae 2012) (Table 1).
Table 1
Nonoperative management of median nerve injury
Median nerve injury: nonoperative management (initial observation) | |
|---|---|
Indications | Contraindications |
Suspected neuropraxia associated with fracture | Open fracture associated with median nerve deficit |
Gunshot wounds with nerve deficit | Laceration explored for additional injured structures with obvious nerve transection |
Median nerve injury documented to occur following closed manipulation of a fracture or dislocation | |
Outcomes of Nonoperative Management
Our experience with median nerve injury in children suggests that the mechanism of injury is the more important variable in decision-making. As demonstrated in other studies (Waters and Bae 2012), median nerve dysfunction in the setting of closed injuries warrants a 4–6-month period of observation. On the other hand, median nerve dysfunction that presents following any manipulation, such as with elbow dislocation or forearm fractures, merits more aggressive treatment including surgical exploration (Fig. 4). If a child’s injury required manipulation, and there was no assessment prior to the reduction, than any median nerve dysfunction is presumed to be new and merits surgical exploration.


Fig. 4
Median nerve entrapped within the elbow joint following closed reduction of a posterior elbow fracture-dislocation involving the medial epicondyle. The nerve deficit was not recognized until well after the fracture had healed
Children with gunshot wounds to the upper extremity can present a clinical challenge. The injuries can vary dramatically based on the velocity of the weapon as well as the proximity of the weapon to the child at the time the injury was sustained. A peripheral nerve can be transected or damaged directly by the projectile, or it can be injured indirectly by shock wave cavitation, the energy the projectile emits through the surrounding soft tissues (Oberlin and Rantissi 2011). Additionally, peripheral nerves can be irritated and injured by shrapnel embedded within the soft tissues after the gunshot wound is sustained. If a child presents with median nerve palsy following injury with a stable bullet that travelled in proximity to the anatomic location of the median nerve, there is a high likelihood of direct injury to the nerve, and therefore early exploration and repair is recommended. With a large cavitation injury, it is possible that a median nerve palsy might be secondary and an initial period of observation may be appropriate (Oberlin and Rantissi 2011; Stoebner et al. 2011). Roganovic specifically reported on a series of Sunderland grade V median nerve injuries sustained secondary to missiles. He concluded that children have better recovery following repair of the median nerve in this clinical scenario and that both the level of the repair and the time between injury and surgical repair were independent predictors of successful outcome for motor and sensory recovery (Roganovic 2005). It is ultimately up to the treating surgeon’s judgment, but such injuries often require urgent operative treatment, and so the nerve should be routinely explored in these situations.
Operative Treatment of Median Nerve Injuries
The surgical approach to any peripheral nerve injury is best understood by dividing the injury into the treatment of acute versus chronic injuries and sharp lacerations versus stretch/crush injuries where the “zone” of nerve injury is greater. The majority of surgical treatment in acute and subacute injuries involves lacerated median nerves as the presence of an open wound in the face of a nerve deficit often infers a nerve laceration. In contrast, the majority of surgery in the chronic setting manages stretch and crush injuries, as these are the mechanisms of injury associated with most closed injuries. The challenge in both situations is accurately assessing the zone of injury so that the surgeon can confidently repair or graft healthy viable nerve endings resulting in a greater likelihood of success. The challenge more often found in the latter situation is assessing the nerve injury intraoperatively, especially when the nerve is in continuity and there is a neuroma in continuity. Another issue critical to the surgical treatment of the median nerve issue concerns the estimated time of nerve regeneration. Repaired and healing nerves advance at a rate of about 1 mm/day. The target muscles for reinnervation start the process of internal degeneration the moment of denervation, and it is assumed and understood that at some point in time, 18–21 months from the time of injury, the denervated muscles undergoes irreversible end-plate demise while the muscle fibers themselves undergo morphological changes that will make them irreversibly fibrotic. Moreover, the sooner the muscles are reinnervated, the greater the potential return of strength. The surgeon must take these factors into account as he/she decides the optimum time to intervene along with the best methods of repair and reconstruction.
Sharp knife lacerations and penetrating injuries secondary to glass are a common cause of median nerve injury in children and typically present soon after the injury (Iconomou et al. 1993). If a nerve deficit is identified or suspected, surgical exploration is warranted. The laceration may be explored acutely if other injuries require urgent surgical intervention (acute hemorrhage) or can be delayed for up to a week or so. One of the advantages of delayed exploration is the better ability to gauge the zone of injury that can extend beyond the immediate margins of the lacerated nerve ends. The dissection and identification of the injured structures is generally easier if performed earlier, before scar tissue has the opportunity to form, and the nerve ends retract proximally and distally from the site of the laceration (Birch 2011; Waters and Bae 2012). In the setting of an open fracture with an associated median nerve deficit, operative exploration at the time of fracture debridement and fixation is advised.
Primary repair of the median nerve is usually possible in the acute and subacute setting without the need for substantial mobilization, posturing of the elbow or wrist, or nerve graft/conduit provided a narrow zone of injury (Kaufman et al. 2009). Even if the zone of injury is up to 2 cm, or viable nerve ends are about 2 cm apart, a primary repair is achievable. If the gap is greater than 4cm; however, a ‘bridge’ will be necessary (Hosalkar et al. 2006). The lacerated nerve ends are prepared by sharp resection until the organized internal architecture of the nerve is visualized and appears healthy (Birch 2011). Less resection is generally required in both lacerations and acute repairs, while crush, stretch, and contaminated injuries can lead to considerable nerve damage proximal and distal to the visible zone of injury even in the acute setting. A tension-free repair is critical to the potential for nerve recovery. During repair of an acute or chronic nerve injury, elongation of 15 % results is a severe decrease in blood flow and therefore a decreased potential for nerve regeneration (Clark et al. 1992).
Positioning and exposure of the median nerve can help facilitate a tension-free repair. With the patient in the supine position and the operative arm placed on a stable hand table, flexion of the wrist and hand can help approximate the ends of the nerve and decrease tension across the repair site. This position can be maintained intraoperatively with the use of any commercially available surgical hand positioner/immobilizer. Careful mobilization of potential soft tissue tethers proximal and distal to the repair can also aid in decreasing tension. Proximal forearm injuries to the median nerve may require division of the pronator fascia to increase visualization and ability to mobilize the proximal portion of the nerve (Pederson and Person 2008). The clinician should consider release of any known areas of constriction distal to repair site as compression has been reported to delay and impair nerve regeneration (Johnston et al. 1993). In distal forearm median nerve injuries, release of the carpal tunnel should be considered. When injuries to the median nerve occur at the level of the wrist or palm, the transverse carpal ligament will likely need to be released for proper exposure of the proposed site of repair.
Primary surgical repair can be epineural, fascicular, or group fascicular. For digital nerve lacerations, an end-to-end epineural repair is performed with 9-0 nylon using the microscope. An epineural repair with 8-0 nylon can also be performed for more proximal lacerations to the median nerve in the forearm and wrist (Fig. 5a, b). The advantages of the epineural repair lie in its surgical simplicity and gentleness compared to other repairs that require internal dissection and damage to the perineural vessels. The surgeon can use the epineural vascular anatomy to line up vessels as well as aligning matched fascicles to perform as anatomic a repair as possible (Tables 2, 3, and 4). A fascicular repair requires stripping the outer epineurium and then directly aligning the perineurium of individual fascicles within the median nerve. This is more feasible distally in the forearm and wrist level as the internal fascicles are organized into a more predictable alignment and there are fewer in number. A compromise between the two techniques is that of grouped fascicular repair, which requires less traumatic dissection but aligns groups of fascicles with segmental sutures through the inner epineurium (Issacs 2010). This technique is particularly useful in the distal median nerve in the forearm where the intraneural topography is well documented (Chow et al. 1986). Despite multiple investigations, the superiority of epineural or fascicular repairs has not been definitively proven (Issacs 2010; Orgel and Terzis 1977). Cabaud et al. demonstrated no statistically significant difference in the results of peripheral nerve repairs performed with epineural or perineural fascicular techniques (Cabaud et al. 1976).
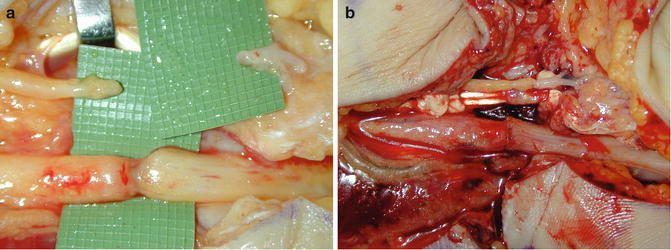
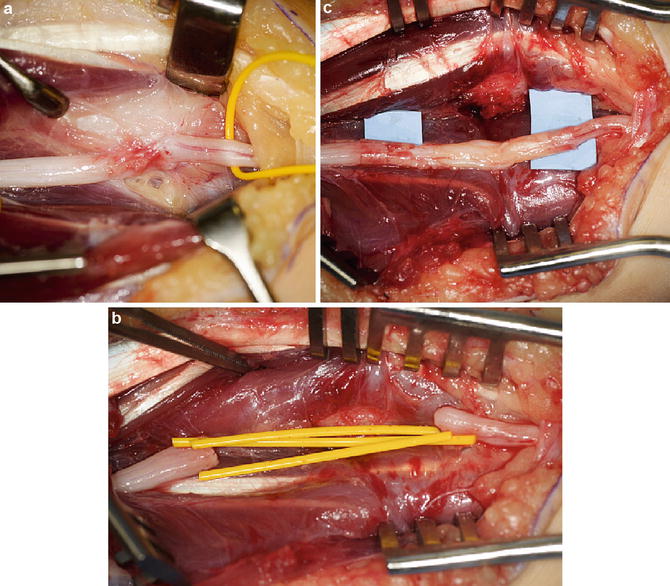
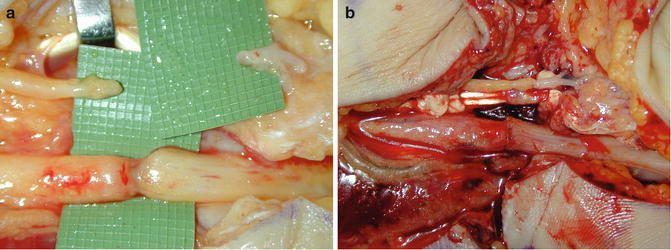
Fig. 5
(a) Median nerve laceration in forearm. (b) Primary epineural repair of median nerve in forearm
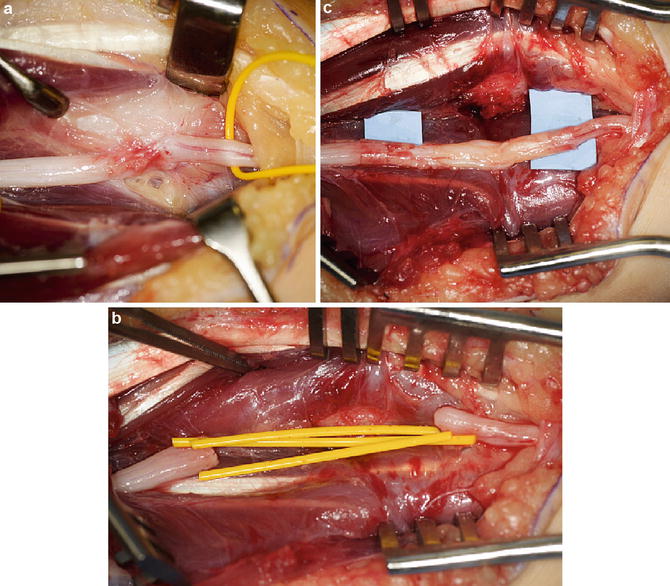
Fig. 6
(a) Photograph of a median nerve exploration in the forearm for a child who failed to recover median nerve function following a palsy sustained as the result of a displaced both bones forearm fracture. Intra-operative nerve testing failed to demonstrate any evidence of conductivity across the zone of injury. (b) Proximal and distal stumps of healthy nerve left once the zone of injury was sharply resected. This defect is too large for primary repair. (c) Median nerve is reconstructed using auto-cable grafts secured at each stump with fibrin glue and reinforced with nerve-tubes. (Case and operative photographs courtesy of Scott Kozin, MD)
Table 2
Operative treatment → primary epineural repair for median nerve laceration (preoperative planning)
Primary nerve repair for median nerve laceration |
|---|
Preoperative planning |
1. OR table: standard OR table with hand table attachment (with a stabilizing leg) |
2. Positioning: supine |
3. Equipment: loupe magnification, operating microscope, micro instruments, 8-0, 9-0, and 10-0 nylon, 11 blade, sterile tongue depressor, and hand stabilizer for palmar or digital lacerations |
4. Tourniquet: non-sterile |
Table 3
Operative treatment → primary epineural repair for median nerve lacerations (surgical technique)
Primary nerve repair for median nerve lacerations |
|---|
Surgical steps (epineural repair) |
1. Sterile prep and drape the extremity, inflate tourniquet, place hand in alumi-hand if palmar or digital laceration is present |
2. Extend traumatic laceration → Bruner or mid-axial on the hand and digits, straight on the volar forearm with zigzags around the wrist creases |
3. Exploration of wound under loupe magnification for associated injuries |
4. Identify nerve stumps proximally and distally |
5. Irrigate and debride wound bed |
6. Prepare nerve stumps → resect unhealthy portions of nerve using 11 blade on sterile tongue depressor until healthy organized nerve is observed in proximal and distal stump |
7. Repair any additional injured structures |
8. Reapproximate nerve ends using nylon (8-0 in distal forearm, 9-0 or 10-0 for more distal injuries) using the microscope. The 9-0 and 10-0 gauges may be the appropriate size for forearm and wrist level repair in infants at the surgeon’s discretion. Place 2 sutures through the outer epineurium 180° apart. Use neural vasculature to help orient stumps appropriately |
9. Assess the tension on the repair and its stability by mobilizing the wrist and fingers |
10. Irrigate wound |
11. Close incision with absorbable suture |
Table 4
Operative treatment → primary epineural repair for median nerve lacerations (postoperative protocol)
Primary nerve repair for median nerve lacerations |
|---|
Postoperative protocol |
1. Immobilize postoperatively in splint or cast (surgeon preference). Use long arm cast in young children and any circumstances where elbow motion applies undue tension on the nerve repair. Keep fingers and thumb free (assuming digital nerve not repaired) to allow for some degree of early nerve/tendon differential gliding. In cases where arm positioning was required for a direct repair, one can put some flexion on the wrist, but it should not exceed 30–40° of flexion |
2. Anticipate early mobilization, within 1–2 weeks of surgery, depending on the tension of repair and stability as determined in Step #9. With older children, early mobilization with splint protection allows differential nerve/tendon gliding. In younger children, or noncompliant children of any age, continue cast-type protection for 3 weeks postoperatively |
3. With the aid of a physiotherapist, work on early range of motion, wound care, strengthening when range of motion is restored, and neurosensory reeducation techniques |
Although microsurgical repair of peripheral nerves is generally performed using nonabsorbable microsutures, the development of fibrin adhesives offers a sutureless alternative (Isaacs 2010; Isaacs et al. 2008). Theoretically, nerve repair utilizing adhesive alone could decrease operative time and traumatic handling of the nerve ends. Moy et al. reported an improvement in the speed of repair of peripheral nerves using a fibrin seal versus suture, but found increased reactive changes within the earlier periods of nerve regeneration histologically (Moy et al. 1988). However, others have demonstrated decreased inflammatory response and an environment more conducive to nerve growth when using fibrin adhesives to perform a peripheral nerve repair (Ornelas et al. 2006; Palazzi et al. 1995).
Overall, children are believed to have better potential for functional motor and sensory recovery following nerve injury and nerve repair (Birch and Achan 2000; Chemnitz et al. 2013; Senes et al. 2009; Ruijs et al. 2005). Primary repair of a median nerve laceration in an end-to-end fashion is preferred over use of a graft or conduit. Hudson et al. found very satisfactory return of opponens pollicis function (4.5 out of 5) and a mean static two-point discrimination of 5 mm in children who underwent primary epineural repair of the median nerve (Hudson et al. 1997). Tajima reported excellent recovery of moving and static two-point discrimination in children who underwent group fascicular repair of the median nerve at the level of the wrist (Tajima and Imai 1989). In children who sustained penetrating injuries to the median nerve from glass, repair of the median nerve resulted in very satisfactory sensory return and acceptable motor function, with the best results seen in the children who underwent primary fascicular repair (Iconomou et al. 1992). In studies that compare the results of repair and grafting among the various upper extremity nerves, median nerve injuries tend to respond very favorably to surgical repair and reconstruction compared to the radial and ulnar nerves (Murovic 2009).
For segmental defects in the median nerve of 3–4 cm or greater, a tension-free end-to-end repair is difficult to achieve primarily. Options for bridging the defect when positioning the wrist/elbow and mobilizing the nerve proximally and distally are insufficient include autograft, allograft, and nerve conduit. Autografts remain the most thoroughly researched and proven of the three options for repairing longer nerve gaps. Autografts are obtained from sensory nerves of similar size to the segment of the median nerve in need of grafting. The sural nerve can be used (and cabled) for sections of the median nerve in the forearm. The medial and lateral antebrachial cutaneous nerves, the medial brachial cutaneous nerve, or the posterior interosseous nerve from the dorsum of the wrist can be employed for more distal areas of injury to the median nerve in the palm and digits. Results of median nerve grafting with autograft in children are generally superior to that found in adults, but are inferior to results of primary nerve suture. Ceynowa et al. performed a retrospective review of children and adolescents who underwent nerve grafting to the median or ulnar nerves using sural nerve grafts with a mean graft length of 2.8 cm. Although results were good overall with a mean DASH score of 14.6 (average period of observation of 7 years), two-point discrimination return was incomplete. Motor function was better in patients with median nerve injuries (Ceynowa et al. 2012). The results of nerve grafting to restore function in the setting of long segmental defects (>5 cm) are somewhat mixed. Long segmental defects can be grafted with favorable results, but shorter defects seem to experience better outcomes (Socolovsky et al. 2011; Karabekmez et al. 2009; Daoutis et al. 1994).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


