It is a great pleasure to be able to agree with Dr Leveno et al regarding recent changes to US recommendations for the management of the second stage of labor to the upper limits of 3 (multiparous with epidural) and 4 hours (nulliparous with epidural) respectively. Our first concerns should surely be long-term maternal and fetal welfare rather than short term, process indicators such as caesarean delivery rates.
In a longitudinal prospective study (Avon Longitudinal Study of Pregnancy and Childbirth) of 2240 nulliparous women, there was an approximate doubling of the risk of severe gynecological symptoms at 47 months after delivery associated with induced, augmented, or prolonged (>12 hours) labors, fetal weight (>4000 g), malpresentations, or operative vaginal delivery.
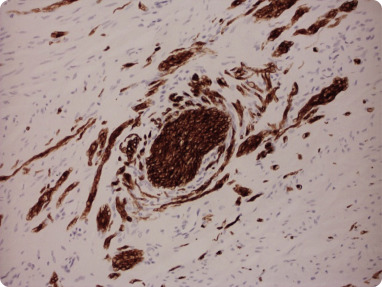
Because most women with gynecological problems do not present to a physician until 5–10 years after a first labor, this may grossly underestimate the true impact of intrapartum care on subsequent gynecological outcomes. In particular, prolonged (>2 hours) and premature (prior to full dilatation), maternal voluntary efforts in nulliparous labor cause irreparable injuries to a woman’s pelvic organs and their supports, with grave consequences for the rest of her life. Avulsion of the tendinous origins of the levator ani from the obturator internus at the arcus tendineus levator ani, and branches of the hypogastric plexi that lie medial to the levator ani, is the primary pathoanatomy. Aberrant, and chaotic, perivascular reinnervation in adjacent pelvic organs ( Figure ) results in chronic pelvic pain with, or without, endometriosis, menstrual disturbances, and vaginal and vulval pain as well as irritative bladder and bowel symptoms.