20.5 Liver diseases
Normal liver anatomy and function
Pattern recognition in acute and chronic liver dysfunction
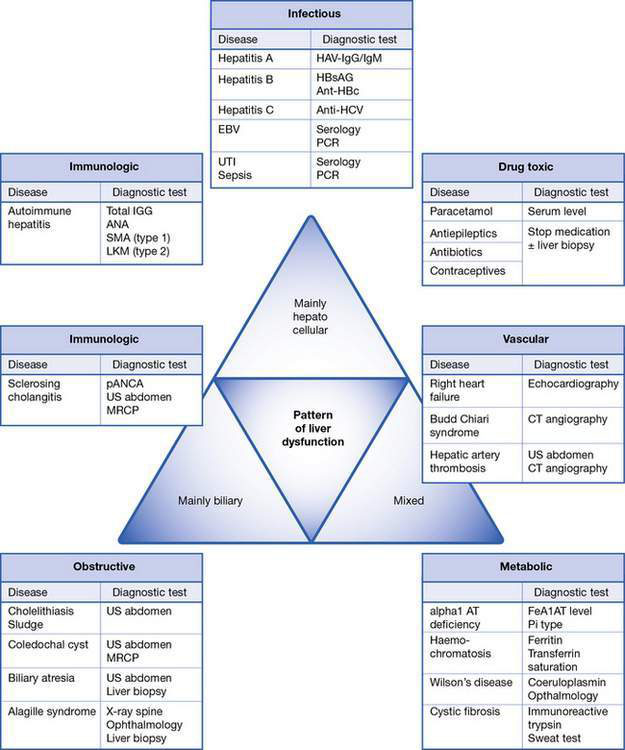
Assessment of liver dysfunction in the child is part of a diagnostic process involving a thorough clinical history, clinical symptoms and signs, and a complete panel of ‘liver function tests’ (see below). The integration of these results will allow further categorization of the disease process. Depending on which morphological and functional compartment is affected, liver disease can be primarily hepatocellular (parenchymal), biliary (cholestatic) or mixed hepatocellular–biliary, and can finally lead to failure of synthetic and detoxification function. Allocation of laboratory tests to a disease pattern results in more targeted investigations (Fig. 20.5.1).
Laboratory patterns of liver dysfunction
Clinical signs of liver dysfunction
A thorough history and clinical examination are essential to guide the diagnostic approach in a child with suspected liver disease. When trying to identify the cause of liver disease, it is useful broadly to categorize children into infants versus older children, acute versus chronic liver disease, and biliary (cholestatic) versus hepatocellular injury. Of course, there will be significant overlap, but the categories are described in detail below and in Table 20.5.1 and Fig. 20.5.1.
Table 20.5.1 Clinical and aetiological categories of liver disease in childhood
| Mode of presentation | Time of presentation | |
|---|---|---|
| Infancy | Older child | |
| Acute | Infectious Biliary/obstructive Metabolic Ischaemic Immunological | Infectious Biliary/obstructive Metabolic Drug-induced Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|