CHAPTER 7 thrombosis of the main hepatic veins. most common benign neoplasm of the liver consisting of large blood-filled cystic spaces. an accessory blood pathway developed through enlargement of secondary vessels. divides the liver into eight segments in an imaginary H pattern. an infectious cystic disease associated with underdeveloped sheepherding areas of the world. excessive deposition of neutral fat within the parenchymal cells. functional lobar–segmental anatomy divides the liver into the right, left, and caudate lobes. blood flowing away from the liver. region in the hepatic hilum containing the proper hepatic artery, common duct, and main portal vein. extension of the right lobe inferior and anterior to the lower pole of the right kidney. a passageway between two natural channels. a tube designed to be inserted in a passageway or vessel to keep it patent. divides the liver into the right, left, caudate, and quadrate lobes. congenital cyst formation associated with weakening of the bile duct wall. • The liver is the largest solid organ in the body, weighing up to 1600 grams in males and 1400 grams in females. • The liver is attached to the diaphragm, anterior abdominal wall, stomach, and retroperitoneum by ligaments. • Consists of an upper and a lower layer. • The upper layer is formed by the peritoneum from the upper margin of the bare area to the undersurface of the diaphragm. • The lower layer is reflected from the lower margin of the bare area to the right kidney and is termed the hepatorenal ligament. • The right and left triangular ligaments are part of the coronary ligament. • Proper hepatic artery enters the liver at the porta hepatis and divides into the right and left hepatic arteries. • Thirty percent of the liver’s blood supply is through the hepatic artery. • Lies medial to the common hepatic duct and anterior to the main portal vein. • Normal diameter of the proper hepatic artery is 2 to 4 mm. • Right, middle, and left hepatic veins converge to empty into the inferior vena cava. • Transport deoxygenated blood from the liver cells to the inferior vena cava. • Course between lobes (interlobar) and between segments (intersegmental). • Have a minimum amount of collagen in the walls. • Follow a straight longitudinal course increasing in caliber closer to the diaphragm. • Main portal vein enters the porta hepatis, dividing into the right and left portal veins. • Left portal vein subdivides into the left medial and left lateral portal veins. • Right portal vein subdivides into the right anterior and right posterior portal veins. • Provide approximately 70% of the liver’s blood supply. • Transport nutrient-rich blood from the digestive tract to the liver cells for metabolic processing and storage. • Are located within the lobes (intralobar) or within the segments (intrasegmental) of the liver. • Normal diameter of the main portal vein should not exceed 13 mm. • Lies anterior and medial to the inferior vena cava. • Located posterior to the ligamentum of venosum and porta hepatis. • Nothing by mouth (NPO) 6 to 8 hours before examination for adults, 6 hours for children, and 4 hours for infants. • Emergency examinations may be performed without preparation. • Use the highest-frequency abdominal transducer possible to obtain optimal resolution for penetration depth. • Place gain settings to display the normal liver parenchyma as a medium shade of gray with adjustments to reduce echoes within the vessels. • Focal zone(s) at or below the place of interest. • Sufficient imaging depth to visualize structures immediately posterior to the region of interest. • Harmonic imaging or decreasing system compression (dynamic range) can be used to reduce artifactual echoes within anechoic structures. • Spatial compounding can be used to improve visualization of structures posterior to a highly attenuating structure. • Systematic approach to evaluate and document the entire liver in both the longitudinal and transverse planes using specific anatomical landmarks. • Longitudinal and anteroposterior diameter measurements of the liver should be included. • Anteroposterior diameter measurement of the common hepatic or common bile duct should be included. • Color Doppler imaging, using a 60-degree angle or less, to evaluate flow direction and spectral analysis of the portal and hepatic veins. • Evaluation and documentation of intrahepatic and extrahepatic bile ducts. • Documentation and measurement of any abnormality in two scanning planes with and without color Doppler should be included. • Normal adult range 35 to 150 U/L. • An enzyme produced primarily by the liver, bone, and placenta and excreted through the bile ducts. • An enzyme present in many kinds of tissue that is released when cells are injured or damaged; levels will be proportional to the amount of damage and the time between cell injury and testing. • Used to diagnose liver disease before jaundice occurs. • Elevation associated with cirrhosis, hepatitis, and mononucleosis. • Normal total bilirubin 0.3 to 1.1 mg/dL. • Normal direct bilirubin 0.1 to 0.4 mg/dL. • A product from the breakdown of hemoglobin in old red blood cells; a disruption in the process may cause abnormal levels; leakage into tissues gives the skin a yellow appearance. • Reflects the balance between production and excretion of bile. • Elevation of direct or conjugated bilirubin is associated with obstruction, hepatitis, cirrhosis, and liver metastasis. • Elevation of indirect or nonconjugated bilirubin is associated with nonobstructive conditions. • Normal clotting time is 10 to 15 seconds. • Enzyme produced by the liver. • Production depends on amount of vitamin K. • Elevation associated with cirrhosis, malignancy, malabsorption of vitamin K, and clotting failure.
Liver
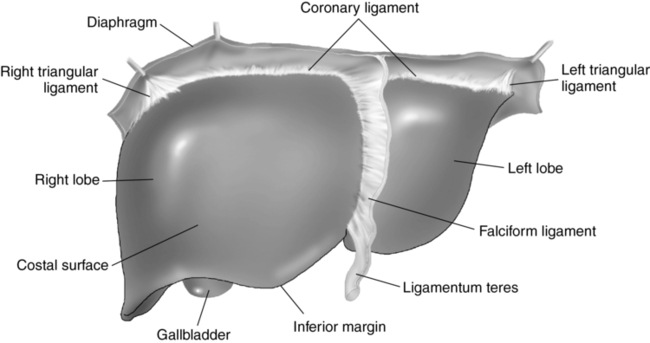
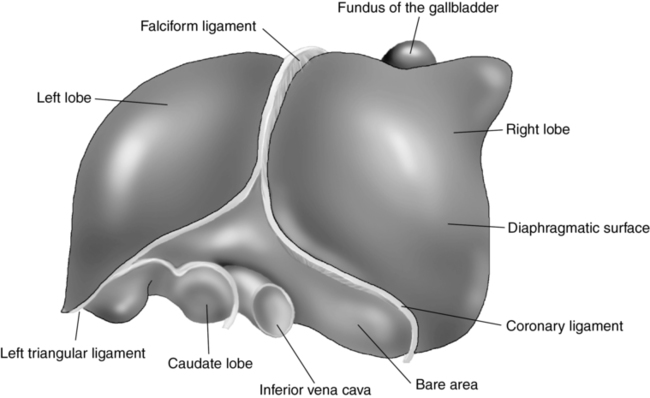
Anatomy (figs. 7-1 and 7-2)
Liver ligaments
Coronary
Vascular anatomy
Hepatic arteries
Hepatic veins
Portal veins
Location
Caudate lobe
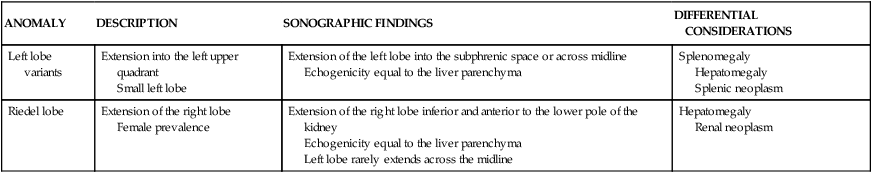
ANOMALY
DESCRIPTION
SONOGRAPHIC FINDINGS
DIFFERENTIAL CONSIDERATIONS
Left lobe variants
Extension into the left upper quadrant
Small left lobe
Extension of the left lobe into the subphrenic space or across midline
Echogenicity equal to the liver parenchyma
Splenomegaly
Hepatomegaly
Splenic neoplasm
Riedel lobe
Extension of the right lobe
Female prevalence
Extension of the right lobe inferior and anterior to the lower pole of the kidney
Echogenicity equal to the liver parenchyma
Left lobe rarely extends across the midline
Hepatomegaly
Renal neoplasm
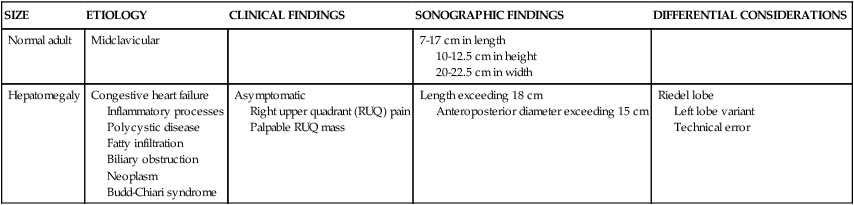
SIZE
ETIOLOGY
CLINICAL FINDINGS
SONOGRAPHIC FINDINGS
DIFFERENTIAL CONSIDERATIONS
Normal adult
Midclavicular
7-17 cm in length
10-12.5 cm in height
20-22.5 cm in width
Hepatomegaly
Congestive heart failure
Inflammatory processes
Polycystic disease
Fatty infiltration
Biliary obstruction
Neoplasm
Budd-Chiari syndrome
Asymptomatic
Right upper quadrant (RUQ) pain
Palpable RUQ mass
Length exceeding 18 cm
Anteroposterior diameter exceeding 15 cm
Riedel lobe
Left lobe variant
Technical error
Technique
Preparation
Examination technique and image optimization
Laboratory values
Alkaline phosphatase
Aspartate aminotransferase (ast)
Bilirubin
Prothrombin time
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Liver