Dysplasia
Gene defect
Mode of inheritance
Diastrophic dysplasia
DTDST gene (5q32-q33.1)
AD
Multiple epiphyseal dysplasia (MED)
Type I
Type II
COMP (Chr19)
COL9A2
AD, less commonly AR
Pseudoachondroplasia
COMP (chromosome 19q13)
AD
Ellis-van Creveld syndrome
EVC gene (chromosome 4p16)
AR
Achondroplasia
FGFR3
80 % Sporadic mutation
20 % AD
Hypochondroplasia
FGFR3/IGF-1
Spontaneous mutation, less commonly AD
Spondyloepiphyseal dysplasia (SED)
Type II collagen
Congenita: AD
Tarda: x-linked recessive
Kniest syndrome
Type II collagen
AD
Metaphyseal chondrodysplasias
Schmid type
Jansen type
McKusick
Collagen type X A1 chain deletion
PTHRP (chromosome 3p22-p21.1)
RMRP (chromosome 9)
AD
AD
AR
Cleidocranial dysostosis
RUNX2/CFBA1gene (chromosome 6)
AD
Morquio syndrome (type IV Mucopoly-saccharidosis)
GALNS/GLB1 gene defect
AR
Table 19.2
Selected systemic abnormalities in patients with skeletal dysplasias
System involved | Pathologic condition | Skeletal dysplasia |
|---|---|---|
Head | Hydrocephalus | Achondroplasia |
Eye | Cataracts Retinal detachment | Morquio syndrome SED congenital, Kneist |
Ear | Recurrent otitis media Hearing loss | Achondroplasia, Kneist Kneist |
Cardiac | Congenital heart defects Acquired (cardiomyopathy, valvular disease) | Ellis-van Creveld dysplasia Morquio syndrome |
Respiratory | Laryngotracheomalacia Central +/− obstructive sleep apnea Restrictive lung disease | Campomelic dysplasia, diastrophic dysplasia Achondroplasia Metatropic dysplasia, thanatophoric dysplasia, Ellis-van Creveld dysplasia |
Immunologic | T-cell impairment, neutropenia, anemia | McKusick metaphyseal chondrodysplasia |
Skeletal abnormalities in patients with skeletal dysplasias can be a source of considerable morbidity and often need surgical correction [5, 10]. These may result from:
1.
Shortening of specific limb segments (rhizomelic, mesomelic, and acromelic) characteristic of many disproportionate skeletal dysplasias with short stature.
2.
Unequal growth rates of paired long bones in the forearm and leg (e.g., relatively long fibula in achondroplasia associated with genu varum; and relatively short fibula in chondro-ectodermal dysplasia associated with genu valgum).
3.
Joint contractures, deformities, and instability: Joint contractures result from angular deformation centered at the joints rather than in the adjacent physeal and metaphyseal regions of the developing bones. These are almost always in flexion and are particularly characteristic of diastrophic dysplasia. Joint instability can result from a combination of generalized ligamentous laxity and structural epiphyseal abnormality (e.g., spondyloepiphyseal dysplasia, Morquio syndrome).
Lower Extremity Deformity in Skeletal Dysplasia
Individuals with skeletal dysplasias are not only shorter in stature than the average population, but each dysplasia has its own set of unique skeletal abnormalities (Box 19.1). In addition, the natural history of these dysplasias is highly variable and influences decision making. Characteristic deformities at various bones and joints are seen in skeletal dysplasias (Table 19.3).
Table 19.3
Characteristic deformities of various skeletal dysplasias
Deformity | Skeletal dysplasia |
|---|---|
Acetabular dysplasia | Diastrophic dysplasia MED Morquio syndrome |
Coxa vara | Cleidocranial dysplasia MED Pseudoachondroplasia SED—congenita Schmid metaphyseal chondrodysplasia |
Coxa valga | Morquio syndrome |
Hip degenerative disease | Pseudoachondroplasia MED SED |
Genu varum | Achondroplasia McKusick metaphyseal chondrodysplasia (mild) Pseudoachondroplasia Schmid metaphyseal chondrodysplasia |
Genu valgum | Diastrophic dysplasia Ellis-van Creveld syndrome MED Morquio syndrome Pseudoachondroplasia SED – congenita |
Internal tibial torsion | Achondroplasia Schmid metaphyseal chondrodysplasia |
External tibial torsion | |
Ankle varus | Achondroplasia McKusick metaphyseal chondrodysplasia (mild) Schmid metaphyseal chondrodysplasia |
Talipes equinovarus | SED (supple) Diastrophic dysplasia (rigid) |
The challenges of deformity correction in skeletal dysplasia patients include:
Multifocal, and often multiplanar deformities (sagittal, coronal, rotational, and translational).
The abnormalities in ossification can impair visualization of the chondro-osseous structures and joint lines on plain radiographs, adding another level of difficulty to planning the deformity correction. This may necessitate additional imaging studies such as MRIs (often needing sedation or anesthesia, which is not without its difficulties) and CT scans as well as liberal use of intraoperative arthrograms.
Deformity at one site (and its correction) may influence the development and/or progression of deformities at adjacent sites. Other challenges include deciding which deformities need to be managed surgically and which can be accommodated by adjacent correction.
Skeletal dysplasias can affect the quality of bone and cartilage. Therefore, it is imperative to have an understanding of the pathophysiology and natural history of these conditions. These differences can affect the types of correction and fixation used. The size and quality of bone often times may influence implant selection and necessitate creativity in the operating room in order to accomplish the desired surgical goals.
Box 19.1
Each skeletal dysplasia is unique with specific skeletal and systemic manifestations. Evaluation by an experienced multidisciplinary team is essential.
Deformities in skeletal dysplasias are usually multifocal and multiplanar.
Deformities may arise from bony, articular, as well as soft tissue abnormalities. These may need to be addressed individually for appropriate correction.
Patients with certain skeletal dysplasias have upper cervical instability and need appropriate evaluation.
Surgical Considerations
Preoperative Evaluation
Evaluation of a child with skeletal dysplasia is best performed by a multidisciplinary team (including orthopedic surgery, genetics, physical and occupational therapists, and other necessary specialists such as otorhinolaryngology, neurosurgery, ophthalmology, and dentistry) familiar with these conditions [5, 11]. A thorough history, including questions regarding pain, endurance, gait abnormalities, activities of daily living, and recreation, provides clues to functional limitations. A detailed systemic evaluation is also indicated and may identify major, sometimes life-threatening, issues (see Table 19.2). The extremities should be examined for range of motion, ligamentous laxity, joint contractures, and malalignment (in all planes). Examination of the spine for sagittal and coronal plane deformities and a thorough neurological examination are needed because of the frequent incidence of spinal deformities, instability, and neurological compromise in certain dysplasias. Cervical spine instability is common in mucopolysaccharidoses like Morquio syndrome, spondyloepiphyseal dysplasia (SED), diastrophic dysplasia, pseudoachondroplasia, and chondrodysplasia punctata. Flexion-extension radiographs are useful in evaluating such patients who may be at risk for cervical instability, especially if they have symptoms of neck pain and long track signs. We use flexion-extension radiographs in most dysplasias, except for achondroplasia, at presentation and also intermittently thereafter, especially in dysplasias such as SED or Morquio syndrome, where instability may develop over time. These, however, may be somewhat difficult to interpret in this population given the delayed ossification, odontoid hypoplasia, limited neck motion, and abnormal anatomy seen in many of these patients. Additionally, sometimes the bony landmarks used for measurement may be obscured by overlapping shadows cast by the mandible, occiput, and foramen magnum. Any patient with back or radicular pain, neurogenic claudication, incontinence, or objective neurologic findings (such as hypertonia, brisk reflexes, clonus, motor weakness) should be evaluated with an MRI [12]. The child’s gait is assessed by observing the child walk, run, and play [13]. Gait analysis can be helpful in these patients. Discussion with the family is critical to establish the goals of treatment as well as to manage expectations appropriately.
Imaging
A skeletal survey is often performed at the initial visit to identify the skeletal features that aid in diagnosis. At our institution, skeletal survey for skeletal dysplasia typically includes anteroposterior (AP) and lateral radiographs of the cervical, thoracic, and lumbar spine and AP view of the long bones of the upper and lower extremities as well as of the pelvis, hands, and feet. Cervical flexion-extension views are obtained in most dysplasias (except for achondroplasia). We add further radiographs as clinically indicated. AP and lateral full-length radiographs of the lower extremities (preferably weight-bearing views) are mandatory prior to surgical intervention. These allow for an evaluation of the overall alignment and location of deformities. It is also imperative to obtain dedicated weight-bearing radiographs of the specific joints to allow for appropriate deformity analysis (please refer to Chap. 2). The full-length radiographs alone will not always allow for an accurate quantitative determination of the magnitude of deformity. For example, the magnitude of ankle deformity can be misjudged based on full-length radiographs centered at the knee because of the parallax of the X-ray beam. Additional three-dimensional studies such as computed tomography and/or magnetic resonance imaging may be performed for detailed evaluation of bone and cartilage anatomy, measurement of torsional abnormalities, assessment of joint condition, etc. However, these are static studies and may not always reflect the alignment of the limb in conditions of dynamic loading (gait). We often perform a three-dimensional gait analysis in these patients as an adjunct to X-rays to aid in preoperative decision making. Such dynamic evaluation helps to quantify the forces across the various joints and also helps us compare pre- and postoperative function.
Anesthesia
Preparation of the patient for the surgical procedure is at least as important as the surgical procedure itself (Box 19.2). Given the fact that many of these patients have small and “difficult” airways, preoperative anesthesia consults and discussion of the various issues specific to that patient are very useful. There may be minor surgical procedures but there is no “minor anesthesia” for these patients. Anesthesia should be performed by an anesthesiologist familiar with various medical comorbidities associated with this patient population. Our institution has described a “difficult” airway management in these patients as one which requires two anesthesia providers when ventilating with a facemask. One provider applies the face mask while maintaining anterior mandibular displacement and cervical stabilization while the other ventilates with positive pressure [14]. Care must be taken to protect the neck in patients with cervical instability by using in-line cervical traction [15]. In addition, specialized tools such as video laryngoscope and fiberoptic intubation should be readily available in these situations. Given the fact that each anesthetic session poses a certain risk to the patient, we prefer to combine as many procedures as feasible under the same anesthetic.
Regional anesthesia is often used for pain control and to reduce the amount of narcotic needed during and after surgery. Caudal epidural analgesia is preferred over lumbar epidurals in patients with known vertebral anomalies, prior fusions, and thoracolumbar kyphosis that can co-exist with these conditions. Typically, caudal epidural may be administered to those patients 10 years of age and younger who undergo lower extremity osteotomies. Careful dosing of the epidural medications and regular neurovascular checks are essential to avoid missing the diagnosis of an early compartment syndrome.
Positioning
Positioning these patients is also critical as patients with severe kyphosis are at risk for developing paraparesis/paraplegia with prolonged supine position. The pathogenesis of this phenomenon is poorly understood at this time. Neuromonitoring should be considered in long procedures in such high-risk patients undergoing lower extremity surgery.
Box 19.2
Careful anesthetic technique, protecting the cervical spine and minimizing the number of anesthetic episodes, is important.
Consider neuromonitoring during nonspinal procedures in the supine position in patients with severe kyphosis to minimize risk of adverse neurologic events.
Careful preoperative planning and attention to addressing the bony and soft tissue deformities is key to improving outcomes.
Sequence of correction of deformities may vary in individual circumstances, but is usually proximal to distal.
Implant Size and Design
Implant size and design needs to be considered in preoperative planning. Some of these patients are extremely small (primordial dwarfism) and appropriately sized implants are critical to the successful execution of the preoperative plan. The popular commercially available precontoured implants will rarely accommodate the morphology of bones in patients with skeletal dysplasias. Given the poor bone quality in some of the patients, locking plate and screw constructs may be useful when performing acute corrections. Even while planning deformity correction with external fixators, implant selection should be kept in mind. For example, the appropriate fit of a Taylor Spatial Frame (Smith & Nephew; Memphis, TN, USA) may necessitate use of extra-extra short struts (which may need to be ordered preoperatively). Frequently, given the multifocal nature of the deformities, more than one osteotomy and therefore fixation options may be needed in the same bone. Having an appropriate inventory of instruments and implants saves the surgeon from frustration and improves patient outcome.
Methods of Deformity Correction
The principles of deformity correction in the dysplasia population are no different from those without dysplasias. However, the multifocal and multiplanar nature of the deformities, issues with size and quality of the bone, ligamentous laxity, and growth potential make deformity correction extremely challenging in these patients. Many of these patients have substantial delay in ossification, making planning and correction of deformities even more challenging. It has been demonstrated that the choice of osteotomy often times changes based on the results of intraoperative arthrography, particularly in patients under 8 years of age [16]. We use arthrography liberally during surgery to mitigate some of these issues. This helps us not only to visualize the cartilaginous anatomy but also to evaluate the dynamic stability of the joint with stress views in the operating room.
Deformity correction in these patients can be accomplished via acute or gradual methods.
Acute Correction
Acute methods of deformity correction include use of osteotomies with immediate correction and fixation via various methods. In general, these techniques follow the same principles as those patients without skeletal dysplasias. Care should be taken to be familiar with the various deformities associated with particular conditions (see Table 19.3). For example, genu varum is present in the majority of achondroplastic children by 5 years of age and 90 % of achondroplastic adults [17]. The genu varum can be secondary to distal femoral varus, lateral joint line opening, proximal and distal tibial varus and is nearly always associated with internal tibial torsion. Progressive varus, symptomatic gait abnormalities, lateral thrust, and occasionally cosmesis are our typical indications of genu varum correction. One or all of these deformities may be present, so careful preop planning must be done while planning the correction. The deformity in young children usually is due to proximal tibial varus, lateral joint line opening, and internal tibial torsion. These children can be successfully treated with a proximal tibial osteotomy with fibular shortening osteotomy via acute correction. Care must be taken to displace the proximal tibia in order to maintain a neutral mechanical axis and correct the typical internal tibial torsion. With this method, acceptable correction can be attained [18]. Recurrence is common in very young children, especially if there is undercorrection. It has been suggested that the preferred treatment for skeletally mature individuals with achondroplasia and distal tibial varus is an acute opening distal tibial osteotomy combined with a shortening distal fibula. Displacement usually is required to correct the mechanical axis [18]. The authors have typically used a shortening, derotational osteotomy to manage this deformity. With acute deformity correction, one can re-establish normal mechanical alignment, but not perform additional limb lengthening. In addition, acute corrections, particularly of the proximal tibia, have been associated with complications including peroneal nerve palsies, vascular injuries, and compartment syndromes [19].
Gradual Correction with Guided Growth
Gradual deformity correction is a powerful tool for angular realignment and/or lengthening in the skeletal dysplasia population. This can be done by way of guided growth techniques or external fixation methods. There is a paucity of literature that addresses the application of guided growth techniques in this unique population. However, we have demonstrated that growth modulation using a tension band plate and screw system or staples is an effective way to provide deformity correction in a variety of skeletal dysplasias [20]. It is a relatively simple surgery that has a low risk of damage to the physis or mechanical failure. We have also found that despite an abnormal epiphysis and metaphysis, the screw purchase has been reliable. An exception is pseudoachondroplasia where it can be difficult to achieve epiphyseal fixation. This technique can be used in very young patients [20]. Guided growth via hemiepiphyseal stapling in patients with multiple epiphyseal dysplasia (MED) has also been studied. In these children, stapling has been effective for angular deformity correction. However, the response of the physis after staple removal is unpredictable, necessitating avoidance of excessive overcorrection and close monitoring until skeletal maturity [21]. There are some skeletal dysplasias that are associated with extremely slow growth or have significant joint laxity, which can affect correction. Slow growth and a significant deformity is a combination that will likely lead to failure of correction when using guided growth treatment in such patients (Box 19.3).
Gradual Correction with External Fixation
Gradual deformity correction can also be accomplished using external fixators [22, 23]. This approach has two main advantages. Primarily, the multifocal and multiplanar deformities that are associated with skeletal dysplasias can be addressed at one surgery. Some of the gradual correction devices also allow for simultaneous multiplanar correction, addressing coronal, sagittal, and axial deformities without the need for complex osteotomies that are prone to error. Secondly, this method also allows for concurrent limb lengthening in this patient population with varying degrees of short stature. Patients must be counseled about their care and management preoperatively as limb lengthening can be associated with several complications [24, 25]. However, with appropriate instruction and care, external fixators are extremely useful for correction of most complex deformities. Currently, we prefer to use the Taylor Spatial Frame (Smith & Nephew; Memphis, Tennessee) for more complex deformities and a uniplanar external fixator for some of the less complex deformities.
Box 19.3
Growth modulation around the knee is a useful technique for deformity correction in patients with skeletal dysplasia, but the results are dependent on the growth potential and degree of associated ligamentous laxity.
Special inventory of implants of appropriate size is essential.
Plan procedures keeping in mind the natural history of the underlying skeletal dysplasia.
Controversies in Lengthening for Stature
Limb lengthening (without the correction of angular deformities) in short-statured individuals has been a subject of debate [24–29]. The achondroplastic population has been the most studied to date. The motivation to lengthen limbs in the skeletal dysplasia population has mainly been to improve functional disabilities associated with difficulty in locomotion [30]. Other concerns, particularly in the idiopathic short-statured patient, have been related to aesthetic, social, and psychological issues.
Medical and surgical treatments to address short stature in achondroplasia have been studied. Growth hormone (GH) administration has led to variable results [31]. In trials, early gains in height after commencement of GH treatment have been seen to varying degrees. However, the effects have not been as promising with continued administration. There are also concerns of aggravating the disproportionate nature of limb segment shortening. Surgical techniques for stature lengthening in achondroplasia have addressed the femora, tibiae, and humeri via distraction osteogenesis. This method has reliably been able to provide increases in height, but at a cost [24, 25, 27, 29].
The average gain in height through surgical limb lengthening in achondroplasia has been reported to be 18–23 cm, resulting in an average total patient height of 140 cm [24, 30, 32]. This does not completely ameliorate the disproportionate trunk height. There are several drawbacks to limb lengthening purely for increased stature, including prolonged treatment time and high complication rate (reported up to 100 %). It is unclear as to whether or not such bilateral limb lengthening improves the patient’s quality of life. Kim et al. showed that there was an improvement in self-esteem (using the Rosenberg self-esteem questionnaire), but there was no difference in physical or functional scores (using the SF-36 and AAOS lower extremity scores) when comparing achondroplastic patients who underwent lengthening versus those who did not undergo surgical treatment [24]. They studied 22 patients with achondroplasia who had tibial and femoral lengthening and compared them to a matched cohort with achondroplasia who did not undergo lengthening. They had 123 complications in 88 lengthened segments but reported that may of these were minor and did not need intervention. They felt that lengthening was a viable option given the improved self-esteem. The same group also looked at humeral lengthening in the achondroplasia population and reported that humeri tend to consolidate faster and have less fractures and angular malalignment compared to femoral lengthening. Extensive (more than 50 % of the length of the femur) lengthening of the femur results in higher incidence of fractures and joint issues. Extensive lengthening is also associated with physeal growth retardation, both femoral and tibial. Surgical strategies include bilateral tibial lengthening, lengthening of the femur and tibia on one side, crossed femur and tibia or all 4 segments simultaneously. Time in external fixators may be shortened by lengthening over an intramedullary nail or use of intramedullary lengthening techniques. The authors rarely perform stature lengthening.
There is a role for stature lengthening in the carefully selected patient who is well aware of the long and arduous nature of the process and the potential for significant complications. However, the patient must be counseled that the gain in height may not correlate to an improvement in quality of life [25].
Postoperative Considerations
There are several aspects of the postoperative course specific to the short-statured patients that should be taken into consideration. This is particularly true when utilizing external fixation for deformity correction. These children typically require more support because of their limited upper extremity reach. It is important to work with the physical and occupational therapists to provide appropriate assistive devices and strategies for activities of daily living.
The psychosocial aspect of deformity correction should not be overlooked in patients with skeletal dysplasias. These children may have preexisting self-image concerns because of their underlying conditions. With external fixators in place, these self-conscious feelings can be amplified. It may be useful to involve mental health professionals in the preoperative evaluation and postoperative care of these patients.
The skeletal dysplasia population often travels to referral centers for these complicated deformity corrections. We prefer to keep these patients locally during the timeframe of distraction and/or correction. This allows us to follow them in clinic on a weekly or biweekly basis and to appropriately address any complications that may arise. This oftentimes entails working with local or national charities, such as the Ronald McDonald House, for lodging and other necessities. In addition, the caregivers of these children need ample time to plan for the required postoperative stay if they are not locally based.
Planning for the Future
When planning these corrections, care must be taken to consider the long-term effects of such surgical interventions. Many individuals with skeletal dysplasias, such as multiple epiphyseal dysplasia (MED), spondyloepiphyseal dysplasia (SED), pseudoachondroplasia, diastrophic dysplasia, and Morquio syndrome (MPS IVA), are predisposed to premature osteoarthritis. These patients often need total joint arthroplasty (TJA) at a relatively young age. This must be taken into account when performing osteotomies that may make TJA more difficult. The surgeon needs to consider various obstacles when performing TJA in these patients. For instance, in total knee arthroplasty, customized implants and constrained designs are often needed because of patient’s short size and a lack of ligamentous constraints associated with the underlying pathologies [33, 34]. When considering total hip arthroplasty, the surgeon needs to evaluate the need for potential acetabular augmentation secondary to bony deficiency, the possibility of extensive soft tissue releases because of contractures, presence of tortous and narrow proximal femoral intramedullary canals, and the potential for needing custom implants due to small stature [35]. When proper preoperative planning is executed, good results can be achieved with total joint arthroplasty in patients with skeletal dysplasia, though complication rates can be high [33, 35].
Specific Skeletal Dysplasias and Their Associated Deformities
Achondroplasia
Achondroplasia is the most frequently encountered form of skeletal dysplasia with an incidence of approximately 1 in 10,000 live births [36]. This results from a mutation in the FGFR3 gene. This over-activity of FGFR3 results in abnormalities in endochondral ossification, whereas intramembranous ossification is not affected. This therefore results in involvement of the base of the skull (resulting in foramen magnum stenosis) and the extremities. There are predictable patterns of deformity in this population. In the upper extremity elbow flexion deformities are common and often associated with distal humeral recurvatum. The severe rhizomelia seen in these individuals can result in marked limitation in reach and humeral lengthening can improve function in these patients. In the lower extremity, hip flexion and knee deformity are often noted. The most commonly addressed deformity is genu varum, which is often associated with internal tibial torsion and occasionally genu recurvatum. A common misconception is that uncorrected genu varum in children with achondroplasia results in knee osteoarthritis later in life. In fact, osteoarthritis is rare and the knee joint is usually not a source of functional limitation in these patients. Spine problems such as central stenosis of the lumbar segments often result in limited function. The etiology of genu varum is unclear. Several mechanisms have been proposed, including ligamentous laxity, obesity, asymmetric growth of the proximal tibial physis, and asymmetric growth of the fibula relative to the tibia [37–39]. As previously mentioned the varus deformity can exist in the distal femur, the knee joint, and the proximal and distal tibia. Indications for surgical correction of genu varum and internal tibial torsion in these children include knee pain, progressive deformity, lateral thrust during gait, and rarely, cosmesis. Genu valgum, though uncommon, may also be seen in some patients. However, the valgus deformity is rarely severe enough to warrant surgical correction.
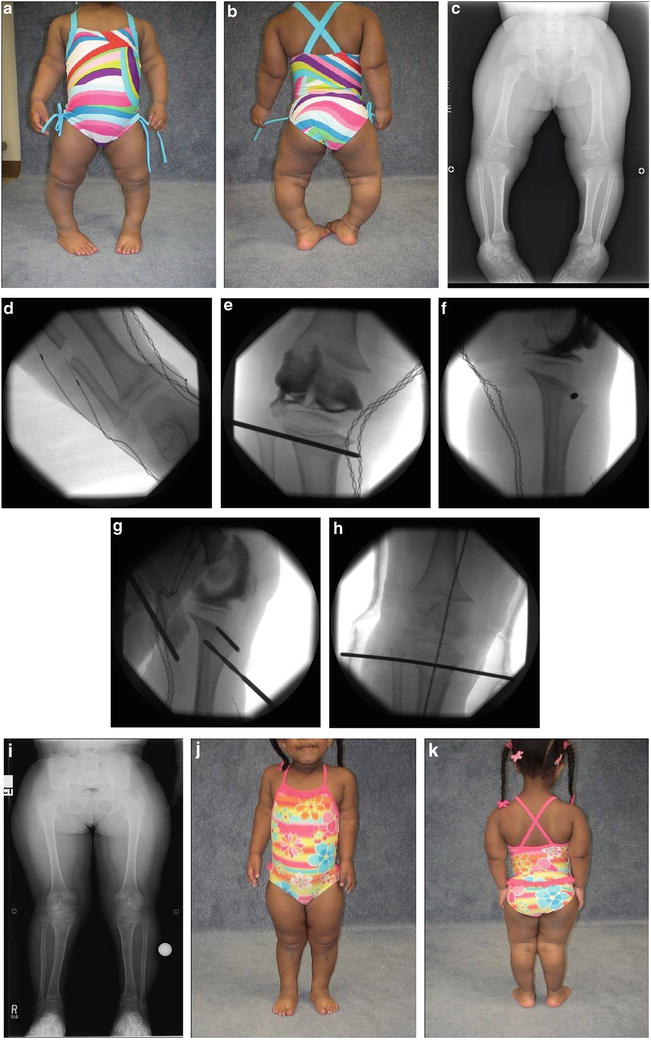
Several techniques for correction of genu varum in achondroplastic patients have been described previously. Fibular epiphysiodesis or shortening may be useful in young patients (5–8 years old) with mild deformity [18, 40]. However, long-term data on this technique is lacking. Acute correction in young children with an oblique proximal tibial osteotomy (Fig. 19.1a–k), simultaneously correcting the tibial varus and internal rotation, has achieved reliable results with a low recurrence rate as long as the joint line and mechanical axis are brought to a neutral position [41, 42].