Lesions of The Liver
Hepatic tumors in children are relatively rare. The most common malignant hepatic neoplasms are not primary tumors, but rather metastatic lesions such as Wilms tumor, lymphoma, and neuroblastoma.1 Primary liver tumors comprise between 1–4% of all solid tumors in children. Malignant hepatic tumors occur at a rate of about 1 to 1.5 per million children per year.1,2 However, ten primary liver masses occur with some frequency in the pediatric age group Five of these occur only in children: infantile hepatic hemangiomas, hepatoblastoma, mesenchymal hamartoma, rhabdomyosarcoma of the biliary tract, and undifferentiated embryonal sarcoma (Table 67-1). The age distribution for hepatic masses is distinctive, with hepatoblastoma and infantile hepatic hemangioma occurring most commonly in the first two years of life, and hepatocellular carcinoma and focal nodular hyperplasia occurring most commonly after age 5 years (Table 67-2).1
TABLE 67-1
Hepatic Tumors in Pediatric Patients, Birth to 2 Years (AFIP 1970–1999)
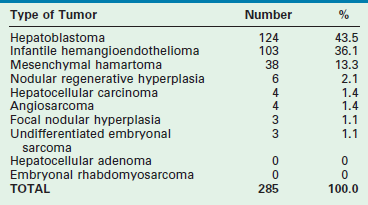
Reprinted from Stocker JT. Hepatic tumors in children. In: Suchy FJ, Sokol RJ, Balistreri WF, editors. Liver Disease in Children. 2nd ed. Philadelphia: Lippincott Williams & Wilkins; 2001. p. 915.
TABLE 67-2
Hepatic Tumors in Pediatric Patients, 5 to 20 Years (AFIP 1970–1999)
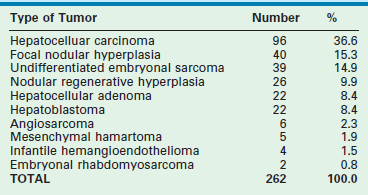
Reprinted from Stocker JT. Hepatic tumors in children. In: Suchy FJ, Sokol RJ, Balistreri WF, editors. Liver Disease in Children. 2nd ed. Philadelphia: Lippincott Williams & Wilkins; 2001.
Couinaud’s elegant description of the segmental anatomy of the liver has allowed hepatic operations to evolve to a level at which they can be performed with an acceptable morbidity and mortality (Fig. 67-1).3,4 The cumulative experience with hepatic resection and hepatic transplantation has allowed the development of techniques for both subsegmental and multisegmental resections of the liver in children. With the continued expansion of knowledge about these tumors, reasonable surgical and medical management plans can be devised.5
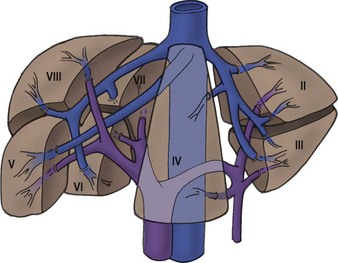
FIGURE 67-1 The segmental hepatic anatomy as defined by Couinaud. A comprehensive understanding of the hepatic segmental division is necessary for successful hepatic resection. (From Couinaud C. Surgical anatomy of the liver: Several new aspects. Chirurgie 1986;112:337–42; Couinaud C. The anatomy of the liver. Ann Ital Chir 1992;63:693–7.)
Benign Hepatic Tumors
Infantile Hepatic Hemangiomas
Incidence
Infantile hepatic hemangioma (IHH) is the most common benign solid hepatic tumor in children, comprising about 16% of all pediatric liver tumors.1 It also is the most common liver tumor in the first year of life. Almost all children with IHH are seen initially before age 6 months, and the majority are encountered in the first 2 months.6,7 Historically, a slight female predominance has been found, but this finding has not been uniformly seen.8
Clinical Presentation
IHHs can be either single lesions that can expand to a massive size or a multinodular infiltrative mass. Occasionally these lesions are asymptomatic and present as an abdominal mass or abdominal distention. Hepatic hemangiomas can also be found in association with congenital syndromes such as Osler–Weber–Rendu, Klippel–Trénaunay–Weber, and Ehlers–Danlos. IHH has also been reported in association with Beckwith–Wiedemann syndrome, diaphragmatic hernia, trisomy 21, transposition of the great arteries, and extranumerary digits.9,10
Infants with IHH can present with significant symptoms including hepatomegaly, high-output congestive heart failure, respiratory distress, and anemia. Occasionally these infants present with the Kasabach–Merritt syndrome that is characterized by acute thrombocytopenia, a microangiopathic hemolytic anemia, and a consumptive coagulopathy.11 This syndrome can be life threatening and requires aggressive supportive treatment, as well as treatment of the hemangioma itself. Fortunately, the Kasabach–Merritt syndrome occurs infrequently and is usually associated with IHH that have rapid growth to a diameter of 5 cm or more. No cases have been reported in association with smaller tumors.12
The Boston Children’s Hospital Vascular Anomalies Center has recently made a proposal to classify IHH as either focal, multifocal, or diffuse.13 Focal lesions tend to be asymptomatic, are rarely associated with cutaneous hemangiomas, and often are identified on prenatal ultrasound (US). Focal lesions can have high-flow shunts and can have an associated low grade anemia or thrombocytopenia. Multifocal lesions also can be asymptomatic. They are often found on visceral imaging that is performed when evaluating patients with multiple cutaneous hemangiomas. These extrahepatic hemangiomas can occur at multiple distant sites including the skin (45%), lung (10%), pancreas, lymph nodes, and bone.14,15 Some of these multifocal IHH lesions, however, are associated with high-output cardiac failure from either intralesional or portovenous shunting. The diffuse lesions present with near total replacement of the hepatic parenchyma with multiple hemangiomas which can result in massive hepatomegaly, abdominal compartment syndrome, or significant respiratory compromise. This lesion is often associated with severe hypothyroidism due to the overproduction of type III iodothronine deiodinase.16,17 The hypothyroidism can be severe enough to cause low-output cardiac failure or significant mental retardation. Interestingly, there has not been a patient reported with diffuse IHH who has developed high-output cardiac failure. Other symptoms that can occur in patients with IHH include jaundice, failure to thrive, respiratory difficulties, or poor feeding. Historically, as many as 50–60% of infants with IHH have symptoms of congestive heart failure that seems to be age related.18,19 Neonates with a focal hemangioma tend to present with high-output heart failure at birth, whereas infants with multifocal lesions tend to present with heart failure between the ages of 1 and 16 weeks.
In patients with IHH, the hepatic transaminase levels and occasionally the α-fetoprotein (AFP) level can be elevated. The cause of this AFP elevation is unclear. Moreover, an elevated AFP level in neonates must be interpreted with some caution. The AFP level is normally elevated in neonates and it does not decrease to adult levels until about 6 months of age.15 When there is a significant elevation of the AFP level, however, hepatoblastoma must be excluded by either imaging studies or biopsy of the lesion.20
A significant incidence of placental abnormalities has recently been reported in very low birth weight infants (<1500 g) who present with infantile hemangiomas.21 These researchers discovered a variety of anomalies that could potentially lead to the shedding of placental cells into the fetal circulation. If fetal hypoxic stress is also present, these placental cells could be exposed to an increased level of angiogenic factors that could then lead to increased endothelial cell or placental cell proliferation in the postnatal period with the subsequent development of an IHH.
Imaging
The ultrasound evaluation of IHH can be highly variable. Solitary lesions can have a heterogeneous echogenicity, and the Doppler spectral analysis can show a variety of flow patterns. Multifocal lesions, however, tend to be more uniform in their appearance and are seen as echolucent nodules associated with a high-flow vessel.22 On computed tomography (CT) with intravenous contrast, classically the lesions either enhance diffusely or show rim enhancement that is followed by gradual filling of the center of the lesion (Fig. 67-2).19,23,24 In one series, the CT enhancement pattern was correlated to the size of the lesions. Lesions less than 1 cm enhanced homogeneously in the arterial phase. Lesions greater than 2 cm demonstrated peripheral rim enhancement and those in between 1–2 cm showed a mixed enhancement pattern in the arterial phase (Fig. 67-3).25 Unfortunately, this ‘classic’ enhancement pattern is not always present in IHH which can make the radiologic diagnosis difficult.
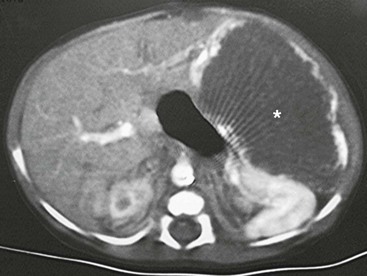
FIGURE 67-2 CT scan after intravenous administration of a contrast agent shows a large hemangioendothelioma (asterisk) with peripheral enhancement in the left lateral segment.
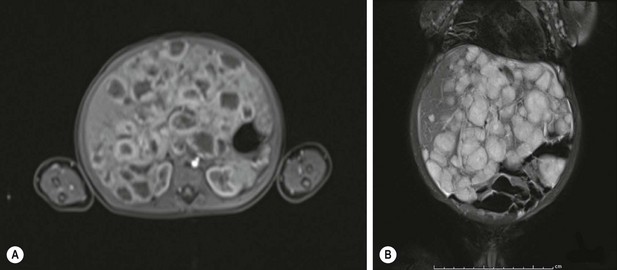
FIGURE 67-3 Infantile hepatic hemangioma: diffuse form. (A) An MRI in the arterial phase showing rim enhancement of the hemangiomas after injection with gadoxetate disodium (Eovist). (B) The T2-weighted image showing the same liver that is filled with hemangiomas.
Magnetic resonance imaging (MRI) is emerging as the single most useful modality to show both the location of the hemangioma and its flow pattern and structure.26,27 The addition of intravenous gadolinium and a gradient-recalled-echo sequence to the MRI enhances its utility.
Focal lesions on MRI are well defined and hypointense to the liver on T1 images and hyperintense on T2-weighted images. Gadolinium demonstrates peripheral enhancement with variable central enhancement that is related to the amount of hemorrhage or thrombosis that is present in the lesion. Multifocal and diffuse lesions tend to show similar MRI findings except that there are multiple lesions present. Recently, however, there has been a case report of a hypervascular hepatoblastoma that had an MRI pattern that was identical to a hemangioendothelioma.28 Therefore, again, radiology alone cannot reliably distinguish between benign and malignant lesions.
IHH also has been seen in conjunction with both focal nodular hyperplasia and hepatic mesenchymal hamartoma.29,30 These associations are important to remember during the radiologic evaluation of a child with multiple hepatic masses.
Histology
Microscopically, the histologic pattern has been divided into type 1 and type 2 lesions. A type 1 lesion consists of a single layer or, occasionally, several layers of flat endothelial cells on a supporting fibrous stroma.31 In a type 2 lesion (20% of cases), the endothelial cells are pleomorphic, larger, and more hyperchromatic than those seen in type 1 tumors. Also, there are poorly formed vascular spaces that often show tufting or branching. It is thought that the histologic picture of the type 2 lesion is more characteristic of a rapidly proliferating process. The histological differentiation between a type 2 lesion and an angiosarcoma can be difficult.14,32 The addition of a histologic stain for the marker Glut 1 can be helpful in making the diagnosis of IHH.9 Focal lesions do not stain positive for Glut 1, while multifocal lesions will be positive for this marker.33,34 Well-preserved bile ducts can frequently be seen near the periphery of a type 1 lesion, whereas bile ducts are absent in a type 2 lesion.
Treatment
The life cycle of infantile cutaneous hemangiomas is divided into three stages. The first starts usually after birth and is a characterized by a rapid growth phase that lasts about 9 to 12 months. In the second phase, the hemangioma begins the process of involution. This process can take anywhere between 5 and 7 years. The last phase is the involuted phase where the hemangioma is permanently replaced by fibrofatty tissue.13 Hepatic hemangiomas also tend to follow a similar life cycle. The therapy for IHH depends on the severity of the presenting symptoms and the size of the mass(es).
Asymptomatic lesions are monitored, and no specific therapy is instituted until symptoms occur.11,35 As part of the evaluation of the asymptomatic patient with multifocal hemangiomas, imaging studies of the brain and chest should also be performed to make sure there are no associated intracranial or pulmonary lesions. In addition, all patients with multifocal lesions should be screened for hypothyroidism. Focal IHH are felt to follow a unique clinical course that is similar to the clinical course of a cutaneous rapidly involuting congenital hemangioma where involution is seen by 12 to 14 months of age.36
Infants who present with congestive heart failure, coagulopathy, or respiratory compromise require intervention. Mortality rates in these patients have been reported to range from 17–35%, with some reports of death in as many as 90% of those who are severely symptomatic.37–39 Risk factors for death include congestive heart failure, jaundice, multiple tumor nodules, and the histologic absence of cavernous differentiation.
If there is hemodynamic instability, respiratory compromise, or coagulopathy, then therapy directed toward the hemangioma is needed. The usual initial treatment for a symptomatic lesion is prednisone or prednisolone at a dose of 2–3 mg/kg/day. The symptomatic response rate to corticosteroids is reported to be about 45%.40,41 If steroids are ineffective, then some IHHs have shown a response to vincristine at a weekly dose of 1–2 mg/m2 for two weeks.12 Labreze et al. have reported on the use of propranolol (2 mg/kg/day) for the treatment of severe infantile capillary hemangiomas with excellent results.42 Marsciani et al. have successfully used the combination of propranolol (1 mg/kg/day followed by 2 mg/kg/day) and steroids in the treatment of a 2-month-old child with diffuse IHH.43 They noted a dramatic decrease in liver size only one week after the addition of the propranolol. Another agent that has been reported to be possibly effective in IHH is curcumin, which is derived from the spice tumeric. Curcumin has antiangiogenic activity and has been tested with some success in a variety of tumors.44 Hassell et al. described its apparent successful use in a 6 month old with a multifocal IHH.45
Resection should be considered if the hemangioma is confined to a single lobe. In this situation, a survival rate of 92% has been reported, even if the clinical situation is complicated by congestive heart failure.32,46 However, some authors feel that resection is rarely needed if both pharmacotherapy and embolization are aggressively pursued.13
Embolization is an important part of the therapy of symptomatic hemangiomas.47,48 In order to decrease the chance of the IHH recurring, it is important that both the arterial and portal vascular supply to the IHH are occluded as distally as possible.11,19 After successful embolization, a rapid improvement in the clinical course usually occurs within five days. However, there may not be any associated change in the size of the hemangioma itself.47,48 Embolization should be considered early in the treatment course in those infants who are in significant cardiac failure. Unfortunately, embolization has not been helpful in infants with diffuse disease because of the absence of significant shunting.
Finally, in infants in whom other modes of treatment have failed, liver transplantation has been used successfully for severe congestive heart failure or unremitting coagulopathy (or both).49 The infants that will most commonly need to be considered for a liver transplant will be those who have the diffuse IHH subtype. Infants who experience rapid clinical deterioration in the postnatal period have a high mortality after liver transplantation so careful consideration needs to be given to their candidacy.50
The Vascular Anomalies Center at Boston Children’s Hospital has suggested a treatment algorithm for IHH.13 All asymptomatic lesions should be monitored with ultrasound until resolution. Symptomatic lesions should be treated with steroids. If there is no response, then the hemangioma should be embolized. Infants with diffuse disease should have a TSH checked and be started on steroids. If abdominal compartment syndrome is present, then the infant needs to be evaluated for a liver transplant in case there is no response to steroids.
Malignant transformation of an IHH to an angiosarcoma has been reported in older children.18,51 For this reason, patients who are asymptomatic or who become asymptomatic after therapy must be monitored for complete anatomic resolution of their hemangioma. Resection of any residual lesion should be strongly considered.
Mesenchymal Hamartoma
Incidence
Mesenchymal hamartoma is reported to be the third most common hepatic tumor and the second most common benign tumor in children.1 Of all benign hepatic lesions, mesenchymal hamartomas account for between 18–29% of these tumors.52,53
Epidemiology
The reasons for the development of a mesenchymal hamartoma are unclear. One theory is that it results from abnormal development of the primitive mesenchyme, which appears to occur at the level of the hepatic ductal plate, causing abnormal bile ducts.54 This concept is supported by the histologic finding of a combination of cystic, anaplastic, and proliferating bile ducts, as well as the presence of multiple portal vein branches, within the tumor. It is postulated that the tumor then develops a cystic component as a result of obstruction and dilatation of lymphatics or from occluded bile ducts (or both). The tumor enlarges during infancy as the cystic areas increase in size. Most of the proliferative growth appears to occur before or just after birth because no observable mesenchymal mitotic activity is visible on histologic sections of the tumor.55
A second theory is that the lesions are reactive rather than developmental.56 It is hypothesized that an abnormal blood supply to an otherwise normal hepatic parenchyma causes ischemic necrosis, leading to reactive cystic changes within that portion of the liver. This theory is supported by the findings that hamartomas often have a necrotic center, are often attached to the liver by only a thin pedicle, and rarely are found centrally in the liver.
The third theory suggests that a mesenchymal hamartoma is a proliferative lesion. This theory is supported by several findings. Increased fibroblast growth factor-2 (FGF-2) staining has been noted in the proliferating hepatic stellate cells adjacent to the mesenchymal hamartoma.57 Both the stellate cells in the liver and the spindle cells in the mesenchymal hamartoma tissue strongly express molecules of the FGF-receptor family. It is speculated that a local increase of FGF-2 secretion could stimulate the growth of the spindle cells to form the mesenchymal hamartoma. FGF-2 also is a potent angiogenic factor that could contribute to the intense vascularization seen within some of these lesions. A recent study has identified that the spindle cells that make up the predominant cell line in a mesenchymal hamartoma appear to be derived from hepatic stellate cells.58 A possible genetic cause for these abnormalities has been proposed as well. Cytogenetic studies of these tumors have documented several abnormalities including translocation/deletion of chromosome19q13 or the loss of heterozygosity due to multiple monosomies. The resulting dysregulated imprinting may be an additional cause for a mesenchymal hamartoma.59–63
Clinical Presentation
The widespread use of prenatal imaging has led to the detection of hepatic masses before birth.15 Cases of hepatic mesenchymal hamartoma that were diagnosed prenatally have been described.64,65 One of the unique characteristics of a prenatal mesenchymal hamartoma is that it can be solid as well as cystic. Unfortunately, the prognosis for these antenatally diagnosed neonates is often poor with a reported mortality rate of 29%.66 This mortality is related to: (1) the development of congestive heart failure from compression of the inferior vena cava or the umbilical vein by the tumor mass; or (2) the development of hydrops that can occur from fluid losses into cysts or decreased albumin production by the liver. Thus, it may be best to deliver these fetuses before fetal hydrops develops.65 Another series reported the use of repeated intrauterine aspiration of the cysts until the infants could be delivered and definitive treatment initiated.67 While this therapy is appealing, there currently is insufficient evidence to recommend its widespread use.66
In the neonate, these lesions can have a varying presentation. High-output cardiac failure, pulmonary hypertension, and disseminated intravascular coagulopathy have been reported in neonates with highly vascular mesenchymal hamartomas.68–70 Respiratory distress secondary to a large hepatic mass impinging on the diaphragm has also been described.65 Unfortunately, the prognosis for infants with a perinatal diagnosis is also poor with a reported mortality of 35%.66
The presentation of a mesenchymal hamartoma in the older child is usually that of progressive abdominal distention or an abdominal mass (or both). There is a significant right-sided predilection for these masses, and they tend to be somewhat more common in males.1 Occasionally, the associated symptoms of nausea and vomiting can occur that are secondary to the compression of the stomach and intestine by the expanding mass.
On physical examination, abdominal distention or a palpable abdominal mass is most common. The mass tends to be nontender and fixed. Laboratory studies almost always are normal, including liver function studies. The AFP level can be moderately elevated and it returns to normal after resection. However, it is important to remember that patients have been treated with chemotherapy for hepatoblastoma until a tumor biopsy was performed and a mesenchymal hamartoma was subsequently diagnosed.71,72
Imaging
CT, ultrasound, and MRI have all been used for diagnosis. On CT and ultrasound, a multiseptated, multicystic, anechoic mass is usually located either in the periphery or scattered throughout the liver.73,74 Occasionally the mass is pedunculated. Calcification within the tumor is unusual, but has been reported so the presence of calcifications within a tumor does not exclude a mesenchymal hamartoma.75,76 MR angiography has proven useful both in the diagnosis and planning of resection.77,78 The finding of a small round hyperechoic parietal nodule on ultrasound is usually highly sensitive for making the diagnosis.79
Histology
Mesenchymal hamartomas typically are large, well-circumscribed tumors that measure at least 8–10 cm in diameter (Fig. 67-4). Seventy-five per cent of these tumors occur in the right lobe of the liver, and only 3% are seen in both lobes of the liver. On cut section, multiple cysts can measure from a few millimeters to 15 cm in diameter. These cysts are filled with either serous or viscous fluid separated by loose fibrous and myxoid tissue (Fig. 67-5). The surrounding tissue is yellow-tan to brown and is loose to moderately dense.
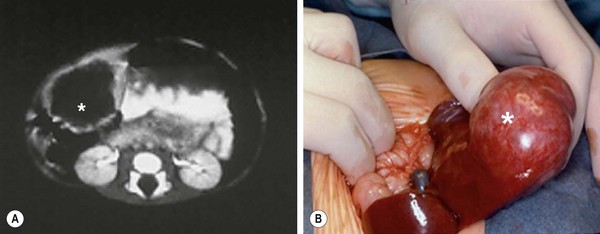
FIGURE 67-4 This young child presented with a palpable right upper abdominal mass. (A) CT scan shows an anechoic mass (asterisk) in the periphery of the liver. (B) At operation, the mass (asterisk) was found to be pedunculated and emanating from the right lobe of the liver. This hamartoma was easily removed.
Microscopically, the tissue consists of a mixture of bile ducts, liver cell cysts, and mesenchyme. The cysts may be dilated bile ducts, dilated lymphatics, or amorphous cysts surrounded by mesenchyme. In older patients, the cysts may be lined with cuboidal epithelium (Fig. 67-6). Elongated or tortuous bile ducts surrounded by connective tissue are unevenly distributed throughout the mesenchyme. Typically the hepatocytes appear normal, and they are not a predominant part of the pathologic process. The bile ducts in the periphery of the lesion seem to be undergoing active proliferation.1
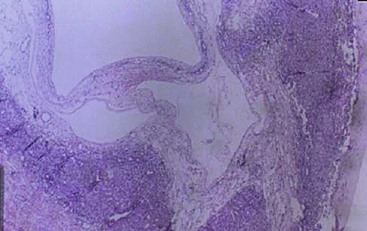
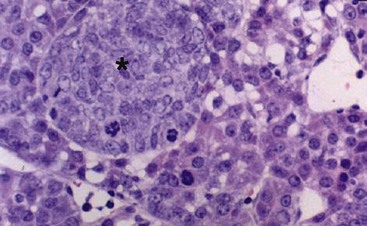
FIGURE 67-6 Light microscopy of mesenchymal hamartoma showing a cyst lined with cuboidal epithelium.
Despite the fact that the majority of these tumors are localized, there have been reports of these tumors being multifocal.63 This may account for the occasional recurrences that are seen after resection of the primary tumor.
Treatment
Various management strategies have been used for these lesions. Because they are sometimes encapsulated, enucleation may be possible. Very large, bilobar tumors that are not amenable to resection can be marsupialized into the peritoneal cavity, but recurrence after marsupialization can occur. If marsupialization is performed or the resection is incomplete, careful, long-term follow-up is important because of the risk of recurrence or the development of undifferentiated embryonal sarcoma.80 Complete excision of the lesion with a margin of normal liver is curative (including the use of liver transplantation for large, bilobar lesions) and is the recommended therapy.81,82 For massive lesions with multiple cysts, one group reported the use of ultrasound-guided, intraoperative aspiration of the cysts.83 This technique substantially reduced the size of the mass and made the resection much easier. Spontaneous involution of these lesions has been reported, but is unusual.84
There is now strong evidence that an undifferentiated embryonal sarcoma of the liver can develop within a preexisting mesenchymal hamartoma.63,85–88 This association has occurred both synchronously and metachronously. The evidence for a direct link between a mesenchymal hamartoma and an undifferentiated embryonal hepatic sarcoma comes from the simultaneous finding of both tumors arising within the same mass. Moreover, aneuploidy and similar chromosomal abnormalities involving chromosome 19q13 have been reported in both a hepatic mesenchymal hamartoma and an undifferentiated embryonal sarcoma.60,61,89,90
Focal Nodular Hyperplasia
Incidence
Focal nodular hyperplasia (FNH) accounts for about 10% of the hepatic tumors in children.1 The reported age range is between 7 months and 16 years, with a mean of 7 years, and there is a slight female predominance.91 The majority of these tumors are discovered incidentally.91,92 The most common symptom is abdominal pain, but some patients describe decreased appetite, an abdominal mass, weight loss, or a combination. Hepatomegaly is a common finding, and liver function abnormalities are often present.
FNH has been seen in association with a variety of different conditions and situations, including previous liver trauma, other liver tumors, hemochromatosis, Klinefelter syndrome, the use of itraconazole, after a successful Kasai procedure, after liver transplantation, and with cigarette smoking.93–100
The etiology of FNH is not certain, but the evidence suggests that it may be a congenital vascular abnormality. These lesions have a single feeding artery and there is an absence of bile ducts or veins in the lesion. The large artery causes a hyperperfused area of the parenchyma with subsequent growth of the liver tissue around the artery.101 In addition, FNH has been associated with other vascular lesions such as hemangiomas, arteriovenous malformations, and hereditary hemorrhagic telangiectasia.102,103 Further evidence that FNH is a reactive lesion secondary to vascular anomalies comes from a study in which an increase in the angiopoietin ratio (ANGPT1/ANGPT2) was seen.104 The ANGPT1 and ANGPT2 genes are necessary for normal vascular development. In FNH, an overexpression of the ANGPT1 gene and an absence of the antagonistic ANGPT2 gene lead to uncontrolled and disorganized vascular development. Although it is not clear that this is the exact pathogenesis of FNH, it certainly suggests that this genetic imbalance may play a causative role. FNH can also develop from an acquired abnormality of the hepatic vasculature. Thrombosis of either a hepatic artery or portal venous branch can initially cause ischemia of a portion of the liver followed by recannulation and reperfusion, which leads to hepatocyte proliferation.105
Controversy exists about the relation between oral contraceptive use and the development of FNH. In a case–control study, it was noted that neither menstrual nor reproductive factors correlated with FNH risk. However, oral contraceptive use was a significant risk factor in the development of FNH.99 As the use of oral contraceptives also appears to be associated with hepatocellular adenomas, a history of oral contraceptive use does not help in distinguishing between these two entities.99
In children, an association has been noted between the congenital absence of the portal vein (Abernathy syndrome) and FNH.106–108 In addition, these patients have an increased incidence of other solid tumors such as hepatoblastoma, hepatocellular carcinoma, and hepatocellular adenoma.109,110 FNH also has been seen, albeit less frequently than hepatocellular adenoma, in patients with glycogen storage disease (GSD) type 1.108
Over the last six years there has been an increasing awareness of the occurrence of FNH in oncologic patients who have completed their therapy. The reported incidence of FNH in the general pediatric population is 0.02% but is 0.45% in the postoncology treatment population.111 As opposed to nononcologic patients where the FNH is usually solitary, post-treatment oncologic patients frequently have multiple FNHs. The cause of these post oncologic FNHs is not known, but is felt to be secondary to alterations in liver perfusion that occur as the result of the chemotherapy or radiation that these patients receive.105,112 The development of hepatic mass(es) in an oncology patient leads to a diagnostic dilemma between an FNH or a recurrent tumor. One of the higher risk groups for developing an FNH after therapy are patients who were treated for neruoblastoma.111–116 There also seems to be an increase in the development of FNHs in children who have received a hematopoietic stem cell transplant.117–119 Therefore, a liver lesion that occurs after treatment of a previous cancer does not always mean that there has been a recurrence of the primary tumor. A biopsy of the lesion should always be done before the initiation of further therapy.120
Imaging
The diagnosis of FNH often requires the use of multiple different imaging modalities. On CT, the classic findings are early enhancement of the lesion and the presence of a central scar (Fig. 67-7).121 Unfortunately, this pathognomonic association is not often seen.122,123 Additional imaging modalities include single-photon emission radionuclide scans with either radiolabeled sulfur colloid or hepatobiliary iminodiacetic acid (HIDA) imaging. These studies usually demonstrate hypervascularization, increased tumor tracer uptake, and a central cold area.124–126 Technetium-99m sulfur colloid scanning can also be useful in distinguishing between FNH and a hepatic adenoma. FNH lesions take up the tracer because the Kupffer cells in the FNH take up the colloid but hepatic adenomas do not take up tracer because they lack Kupffer cells.127 MRI also has been useful when coupled with either gadolinium enhancement or the use of liver-specific contrast agents such as mangafodipir trisodium or iron oxide. During the arterial phase of dynamic contrast enhancement, an FNH will demonstrate distinct hypervascularity.128 These contrast agents can also help diagnose an FNH by allowing better identification of the central scar.129,130
Histology
FNH classically is characterized by nodular architecture, a central or eccentric scar containing malformed vessels that resemble an arteriovenous malformation, and a variable amount of bile duct proliferation (Figs 67-8 and 67-9).131,132 FNHs always occur in the setting of a noncirrhotic liver.
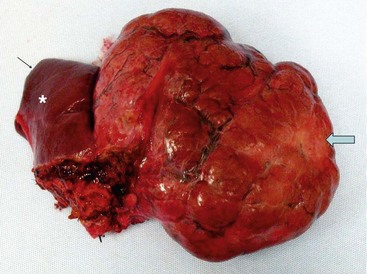
FIGURE 67-8 A large focal nodular hyperplasia lesion was resected. External scarring (arrow) is seen in the lesion. An asterisk marks normal liver.
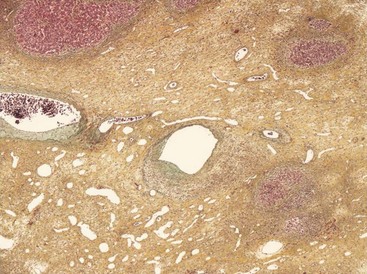
FIGURE 67-9 Light microscopy of a focal nodular hyperplasia showing a central scar containing abnormal blood vessels.
Histologically, the classic form of FNH with a central scar accounts for about 80% of the lesions. Twenty per cent are nonclassic where the FNH lacks either the nodular architecture or the presence of the malformed blood vessels. These nonclassic lesions are subdivided into three histologic categories: the telangiectatic form, the mixed hyperplastic form, and the adenomatous form.133 These nonclassic categories always lack a macroscopic scar and all three forms can be difficult to distinguish from and may be related to a hepatocellular adenoma.134 Immunohistochemical staining for cytokeratins 7 and 19 along with staining for neuronal cell adhesion molecule (CD56) has shown to be very helpful in distinguishing between FNH and hepatocellular adenoma.134 Hepatocellular adenomas have been reported to be present in association with FNH in about 4% of the cases.131
Recently, there has been a case report of what appears to be malignant transformation of an FNH to a fibrolamellar hepatocellular carcinoma.135 Also, FNH has been reported to occur in association with a well-differentiated fibrolamellar hepatocellular carcinoma.135,136 This observation is important to remember in patients who have multiple hepatic nodules.137,138
Treatment
The treatment of FNH depends on the clinical situation. If the diagnosis is certain, and the patient is asymptomatic, the consensus is that these patients can be followed with serial ultrasound to ensure that no progression of the lesion occurs.91,122 Percutaneous biopsy can be helpful in the diagnosis.139 However, if the patient is symptomatic, if the lesion is greater than 5 cm, if progression of the mass is seen, or if the diagnosis is unclear, then a biopsy or a resection of the lesion is recommended.140–143 Due to the association of FNH with hepatocellular carcinoma, patients who are expectantly managed must have serial evaluations to ensure that no progression occurs. Moreover, they need to be monitored for the development of other hepatic lesions.
Several reports have noted a 40–50% regression rate in cases of FNH that have been monitored.144,145 In the pediatric population, the true incidence of regression is not known due to the lack of long-term follow-up studies; however, it may be much lower than in the adult population.143 Regression of FNH is more likely if the use of oral contraceptives ceases.146,147
In two symptomatic patients in whom the FNH was in an area that was thought to be difficult for resection, arterial embolization either with Lipiodol and absorbable gelatin foam (Gelfoam) or iodized oil and polyvinyl alcohol resulted in a significant regression in the size of the mass.148–150
Hepatocellular Adenoma
Incidence
Hepatocellular adenoma is a very rare hepatic tumor in children, comprising only about 4% of all solid liver tumors.1 It is most commonly seen in women in their 20s and is associated with the use of oral contraceptives.
Imaging
Hepatic adenomas are solitary lesions in most cases, but occasionally two to three adenomas can be seen in one patient.149,151,152 On ultrasound, these lesions can have a variable appearance, depending on the tumor composition. They can have a hyperechoic, hypoechoic, or a mixed echoic pattern depending on whether it is a simple adenoma, an adenoma with fatty metamorphosis, or an adenoma with hemorrhagic necrosis.149
On CT, the adenoma can either be isoattenuating relative to the normal liver or hyperattenuating (due to the presence of fat). They are usually sharply marginated and nonlobular, but can be encapsulated or calcified in some patients.153 Hyperattenuated areas often correspond to areas of recent hemorrhage. On CT scan with intravenous contrast, a hypodense discrete lesion will show either arterial-phase enhancement or peripheral enhancement secondary to large subcapsular feeding vessels.154
On MRI, these lesions are either hypo- to hyperintense on T1-weighted images with uniform signal loss on out of phase T1-weighted views. On T2 images, the lesions are isointense to slightly hyperintense and gadolinium enhancement is maximal during the arterial phase with rapid fading.154 The finding of central hemorrhage or necrosis on CT scan helps differentiate hepatocellular adenoma from FNH.
Associated Conditions
Hepatocellular adenomas were extremely rare prior to 1960, which corresponds to the year in which oral contraceptives were first introduced.155 In women who have never used oral contraceptives, the annual incidence of hepatic adenoma is estimated to be about one per million. The duration of oral contraceptive use is directly related to the risk of developing a hepatic adenoma. The use of contraceptives for 5 to 7 years carries a fivefold increased risk, and use for 9 or more years has a 25-fold increased risk.156–158
Hepatocellular adenomas also have been associated with galactosemia, hypothyroidism, polycythemia, diabetes, Fanconi anemia, polycystic ovary syndrome, and the use of anabolic steroids.159–162
Hepatocellular adenomas are a significant complication in patients with type 1A GSD from their teenage years into adulthood.163,164 The estimated prevalence of adenomas in these patients is close to 50%.165,166 The pathogenesis of adenoma development is poorly understood in this group, but may be related in part to the tightness of the metabolic control.167 These adenomas are often multiple rather than solitary lesions. Unfortunately, in this patient population, hepatocellular carcinoma can occur in association with hepatocellular adenomas. The youngest reported patient with GSD was 6 years old at the time of the diagnosis of hepatocellular carcinoma.168 In several series, hepatocellular carcinoma has been found to develop in up to 18% of patients with a hepatocellular adenoma.169–173 Direct evidence for malignant transformation of a hepatocellular adenoma into a carcinoma has been confirmed with the reporting of a hepatocellular carcinoma within a hepatic adenoma in patients with GSD.174 Abnormalities in chromosome 6 have been also been identified in type 1A GSD adenomas and similar chromosome 6 alterations have been identified in hepatocellular carcinomas, suggesting a possible genetic link between these two diagnoses.175
Adenomatosis (the occurrence of more than ten simultaneous adenomas) is a rare disorder, with 38 cases reported in the literature through 2000.176 There is a massive form, characterized by multiple nodules measuring between 2–10 cm, and the multifocal form, in which most lesions are smaller than 1 cm, with only a few larger than 4 cm.177 Oral contraceptive use has been seen in about half of the female patients. Interestingly, diabetes and hepatic steatosis has been noted in these patients, but it is not clear if there is a causative relation.177,178 Adenomatosis has also been reported in patients seven to nine years after a Fontan procedure.179
Histology
Hepatocellular adenomas histologically consist of large plates or cords of cells that resemble normal hepatocytes. These plates are separated by dilated vascular sinusoids, which are equivalent to thin-walled capillaries perfused by arterial pressure. Adenomas do not have a portal venous supply and are fed solely by peripheral arterial vessels that account for the hypervascular nature of these lesions. Kupffer cells are found in reduced numbers and have little or no function. The absence of bile ducts serves as a key histologic feature that helps distinguish the hepatocellular adenoma from FNH. Lipid accumulation is responsible for the characteristic yellow appearance on the cut surface.1
The exact reason for their development is unclear. Two reports have cited the mutations of the Wnt/β-catenin pathway in patients with hepatocellular adenoma.180,181 This pathway mutation has been identified in many hepatocellular neoplasms, although its direct contribution to carcinogenesis is not completely understood. A second mutation has been found in the HNF1A gene that leads to the downregulation of hepatocyte nuclear factor-1α. This downregulation has been linked to the development of hepatic steatosis and hepatic adenomas.182 The significance of these findings in hepatocellular adenoma is also unknown.
Treatment
The treatment approach for these lesions depends on a variety of factors. In patients who are receiving oral contraceptives or androgenic steroid therapy, the first step should be withdrawal of these medications. Multiple case reports mention regression of the adenomas after withdrawal of these compounds. However, in other multiple reports, withdrawal of these agents has resulted in persistence of the adenoma.183–185 If discontinuation is not effective, then the adenoma should be resected. This removes the potential for future hemorrhage or malignant degeneration (10% of lesions).186 If the adenoma is larger than 5 cm or if the diagnosis of the hepatic lesion is uncertain, then excision is recommended.187,188
For patients with ruptured hepatocellular adenomas, the current suggested therapy in the hemodynamically stable patient is nonoperative monitoring and hemodynamic support. Once the hemorrhage has resolved and the patient has recovered, elective resection can be performed. In patients who continue to bleed actively, hepatic arterial embolization should be performed. This not only stops the hemorrhage but also can decrease the size of the adenoma.189 After resolution of the hemorrhage, resection is indicated. This management plan results in a decrease in size of the lesion and allows a more limited hepatic resection under controlled conditions.190,191
Malignant Hepatic Tumors
Hepatoblastoma
Most hepatoblastomas develop before age 3 years, with a median age of about 18 months.192 About 4% are present at the time of birth; 69% are present by the end of two years, and 90% develop by the end of 5 years. Only 3% of cases are noted in children older than 15 years.193 A definite male predominance (1.7 : 1) is seen.5
Epidemiology
Hepatoblastomas are associated with a variety of clinical conditions, syndromes, and malformations (Box 67-1). Beckwith–Wiedemann syndrome is associated most commonly with Wilms tumor, but other tumors such as hepatoblastomas, gonadoblastomas, and adrenal carcinomas are also seen.194,195 The association with hepatoblastoma is so strong that patients with Beckwith–Wiedemann syndrome must be monitored with serial AFP levels every three months until the age of 4 years and an abdominal ultrasound every three months until they reach age 8 years.195–197 Screening studies for hepatoblastoma are also recommended in patients with familial adenomatous polyposis. These patients should be screened for the APC tumor/suppressor gene. If this gene is present, then these patients are at increased risk for developing hepatoblastoma.198,199
Another interesting association exists between hepatoblastoma and extreme prematurity (<1000 g). In the Japanese Children’s Cancer Registry (JCCR), it was noted that hepatoblastomas accounted for 58% of the malignancies diagnosed in extremely low birth weight children.200 In recent epidemiologic studies, several factors were associated with an increased risk for the development of neonatal hepatoblastoma, including birth weight less than 1000 g, maternal age younger than 20 years, use of infertility treatment, maternal smoking, and a higher pre-pregnancy body mass index (BMI of 25–29).201,202 The time from birth to onset of hepatoblastoma in this population ranges from six months to six years.203 Unfortunately, the tumors that occurred in this group grew rapidly and had an unfavorable biologic behavior.204 Although the etiology for the predilection of hepatoblastomas to develop in very low birth weight infants is not known, oxygen therapy, furosemide use, and failure of the infant to grow appropriately were noted to be risk factors.204 The highest correlation was with the duration of oxygen therapy. The risk of hepatoblastoma increased by 20% if oxygen therapy was continued for 30 days, and the risk increased by 100% in children who were treated with oxygen for four months.
Cysteine has also been implicated as a contributing factor. Cysteine is an amino acid that is necessary for the production of glutathione and taurine, both of which are intracellular antioxidants. In premature infant livers, there appears to be impaired production of cysteine.205 Due to the complexities in treating ‘micropremies’ through their first few months, multiple other interventions could influence the development of a hepatoblastoma.
Histology
Hepatoblastomas tend to be unifocal lesions in most cases. Fifty per cent are isolated to the right lobe, 15% are in the left lobe, and 27% are centrally located to involve both lobes (Fig. 67-10).
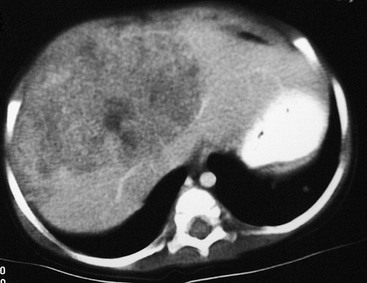
FIGURE 67-10 CT scan after intravenous administration of a contrast agent shows a large right lobe hepatoblastoma extending into the left lateral segment.
Histologically, the tumor can be divided into six different subtypes (Figs 67-11 and 67-12) based on light microscopy (Box 67-2). A correlation between clinical outcome and the histologic subtypes has been suggested. The pure fetal subtype appears to be associated with the better prognosis, whereas the small cell undifferentiated subtype appears to have a very poor prognosis.206–209 In several other studies, chemotherapy was initiated before surgical intervention and likely altered the accuracy of histologic definition of the resected tumor, making it difficult to correlate histology and outcome.210
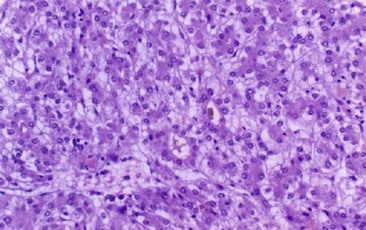
FIGURE 67-11 Histology of a pure fetal hepatoblastoma. Note the hepatocytes have clear glycogen-rich cytoplasm and small, regular nuclei.
Biology and Cytogenetics
Thrombocytosis is common in patients with hepatoblastoma. This may be related to increased thrombopoietin levels, which have been reported in hepatoblastoma cell extracts.210 Elevated interleukin-1b levels also have been noted in hepatoblastoma cell lines.211 This results in an increased production of interleukin-6, which is known to stimulate thrombopoiesis and thrombocytosis.212
Chromosomal abnormalities have been documented in patients with hepatoblastoma.213 The most common defects have been trisomy of chromosomes 20, 2, or 8, or a combination of these. Trisomy 18 also has been found.214 However, to date, no correlation has been noted between these cytogenetic abnormalities and either clinical outcome or tumor biology.
An association between hepatoblastoma and the APC gene was noted in patients with familial adenomatous polyposis and Gardner syndrome.212,215 A recent study found an association between the activation of the Wnt/β-catenin signaling pathway and the development of carcinogenesis in hepatoblastoma and hepatocellular carcinoma.216
Imaging
The first diagnostic test is usually an ultrasound. This usually differentiates between a renal and hepatic mass. An abdominal CT scan is then usually performed. In half of patients, calcification is noted within the mass.217 Spiral CT with an intravenous bolus of a contrast agent not only is helpful in the diagnosis, but also is useful in the staging of the tumor and in determining its resectability. With three-dimensional reconstruction, the location of the mass with respect to the vena cava, the hepatic veins, and the portal venous system can often be precisely delineated (Fig. 67-13). MRI is becoming an increasingly helpful modality for determining the relation of the tumor to the hepatic anatomy and in differentiating hepatoblastomas from other childhood hepatic tumors.218 However, no current noninvasive study can always differentiate between a benign or malignant liver lesion.28 If there is any concern about the diagnosis, a biopsy should be performed.
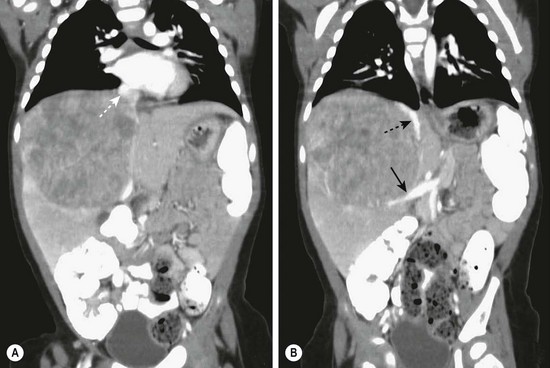
FIGURE 67-13 (A) This CT scan obtained after intravenous administration of a contrast agent in a 1-year-old child shows a large mass in the right hepatic lobe. On other images, the mass appears to invade or compress the medial segment of the left lobe. The middle hepatic vein (dotted arrow) is being compressed by the tumor. (B) The inferior vena cava (dotted arrow) is being displaced medially and anteriorly by the mass, and the portal vein (solid arrow) is markedly displaced inferiorly.
Laboratory Studies
Anemia and thrombocytosis (platelet count >500,000/mm3) are often found in patients with hepatoblastoma.219 However, the hallmark of hepatoblastoma is an elevated AFP level, which occurs in up to 90% of patients.220 The serum levels of AFP can sometimes exceed 1 million ng/mL. This can lead to the ‘hook’ effect in which the initially reported AFP level can be low despite the actual level being very high. If the lesion is suspicious for hepatoblastoma, a request should be made to dilute the AFP sample before retesting.221 Serum AFP has a half-life of between 4 and 9 days, and the levels usually decrease to normal by 4 to 8 weeks after complete removal of the tumor.222 It is important to remember that neonates normally have an elevated AFP level (25–50,000 ng/mL) at birth that does not decrease to ‘adult’ levels until age 6 months.15 This becomes important when evaluating a neonate with a hepatic mass or when monitoring the AFP after liver resection in a neonate or infant.
AFP also has been useful for monitoring purposes. In one case report, a radioimmunodetection method was used (technetium-labeled mouse antihuman monoclonal antibody to AFP).223 After an initial decline in the AFP following liver resection, it began to increase, and an anti-AFP nuclear medicine study accurately located an active tumor in the remaining liver.
Recently, a new marker has been found for hepatoblastoma. Glypican 3 (GPC3) has been detected in hepatic stem cells and has been identified as being expressed by fetal, embryonal, and small cell undifferentiated hepatoblastomas. This marker is also shed by the tumor cells and has the potential to be used as a serum marker for hepatoblastoma.224