Laparoscopic Salpingostomy
Darren M. Lazare
INTRODUCTION
Ectopic pregnancy remains a potentially fatal condition affecting 2% of reported pregnancies and accounting for 9% of all maternal deaths. Etiologic factors relate to distal occlusive tubal disease, resulting either from inflammatory processes, such as endometriosis and pelvic inflammatory disease, or arising from tubal scarring related to previous tubal surgery or prior ectopic pregnancy. The result is a physical barrier to fluid and follicular transport within the tube that can cause hydrosalpinx, infertility, pelvic pain, and ectopic pregnancy.
There have been dramatic improvements in the management of ectopic pregnancy within the last few decades. Ultrasonography has simplified the diagnosis and has allowed earlier diagnosis that often avoids tubal rupture and resulting hemoperitoneum. Equally important is the development of medical treatment regimens that utilize methotrexate. In spite of these advances, there remain circumstances where surgical management is required. Methotrexate is inappropriate for ectopic pregnancies in certain tubal locations or gestations. Surgical treatment is also necessary for up to 10% of patients unsuccessfully treated by methotrexate.
Within the context of surgical management of ectopic pregnancy in hemodynamically stable patients, a laparoscopic approach is superior to laparotomy. Advantages include lesser blood loss, decreased analgesic requirements, shorter duration of hospital stay, quicker return to normal activity, improved cosmesis, and fewer postoperative intra-abdominal adhesions. Outcomes and subsequent pregnancy rates are equivalent to laparotomy. In a review of laparoscopy versus laparotomy in the management of ectopic pregnancy, the rates of subsequent intrauterine pregnancies were 61.0% and 61.4%, and the rates of ectopic pregnancy were 15.5% and 15.4%, respectively. There is conflicting data in the literature regarding persistent ectopic pregnancy in patients managed laparoscopically.
Laparoscopic management can be directed at removing the tube with the gestation, salpingectomy, or removing the gestation and preserving the tube, salpingostomy. Fallopian tube preservation when future fertility is desired remains the primary consideration when performing a salpingostomy. The available evidence does not show different postsurgical pregnancy rates for salpingostomy compared to salpingectomy, although there is a theoretical advantage to maintaining both tubes when possible. There is also no evidence that salpingostomy has a higher rate of persistent ectopic pregnancy or other postsurgical complications, which makes it a viable surgical option for patients requiring surgical management who are seeking preserved fertility.
PREOPERATIVE CONSIDERATIONS
Salpingostomy in the setting of ectopic pregnancy is most often performed as an emergency rather than elective case. As such, preoperative bowel preparation is not possible and also not indicated. There is limited evidence that perioperative antibiotic prophylaxis is
valuable in settings with a high surgical site infection rate. A first-generation cephalosporin is an appropriate choice, and either clindamycin or metronidazole is also an acceptable choice for those allergic to penicillin or cephalosporins. The use of prophylaxis against deep venous thromboembolism should be based on an assessment of risk and should include as risk factors the dorsal lithotomy position and anticipated length of the case as well as patient-specific risks. The patient should be positioned in dorsal lithotomy position with legs in stirrups. General anesthesia is appropriate. A Foley catheter should be placed during the surgery to drain the bladder and may be removed postoperatively once the patient is able to ambulate independently.
valuable in settings with a high surgical site infection rate. A first-generation cephalosporin is an appropriate choice, and either clindamycin or metronidazole is also an acceptable choice for those allergic to penicillin or cephalosporins. The use of prophylaxis against deep venous thromboembolism should be based on an assessment of risk and should include as risk factors the dorsal lithotomy position and anticipated length of the case as well as patient-specific risks. The patient should be positioned in dorsal lithotomy position with legs in stirrups. General anesthesia is appropriate. A Foley catheter should be placed during the surgery to drain the bladder and may be removed postoperatively once the patient is able to ambulate independently.
SURGICAL TECHNIQUE
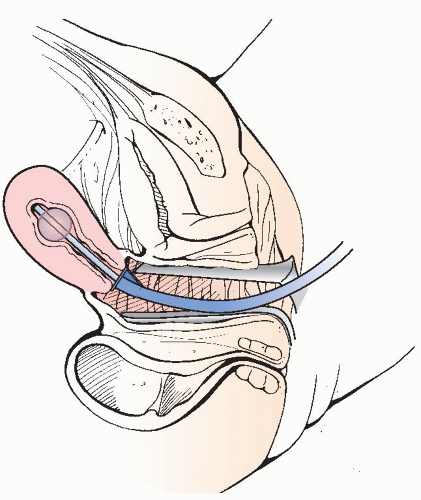
A uterine manipulator facilitates manipulation of the uterus to maximize optimal access to the adnexa laparoscopically. Surgery, therefore, typically begins with the vaginal placement of a uterine manipulator (Figure 6.1).
Upon entry into the peritoneal cavity, the patient is placed in moderate Trendelenburg position to facilitate displacement of the small bowel above the pelvic brim. Careful inspection of the insufflation needle insertion site, upper abdomen, and pelvis may then be performed. The fallopian tube; round and uteroovarian ligaments; and structures of the pelvic sidewall including the ureter, iliac artery, and vein may then be identified. Adequate visualization is often the key determinant to successful laparoscopic surgery. The principle of triangulation also applies whereby the surgeon’s instruments are located at apices that are contralateral to the pathological fallopian tube. We suggest bilateral lower quadrant and an umbilical port for the laparoscope. A suprapubic port or lower quadrant port ipsilateral to the lesion may be added if further retraction by the surgical assistant is required (Figure 6.2).
Initial efforts are directed to assessing bleeding and optimizing the surgical field. An atraumatic grasper such as a laparoscopic Babcock or bowel grasper and suction-irrigator through the lower quadrant ports helps to assess and evacuate the hemoperitoneum. Once the fallopian tube is adequately visualized, it may be gently elevated so as to demonstrate the portion of the tube containing the ectopic pregnancy or hydrosalpinx.
As a means of preventative hemostasis, some surgeons advocate the use of dilute vasopressin solution injected into the mesosalpinx. A typical recipe involves combining 20 IU of vasopressin with 20 to 100 ml of normal saline. A spinal needle inserted directly through the skin or insufflation needle may be used to infiltrate 10 to 20 ml of solution into the avascular peritoneum of the mesosalpinx.
A 1- to 2-cm incision is made over the distended portion of the fallopian tube along the antimesenteric border using monopolar scissors or needle-point cautery (Figure 6.3




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree