Fig. 8.1
Patient positioning for both LSC/RASC: the patient is placed in the dorsal lithotomy position using Yellowfin® (Allen Medical Systems, Acton, MA) stirrups. The arms are tucked at the side. All pressure points are padded. The patient’s breasts should be padded and the patient secured to the table using surgical tape
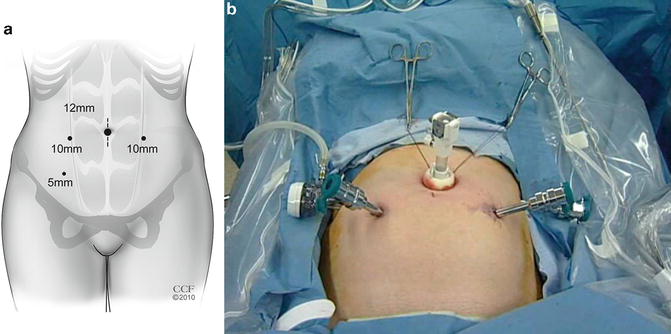
Fig. 8.2
(a) Port placements for laparoscopic pelvic organ prolapse surgery. A fifth port (5 mm) may be placed in the left lower quadrant, or a suture may be used to retract the sigmoid colon. (b) Laparoscopic port placement for robotic pelvic organ prolapse surgery. (a: Reprinted with permission, Cleveland Clinic Center for Medical Art & Photography © 2006–2014. All Rights Reserved)
Two additional 10–12 mm ports are placed lateral to the rectus muscle. One or two additional 5 mm ports are placed 2–3 cm cephalad and 2–3 cm medial to the anterior superior iliac spines, avoiding ilioinguinal and iliohypogastric nerve injury or entrapment. The left lower port is utilized to retract the sigmoid colon to the left and cephalad. This port can be eliminated by using a suture to retract the sigmoid. A 1-0 monofilament suture on a large (CT-X) needle can be passed into the left lower quadrant, through an epiploic appendage of the sigmoid colon, back out through the left lower quadrant, and clamped at the skin level to retract the sigmoid colon (Fig. 8.3).
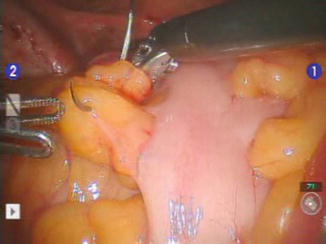
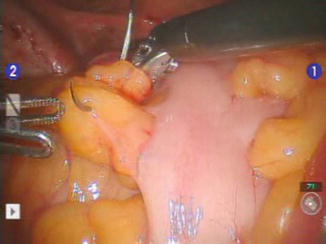
Fig. 8.3
Retraction of the sigmoid colon with a CT-X needle through an epiploic appendage. The needle can be placed though the abdominal wall and clamped at the skin level to retract the sigmoid colon allowing exposure of the sacral promontory
After the sigmoid is retracted, the sacral promontory, right common iliac artery, and right ureter are identified. The posterior peritoneum over the sacral promontory is incised longitudinally to the level of the vaginal apex. An endoanal sizer (Fig. 8.4) is placed in the vagina, thereby reducing the prolapse and elevating the vagina for exposure (Figs. 8.5 and 8.6). The peritoneum over the vaginal apex is then incised, and this dissection is continued anteriorly along the vaginal wall in an attempt to dissect the plane between the bladder and vagina (Figs. 8.7, 8.8, and 8.9). The bladder can be filled to help demarcate this plane. This can also be accomplished with the introduction of a cystoscope light in the bladder. This plane is dissected at least 3 cm distal to the vaginal apex to allow space for placement of the anchoring sutures. The lack of direct tactile feedback makes this dissection challenging; in a recent study of this technique, cystotomy or sutures thrown into the bladder were noted in 10.7 % of cases [6]. Similar dissection is performed on the posterior vaginal wall to de-peritonealize this area and separate the vagina from the rectum posteriorly. The mesh, either in two separate strips (size varies depending on surgeon preference: 2–4 cm × 12–15 cm) or pre-fashioned in a Y-configuration, is passed into the field and sutured with nonabsorbable suture to the posterior and then the anterior vaginal wall (Fig. 8.10). At least four sutures are required on either side to fully anchor the mesh (Fig. 8.11).

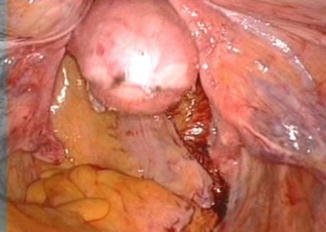
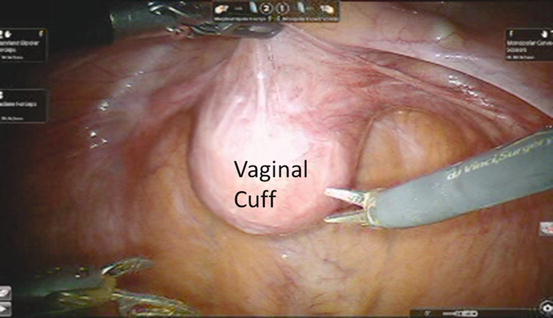
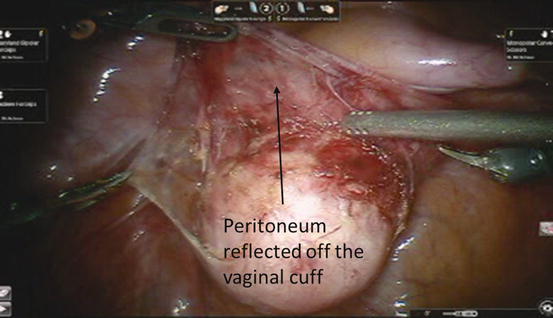

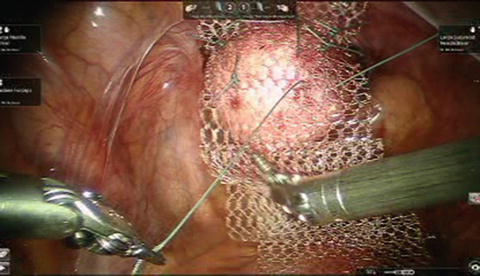

Fig. 8.4
Endoanal sizers (EEA)
Fig. 8.5
Retraction of the small bowel and sigmoid colon allowing exposure of the sacral promontory. (Reprinted with permission, Cleveland Clinic Center for Medical Art & Photography © 2006–2014. All Rights Reserved)
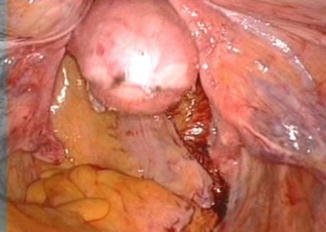
Fig. 8.6
Placement of EEA sizer in the vagina reducing the prolapse and elevating the vagina for exposure
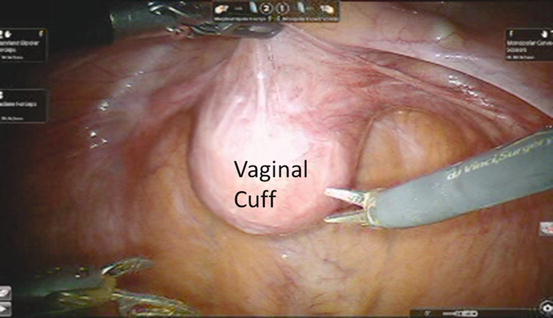
Fig. 8.7
The peritoneum over the vagina apex is incised longitudinally to the level of the sacral promontory. Using the third robotic arm to retract the bladder anteriorly, the peritoneum over the vaginal cuff is exposed. Note the grasper in the left hand and the endoshears in the right hand. (Used with permission of Springer Business + Business Media from McAchran S, Moore C. Robotic Abdominal Sacrocolpopexy. In Best SL, Nakada SY (eds): Minimally Invasive Urology: An Essential Clinical Guide to Endourology, Laparoscopy (LESS), and Robotics. New York: Springer Science + Business Media; 2014)
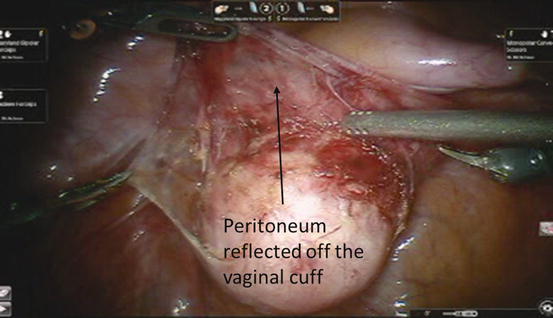
Fig. 8.8
The peritoneum overlying the anterior vagina has been dissected allowing a place to develop between the vagina and the bladder. This will be site for the anterior mesh attachment. (Used with permission of Springer Business + Business Media from McAchran S, Moore C. Robotic Abdominal Sacrocolpopexy. In Best SL, Nakada SY (eds): Minimally Invasive Urology: An Essential Clinical Guide to Endourology, Laparoscopy (LESS), and Robotics. New York: Springer Science + Business Media; 2014)
Fig. 8.9
The peritoneum over the vagina apex is incised longitudinally to the level of the sacral promontory. (Reprinted with permission, Cleveland Clinic Center for Medical Art & Photography © 2006–2014. All Rights Reserved)

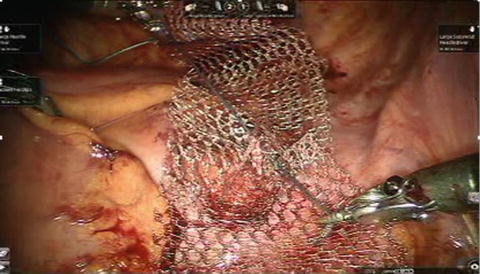
Fig. 8.10
Y-shaped mesh
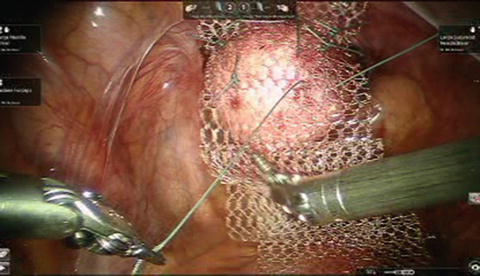
Fig. 8.11
With an EEA sizer in the vagina, the mesh is sutured to the anterior vaginal wall
The next step involves suturing the mesh to the longitudinal ligament of the sacral promontory. Using the third robotic arm the sigmoid colon is retracted to the left pelvic side wall using a bowel grasper or Prograsp™ (Intuitive Surgical, Sunnyvale, CA) exposing the sacral promontory. The peritoneum overlying the promontory is incised using monopolars scissors or hook. Care should be taken to identify the right ureter, iliac bifurcation, and presacral vessels. With careful blunt dissection the fat overlying the promontory is cleared identifying the anterior longitudinal ligament at the S1 or S2 level (Fig. 8.12). This maneuver is frequently done with a laparoscopic Kittner introduced through the 12 mm accessory port which allows tactile feedback of the bone (Fig. 8.13). Should bleeding occur from the presacral space, one can increase insufflation and intrababominal pressure while introducing lap pads to apply direct pressure. In addition sutures, surgical clips, and hemostatic agents can be used. If conversion to open is required, orthopedic thumbtacks can also be used.
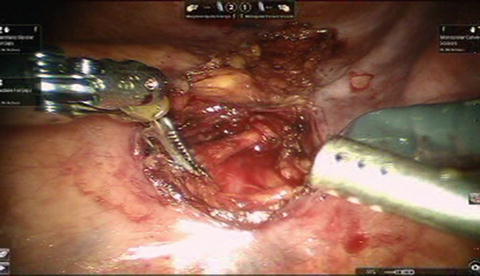

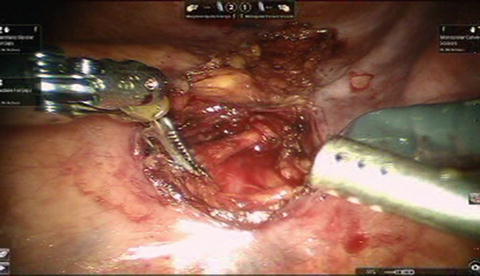
Fig. 8.12
Sacral dissection with the posterior peritoneum incised exposing the anterior longitudinal ligament. (Used with permission of Springer Business + Business Media from McAchran S, Moore C. Robotic Abdominal Sacrocolpopexy. In Best SL, Nakada SY (eds): Minimally Invasive Urology: An Essential Clinical Guide to Endourology, Laparoscopy (LESS), and Robotics. New York: Springer Science + Business Media; 2014)

Fig. 8.13
Fat overlying sacral promontory blunted dissected using laparoscopic Kittner exposing the bone
With the prolapse reduced using the endoanal sizer, the proximal end of the mesh is anchored to the anterior longitudinal ligament of the sacrum with two No. 0 nonabsorbable sutures (Figs. 8.14 and 8.15). The excess mesh is trimmed and the posterior peritoneum is then closed over the mesh (Fig. 8.16). Cystoscopy should be performed at the end of procedure to ensure ureteral patency and that none of the sutures have passed into the bladder.