General Care of the Woman in Labour
Physical Health in Labour
Observations:
The temperature, pulse and blood pressure should be monitored. If abnormal, or the circumstances predispose to abnormalities (e.g. epidural), measurement should be more frequent. Hypotension associated with epidural analgesia will respond to intravenous fluids ± ephedrine; hypertension should be treated as antenatally.
Mobility and Delivery Positions:
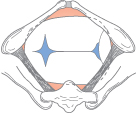
Freedom of movement is encouraged. Most women deliver semi-recumbent: squatting, kneeling or the left-lateral position all increase the dimensions of the pelvic outlet. Pregnant women should not lie flat on their back: the gravid uterus compresses the main blood vessels, reducing cardiac output and causing hypotension, and often fetal distress. This is called aortocaval compression (Fig. 29.2) and in the supine position it is prevented by maintaining at least 15° of left lateral tilt.
Fig. 29.2 Aortocaval compression. If the patient is allowed to lie flat on her back, the inferior vena cava is compressed.

Hydration:
Dehydration in labour is common and women should be encouraged to drink water. Intravenous fluid is also necessary if an epidural is used or if labour is prolonged.
Stomach and Food:
Eating is often discouraged because stomach contents can be aspirated (Mendelson’s syndrome) if a general anaesthetic is required. Ranitidine is often given to reduce the stomach acidity. However, general anaesthesia should rarely be used, and routine starvation of women in labour is inhumane.
Pyrexia in Labour:
This is best defined as >37.5°C. This is associated with an increased risk of neonatal illness and is not always a result of chorioamnionitis (BJOG 2001; 108: 594). It is more common with epidural analgesia and prolonged labour. Cultures of the vagina, urine and blood are taken. Antipyretics are normally administered although it is not known if these are beneficial for the baby; intravenous antibiotics are warranted if the fever reaches 38°C or there are other risk factors for sepsis [→ p.168].
The Urinary Tract:
Neglected retention of urine can irreversibly damage the detrusor muscle [→ p.65]. An epidural usually removes bladder sensation. The woman must be encouraged to micturate frequently in labour; if she has an epidural, catheterization may be needed. Routine catheterization of all, however, is unnecessary.
Mental Health in Labour
The importance of psychological well-being in labour is crucial. The impact of this is seldom remembered but fear and anxiety cause adrenaline secretion and adrenaline slows labour.
Environment:
This need not be too clinical. Resuscitation equipment can be hidden. Music and privacy may help. More women now choose to deliver at home, or in less clinical atmospheres such as birthing centres.
The Birth Attendant:
The continuous presence of a ‘caregiver’ is reassuring. This reduces the length of labour, the use of analgesia, and the augmentation and obstetric intervention (Cochrane 2003: CD003766). Continuous support, explanation and encouragement are needed.
The partner or accompanying person is an important potential source of support for the woman. He/she may need support too.
Control:
Women have differing expectations of labour. Some want labour to be safe, quick and reasonably painless. Others have definite views, either because they view labour as a positive experience rather than a means to an end or because they have preconceptions based on previous or other people’s experiences. They should be encouraged to write their views on a ‘birth plan’, which can be discussed so that expectations are realistic and the woman does not regard deviation from the plan as failure. Most requests in uncomplicated labour can then be safely accommodated, as most labours need little or no intervention.
Progress in Labour: Problems and Their Treatment
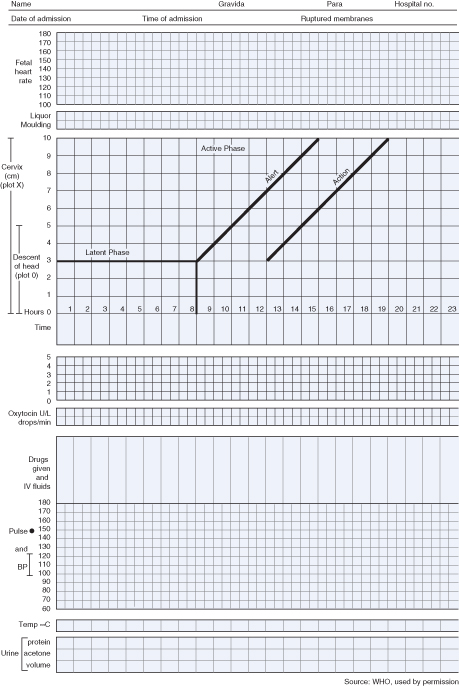
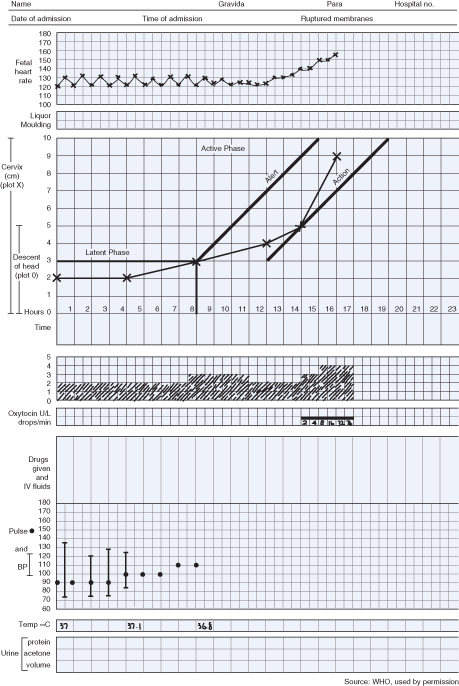
Monitoring Progress: the Partogram
Progress in labour is dependent on the powers, the passage and the passenger. A partogram (Fig. 29.3) is used to record progress in dilatation of the cervix (±descent of the head). This is assessed on vaginal examination and plotted against time. After the latent phase (i.e. at about 3 cm dilated) the usual minimum rate of dilatation is 1 cm/h: ‘alert’ and ‘action’ lines on the partogram indicate slow progress, although debate remains as to exactly where they should be placed. This visual record therefore aids identification of abnormal progress and also forms a record of maternal vital signs, fetal heart rate (FHR) and liquor colour.
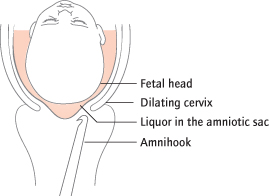
The Powers
‘Inefficient uterine action’ is the most common cause of slow progress in labour. Classifications are meaningless. It is common in nulliparous women and in induced labour, but is rare in multiparous women. Continuous support during labour is associated with a reduction in the length of labour (Cochrane 2003: CD003766), probably because it reduces anxiety. Mobility should also be encouraged. Persistently slow progress is treated by augmentation, initially with amniotomy (Fig. 29.4) and then oxytocin (Fig. 29.5).
Hyperactive uterine action occurs with excessively strong or frequent or prolonged contractions. Fetal distress occurs as placental blood flow is diminished and labour may be very rapid. It is associated with placental abruption, with too much oxytocin, or as a side effect of prostaglandin administration to induce labour. Treatment depends on the cause: if there is no evidence of an abruption, a tocolytic such as salbutamol can be given intravenously or subcutaneously, but Caesarean section is often indicated because of fetal distress.
Nulliparous Labour
The First Stage:
Slow progress in the nulliparous woman is usually due to inefficient uterine action, even if contractions are frequent or feel strong. Strengthening the powers artificially is called augmentation, and this can even sometimes correct passenger problems of attitude or position. This is performed by artificially rupturing the membranes (ARM or amniotomy); if this fails to further cervical dilatation in 1–2 h, artificial oxytocin is administered intravenously as a dilute solution and the dose is gradually increased (Cochrane 2000: CD000015). Provided electronic fetal monitoring is used, this approach is safe because of the relative immunity of the nulliparous uterus to rupture. Oxytocin will usually increase cervical dilatation within 4 h if it is going to be effective. If full dilatation is not imminent within 12–16 h, the diagnosis is reconsidered and Caesarean section is performed: problems with the passage or passenger are more likely and the immunity of the uterus to rupture is diminished.
The Passive Second Stage:
If descent is poor, an oxytocin infusion should be started and pushing delayed by up to 2 h. If an epidural has been used, the urge to push that is characteristic of the active second stage is diminished.
The Active Second Stage:
Pushing need not be directed unless an epidural is present. If the stage lasts longer than 1 h, spontaneous delivery becomes less likely because of maternal exhaustion; fetal hypoxia and maternal trauma are also more common. If the head is distending the perineum, an episiotomy can be performed; if not, traction is often applied to the fetal head with a ventouse or forceps [→ p.270].
Multiparous Labour
The First Stage:
Slow progress in the multiparous woman is unusual. The multiparous uterus is seldom ‘inefficient’ and the pelvic capacity has been ‘proven’ in the previous labour unless delivery has previously been by Caesarean section. The cause is therefore more likely to be the fetal head: its attitude or position, or because it is much bigger than before. In addition, the multiparous uterus is more prone to rupture than the nulliparous uterus. Augmentation of labour with oxytocin must therefore be preceded by careful exclusion of a malpresentation.
The Second Stage:
Instrumental delivery, although rarely needed, requires similar caution.
Augmentation and Induction
Augmentation is the artificial strengthening of contractions in established labour
Induction is the artificial initiation of labour
The Passenger
The fetus can contribute to poor progress in labour.
Occipito-Posterior (OP) Position
This common disorder of rotation [→ p.242] is often combined with varying degrees of extension, and causes a larger diameter to negotiate the pelvic outlet. Labour is often longer and more painful, with backache and an early desire to push. The occiput is palpated posteriorly near the sacrum on vaginal examination (Fig. 29.6). If progress in labour is normal, no action is needed: many fetuses rotate to occipito-anterior (OA) spontaneously or deliver OP. If labour is slow, augmentation is used. If the position is persistent (5% of deliveries), delivery will be ‘face to pubis’ and completed by flexion rather than extension over the perineum. A few do not progress to full dilatation and Caesarean section is required. If associated with a prolonged active second stage, instrumental delivery is usually achievable with rotation to OA position using a ventouse or with manual rotation. Kielland’s forceps [→ p.272], requiring particular expertise, are associated with most success in these circumstances.
Occipito-Transverse (OT) Position
This occurs when normal rotation has been incomplete. The occiput lies on the left or the right, and this is palpated on vaginal examination (Fig. 29.7). This is the position in which the head normally enters the pelvis and is a normal finding in the first stage. Only if vaginal delivery has not been achieved after 1 h of pushing in second stage is the position significant. This is common and usually associated with poor ‘powers’, so rotation with traction is required for delivery to occur: this is usually achieved with the ventouse.
Brow Presentation
This is rare, occurring in 1 in 1000 labours. Extension of the fetal head on the neck (Fig. 28.5) results in a large (13 cm) presenting diameter that will not normally deliver vaginally (Fig. 29.8). The anterior fontanelle, supraorbital ridges and the nose are palpable vaginally. Caesarean section is required.
Face Presentation
This is also rare, occurring in 1 in 400 labours. Complete extension of the head results in the face being the presenting part. Fetal compromise in labour is more common. The mouth, nose and eyes are palpable vaginally. The presenting diameter is 9.5 cm, allowing vaginal delivery in most cases so long as the chin is anterior (mento-anterior position): delivery is completed by flexion over the perineum. If the chin is posterior (mento-posterior position; Fig. 29.9), extension of the head over the perineum is impossible, as it is already maximally extended and Caesarean section is indicated.
Fetal Abnormality
Rarely, abnormalities such as fetal hydrocephalus may obstruct delivery.
Breech presentation and transverse or oblique lie in labour are discussed in Chapter 26.
Common Causes of Failure to Progress in Labour
| Powers: | Inefficient uterine action |
| Passenger: | Fetal size |
| Disorder of rotation, e.g. occipito-transverse (OT), occipito-posterior (OP) | |
| Disorder of flexion, e.g. brow | |
| Passage: | Cephalo-pelvic disproportion |
| Possible role of cervix |
The Passage
Cephalo-Pelvic Disproportion
This implies that the pelvis is simply too small to allow the head to pass through, but it can almost never be diagnosed with certainty. It depends on fetal as well as pelvic size: therefore, although commonly used to describe a person, it is more applicable to a pregnancy. In the absence of a gross pelvic deformity, which is extremely rare in healthy women, it is a retrospective diagnosis best defined as the inability to deliver a particular fetus despite: (i) the presence of adequate uterine activity; and (ii) the absence of a malposition or presentation. The word ‘retrospective’ means that it can normally only be diagnosed after labour has failed to progress and not with any accuracy before labour. Measuring the pelvis clinically or with X-rays or computed tomography (CT) scanning is unhelpful as the pelvis is not completely rigid and the scalp bones can overlap (Fig. 28.7). Cephalo-pelvic disproportion is slightly more likely with large babies, with very short women or where the head in a nulliparous woman remains high at term. Elective Caesarean section is still inappropriate in such women, but the term ‘trial of labour’ is sometimes thoughtlessly used.
Pelvic Variants and Deformities
Normal variants in pelvic shape have been extensively classified but this is virtually never useful in modern practice. The ‘gynaecoid’ or ideal pelvis is found in 50–80% of Caucasian women. The ‘anthropoid’ pelvis (20%) has a narrower inlet, with a transverse diameter often less than the antero-posterior (AP) diameter. The android pelvis (5%) has a heart-shaped inlet and a funnelling shape to the mid-pelvis. In the platypelloid pelvis (10%) the oval shape of the inlet persists within the mid-pelvis.
Abnormal pelvic architecture is usually confined to developing countries where health and nutrition are poor. Rickets and osteomalacia, poorly healed pelvic fractures, spinal abnormalities (such as major degrees of kyphosis or scoliosis), poliomyelitis and congenital malformations are very rare in the West.
Other Pelvic Abnormalities
Rarely, a pelvic mass such as an ovarian tumour or uterine fibroid blocks engagement and descent of the head. This will be palpable vaginally and Caesarean section is indicated.
The Cervix
The role of the cervix is to prevent the fetus from literally dropping out before term. During normal labour, it is not simply the strength of contractions that removes this natural obstruction but a complex mechanism involving hydration of the cervical collagen. The cervix itself, in addition to the contractions, may determine the course of labour, but the clinical relevance of this is poorly understood.
Care of the Fetus
Permanent fetal damage attributable to labour is uncommon: only about 10% of cases of cerebral palsy are attributed solely to intrapartum problems. Nevertheless, fetal death or damage, usually neurological, has devastating effects. There are several causes of damage:
1 Fetal hypoxia, commonly described as ‘distress’, is the best known.
2 Infection/ inflammation in labour, e.g. group B streptococcus [→ p.167].
3 Meconium aspiration leading to chemical pneumonitis.
4 Trauma is rarely spontaneous and more commonly due to obstetric intervention, e.g. forceps.
5 Fetal blood loss [→ p.256].
Fetal Distress and Hypoxia
Definition
The term ‘fetal distress’ is a clinical diagnosis made by indirect methods. It should be defined as hypoxia that might result in fetal damage or death if not reversed or the fetus delivered urgently, but the term is widely abused. In reality hypoxia is simply the best known cause of intrapartum fetal damage and its effects are unpredictable and vary considerably. The convention is that a pH of <7.20 in the fetal scalp (capillary) blood (see below) indicates significant hypoxia.
In reality, the mean cord arterial pH at birth is about 7.22, so a capillary pH of <7.20 will not be uncommon in labour, and conventional practice over-diagnoses fetal distress. Indeed, it is only below 7.00 (Obstet Gynecol 1991; 78: 1103) that neurological damage is considerably more common. Even at this level, most babies have no sequelae; further, most babies with neurological damage had a normal pH at birth. This reflects the influences of other factors, antepartum (e.g. intrauterine growth restriction [IUGR] [→ p.216]) or intrapartum (e.g. maternal fever [→ p.256]) on neonatal outcome.
Aetiology
Why hypoxia occurs is poorly understood. Contractions temporarily reduce placental perfusion and may compress the umbilical cord, so longer labours and those with excessive time (>1 h) spent pushing are more likely to produce hypoxia. Acute hypoxia in labour can be due to placental abruption, hypertonic uterine states and the use of oxytocin, prolapse of the umbilical cord and maternal hypotension.
Epidemiology
Prediction of the ‘at-risk’ fetus is imprecise. Intrapartum risk factors include long labour, meconium, the use of epidurals and oxytocin; antepartum factors include pre-eclampsia and IUGR fetuses. Fetuses with these risk factors are usually monitored in labour with cardiotocography (CTG).
Diagnosing Fetal Distress
As hypoxia is a relatively rare cause of handicap, the effects of attempts to prevent it will be limited. The diagnosis of fetal distress is usually made from the finding of significant fetal acidosis (scalp pH <7.20) or ominous FHR abnormalities. The following are methods employed in the detection of fetal distress.
Colour of the Liquor: Meconium
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree