Chapter 160 Kawasaki Disease
Clinical Manifestations
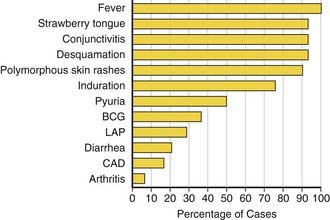
Fever is characteristically high (≥101°F), unremitting, and unresponsive to antibiotics. The duration of fever without treatment is generally 1-2 wk but may persist for 3-4 wk. In addition to fever, the five principal clinical criteria of KD are: bilateral nonexudative bulbar conjunctival injection with limbal sparing; erythema of the oral and pharyngeal mucosa with strawberry tongue and dry, cracked lips; edema and erythema of the hands and feet; rash of various forms (maculopapular, erythema multiforme, or scarlatiniform) with accentuation in the groin area; and nonsuppurative cervical lymphadenopathy, usually unilateral, with node size >1.5 cm (Table 160-1; Figs. 160-1 to 160-4). Perineal desquamation is common in the acute phase. Periungual desquamation of the fingers and toes begins 1-3 wk after the onset of illness and may progress to involve the entire hand and foot (Fig. 160-5).
Table 160-1 CLINICAL AND LABORATORY FEATURES OF KAWASAKI DISEASE
EPIDEMIOLOGIC CASE DEFINITION (CLASSIC CLINICAL CRITERIA)*
OTHER CLINICAL AND LABORATORY FINDINGS
LABORATORY FINDINGS IN ACUTE KAWASAKI DISEASE
* Patients with fever at least 5 days and <4 principal criteria can be diagnosed with Kawasaki disease when coronary artery abnormalities are detected by two-dimensional echocardiography or angiography.
† In the presence of ≥4 principal criteria, Kawasaki disease diagnosis can be made on day 4 of illness. Experienced clinicians who have treated many patients with Kawasaki disease may establish diagnosis before day 4.
‡ See differential diagnosis (Table 160-2).
§ Some infants present with thrombocytopenia and disseminated intravascular coagulation.
From Newburger JW, Takahashi M, Gerber MA, et al: Diagnosis, treatment, and long-term management of Kawasaki disease, Pediatrics 114:1708–1733, 2004.
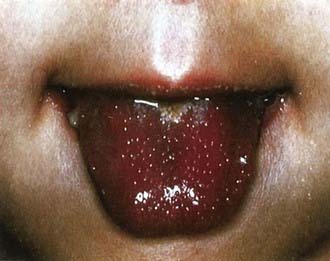
Figure 160-2 Strawberry tongue in mucocutaneous lymph node syndrome (Kawasaki disease).
(Courtesy of Tomisaku Kawasaki, MD.) (From Hurwitz S: Clinical pediatric dermatology, ed 2, Philadelphia, 1993, WB Saunders.)

Figure 160-3 Congestion of bulbar conjunctiva in a patient with mucocutaneous lymph node syndrome (Kawasaki disease).
(Courtesy of Tomisaku Kawasaki, MD.) (From Hurwitz S: Clinical pediatric dermatology, ed 2, Philadelphia, 1993, WB Saunders.)