Chapter 149 Juvenile Idiopathic Arthritis
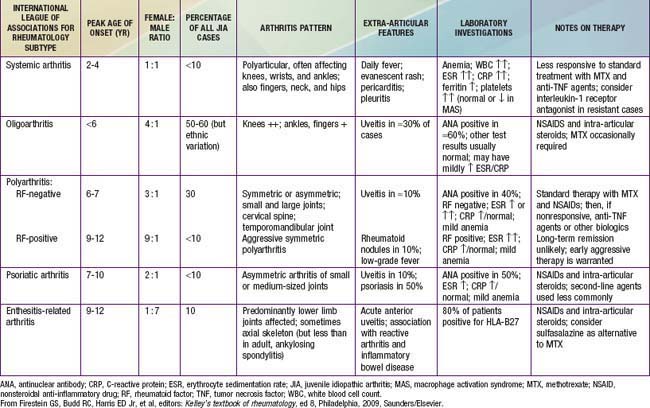
Juvenile idiopathic arthritis (JIA) (formerly juvenile rheumatoid arthritis) is the most common rheumatic disease in children and one of the more common chronic illnesses of childhood. JIA represents a heterogeneous group of disorders all sharing the clinical manifestation of arthritis. The etiology and pathogenesis of JIA are largely unknown, and the genetic component is complex, making clear distinction among various subtypes difficult. As a result, several classification schemas exist, each with its own limitations. In the Classification Criteria of the American College of Rheumatology (ACR), the term juvenile rheumatoid arthritis (JRA) is utilized and categorizes disease into 3 onset types (Table 149-1). Attempting to standardize nomenclature, The International League of Associations for Rheumatology (ILAR) proposed use of a different classification using the term juvenile idiopathic arthritis (JIA) (Table 149-2), which is inclusive of all subtypes of chronic juvenile arthritis. We refer to the ILAR classification criteria; enthesitis-related arthritis and psoriatic JIA are covered in Chapter 150 (Tables 149-3 and 149-4).
Table 149-1 CRITERIA FOR THE CLASSIFICATION OF JUVENILE RHEUMATOID ARTHRITIS
Modified from Cassidy JT, Levison JE, Bass JC, et al: A study of classification criteria for a diagnosis of juvenile rheumatoid arthritis, Arthritis Rheum 29;174–181, 1986.
Table 149-2 CHARACTERISTICS OF THE AMERICAN COLLEGE OF RHEUMATOLOGY (ACR) AND INTERNATIONAL LEAGUE OF ASSOCIATIONS FOR RHEUMATOLOGY (ILAR) CLASSIFICATIONS OF CHILDHOOD CHRONIC ARTHRITIS
| PARAMETER | ACR (1977) | ILAR (1997) |
|---|---|---|
| Term | Juvenile rheumatoid arthritis (JRA) | Juvenile idiopathic arthritis (JIA) |
| Minimum duration | ≥6 wk | ≥6 wk |
| Age at onset | <16 yr | <16 yr |
| ≤4 joints in 1st 6 mo after presentation | • Pauciarticular | |
| >4 joints in 1st 6 mo after presentation | • Polyarticular | |
| Fever, rash, arthritis | • Systemic | • Systemic |
| Other categories included | Exclusion of other forms | |
| Inclusion of psoriatic arthritis, inflammatory bowel disease, ankylosing spondylitis | No (Chapter 150) | Yes |
Table 149-3 INTERNATIONAL LEAGUE OF ASSOCIATIONS FOR RHEUMATOLOGY CLASSIFICATION OF JUVENILE IDIOPATHIC ARTHRITIS (JIA)
| CATEGORY | DEFINITION | EXCLUSIONS |
|---|---|---|
| Systemic-onset JIA | Arthritis in ≥1 joints with, or preceded by, fever of at least 2 wk in duration that is documented to be daily (“quotidian”*) for at least 3 days and accompanied by ≥1 of the following: | c Ankylosing spondylitis, enthesitis-related arthritis, sacroiliitis with inflammatory bowel disease, Reiter syndrome, or acute anterior uveitis, or a history of one of these disorders in a 1st-degree relative. |
| Oligoarticular JIA | ||
| Polyarthritis (RF-negative) | Arthritis affecting ≥5 joints during the 1st 6 mo of disease; a test for RF is negative. | a, b, c, d, e |
| Polyarthritis (RF-positive) | Arthritis affecting ≥5 joints during the 1st 6 mo of disease; ≥2 tests for RF at least 3 mo apart during the 1st 6 mo of disease are positive. | a, b, c ,e |
| Psoriatic arthritis | Arthritis and psoriasis, or arthritis and at least 2 of the following: | b, c, d, e |
| 1. Dactylitis.‡ | ||
| 2. Nail pitting§ and onycholysis. | ||
| 3. Psoriasis in a 1st-degree relative. | ||
| Enthesitis-related arthritis | Arthritis and enthesitis,| or arthritis or enthesitis with at least 2 of the following: | a, d, e |
1 Presence of or a history of sacroiliac joint tenderness or inflammatory lumbosacral pain or both.¶ | ||
| Undifferentiated arthritis | Arthritis that fulfills criteria in no category or in ≥2 of the above categories. |
RF, rheumatoid factor.
* Quotidian fever is defined as a fever that rises to 39°C once a day and returns to 37°C between fever peaks.
† Serositis refers to pericarditis, pleuritis, or peritonitis, or some combination of the three.
‡ Dactylitis is swelling of ≥1 digits, usually in an asymmetric distribution, that extends beyond the joint margin.
§ A minimum of 2 pits on any one or more nails at any time.
| Enthesitis is defined as tenderness at the insertion of a tendon, ligament, joint capsule, or fascia to bone.
¶ Inflammatory lumbosacral pain refers to lumbosacral pain at rest with morning stiffness that improves on movement.
From Firestein GS, Budd RC, Harris ED Jr, et al, editors: Kelley’s textbook of rheumatology, ed 8, Philadelphia, 2009, Saunders/Elsevier.
Pathogenesis
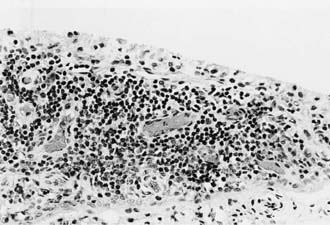
All these immunologic abnormalities cause inflammatory synovitis, characterized pathologically by villous hypertrophy and hyperplasia with hyperemia and edema of the synovial tissue. Vascular endothelial hyperplasia is prominent and is characterized by infiltration of mononuclear and plasma cells with a predominance of T lymphocytes (Fig. 149-1). Advanced and uncontrolled disease leads to pannus formation and progressive erosion of articular cartilage and contiguous bone (Figs. 149-2 and 149-3).

Figure 149-3 MRI with gadolinium of a 10 yr old child with juvenile rheumatoid arthritis (same patient as in Fig. 149-1). The dense white signal in the synovium near the distal femur, proximal tibia, and patella reflects inflammation. MRI of the knee is useful to exclude ligamentous injury, chondromalacia of the patella, and tumor.
Clinical Manifestations
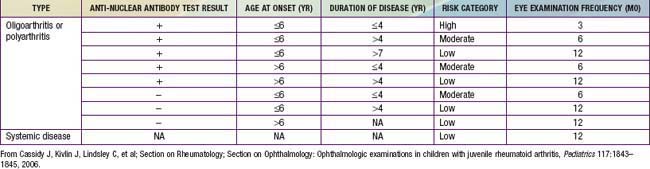
Oligoarthritis is defined as involving ≤4 joints within the first 6 mo of disease onset, predominantly affecting the large joints of the lower extremities, such as the knees and ankles (Fig. 149-4). Often only a single joint is involved. Isolated involvement of upper extremity large joints is less common. Those in whom disease never develops in more than 4 joints are regarded as having persistent oligoarticular JIA, whereas evolution of disease in more than 4 joints over time changes the classification to extended oligoarticular JIA. The latter often portends a worse prognosis. Involvement of the hip is almost never a presenting sign and suggests a spondyloarthropathy (Chapter 150) or nonrheumatologic cause. The presence of a positive antinuclear antibody (ANA) test result confers increased risk for asymptomatic anterior uveitis, requiring periodic slit-lamp examination (Table 149-5).

Figure 149-4 Oligoarticular juvenile idiopathic arthritis with swelling and flexion contracture of the right knee.
Polyarthritis (polyarticular disease) is characterized by inflammation of ≥5 joints in both upper and lower extremities (Figs. 149-5 and 149-6). When rheumatoid factor (RF) is present, polyarticular disease resembles the characteristic symmetric presentation of adult rheumatoid arthritis. Rheumatoid nodules
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree